INTRODUCTIONAdenotonsillectomy on pediatric patients has still been a questionable surgical procedure by professionals due to its postoperative results (2), even being the most common procedure among these patients (6). Tonsils represent the first defense of the upper airways (10) and also the possible surgery complications; the concern about their immunological role explains all the care when selecting patients (3). The enlargement of the palatine tonsils and adenoids is one the most common problems in the ENT services (1); it is responsible for several alteration on children's development and behavior, what worries parents or guardians.
Tonsil hypertrophy is the main cause of upper airway obstruction and of Obstructive Sleep Apnea Syndrome in children (2), causing several damages to them. Disorders such as apnea, disturbed sleep and night snoring can cause alterations on sleeping process. These alterations affect the efficiency of everyday activities on children's life due to tiredness, day sleepiness and emotional discomfort as irritability and impatience (4). For all those reasons, sleeping disorders have been, in the past 20 years, the main recommendation for adenotonsillectomy in pediatric patients, exceeding chronic infections (11).
Mouth respiration is another common alteration on children with Adenotonsillar Hypertrophy (AH). Due to this, alterations develop on the dentocranial skeleton and dental malocclusion and Gothic palate are the most common of them. Still, speech, mastication and deglutition alterations and nocturnal enuresis, day sleepiness, low appetite, adynamia and learning deficit are also common symptoms, which were already mentioned by other authors (5).
Pulmonary hypertension and cor pulmonalle are, less common, but, more severe occurrences. They are considered long-term alterations from AH (6).
Because children with AH are clearly affected on their everyday activities due to the disease effect, the target of this study is to make a comparison between pre- and postoperative signs and symptoms, by showing the results from adenotonsillectomy on these patients' quality of life.
MATERIAL AND METHODSIt was selected 100 patients aging from 1 to 16 years. They searched the ENT department of the Universidade Federal do Paraná complaining of obstructive symptoms and others that were related to hypertrophy of the palatine tonsils and adenoids with adenotonsillectomy recommendation.
Parents and guardians were applied a questionnaire based on the study by Serres et al. in 2000 that was also used by Di Francesco et al. in 2004. The questionnaire referred to the symptoms and effects related to the disease previously to surgery (in the last medical visit before surgery) and the 5-month postoperative follow-up. The questionnaire was not necessarily applied by the same team which performed surgery.
The prospective study followed the principles from the Research Ethics Committee belonging to the institution. It was approved in May 2007, under the protocol 1344.009-2007/01 by the Human Research Ethics Committee of the Hospital de Clínicas da Universidade Federal do Paraná.
Patients were also evaluated regarding adenoid size, which was classified from I to IV according to the traditional evaluation of lateral cranial radiography.
All patients were submitted to adenotonsillectomy and, 5 months after surgery, were reexamined regarding symptoms and effects related to the disease, after having answered the same questionnaire applied to parents/guardians.
The questionnaire follows.
RESULTSOut of the 100 patients who were evaluated, 47 were females and 53 males.
Among the achieved results, we could notice an expressive improvement, confirmed through the statistical validation (p < 0.05) by the Student's t-test, when analyzing signs and symptoms of patients according to the questionnaire.
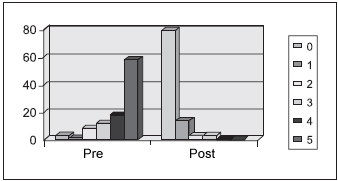
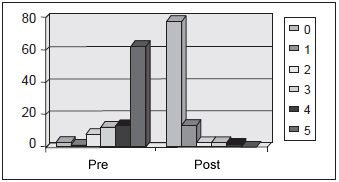
Regarding tonsils degree during the preoperative period, 41 (80%) patients were classified as having Adenoid III and 39 patients with Adenoid IV. Yet, Palatine Tonsils analysis, presented 38 patients (69%) with obstruction III and 31 patients with obstruction IV (Pictures 1 and 2).
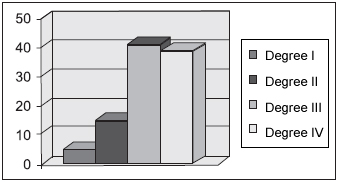
Picture 1. Pharyngeal tonsil - Percentage of distribution of pharyngeal tonsils according to its size grading
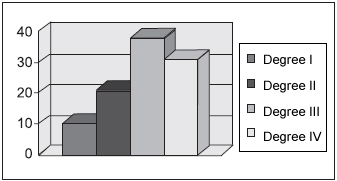
Picture 2. Palatine tonsil - percentage of distribution of Palatine Tonsils according to its size grading
When patients were examined regarding physical discomfort, 98% of patients were affected by nasal obstruction symptom before surgery. From the 100 family member who were interviewed, 51% classified nasal obstruction in children as 5 (which could not be worse). In the postoperative evaluation, 49% of the interviewed people reported that patients had not been affected by nasal obstruction (0 - never).
Low weight (46%) and day fatigue (53%) were also highlighted by parents/guardians and children were classified as 5. However, 79% of parents reported no more occurrences of those symptoms after surgery. (Pictures 3 and 4).
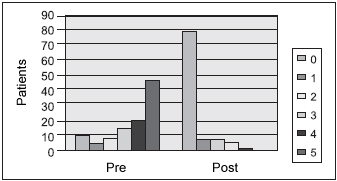
Picture 3. Low weight - incidence of low weight evaluated before and after the surgery
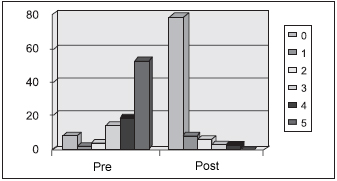
Picture 4. Day fatigue - Incidence of day fatigue in patients evaluated
Analyzing sleep disorders resulting from the pathology, 100% of patients reported night snoring before surgery; 53 patients from those were evaluated as 5 (could not be worse) and 31 were classified as 4 (very often). The evaluation after surgery showed 38% of patients presenting snoring occurrences; and 23 from those were classified as 1 (almost never), 11 patients were classified as 2 (sometimes) and only 4 patients remained with often snoring (3).
Difficulty in waking up in the morning symptoms was reported by 100% of patients; 43 from these were classified as 5 (could not be worse) and 16 were classified as 4 (very often). The after-surgery analysis showed a 98% improvement on patients.
Difficulty in swallowing solid food or chocking was reported as a severe degree by 48% of parents; and 69% reported a significant statistical improvement in 5 months after surgery (Picture 5).
Picture 5. Ingestion of solid food - The difficulty in swallowing solid food or the presence of choking in the evaluated population
Irritability and impatience symptoms were considered severe in 53% of the evaluated children; and moderate in 17% of them. It was noticed a significant statistical improvement in 68% of the cases after surgery (Picture 6).
Picture 6. Impatience - observation of irritability/impatience in the patients evaluated
School development was considered unsatisfactory by 55% of parents. However, there was an improvement in 76% of the children 5 months after surgery.
When children were evaluated on performing everyday activities, 53% of parents reported unsatisfactory behavior. However, there was also an improvement in 75% of the cases after surgery.
Regarding concern about signs and symptoms of their children, 61% of parents reported that their concern could not be worse; and 75% of them report no worries after surgery.
DISCUSSION The presence of tonsil and adenoid hypertrophy; sleeping apnea syndrome; infections resulting from tonsils; otitis media (recidivous acute, chronic or secretive) and rhinosinusitis are considered indications for adenotonsillectomy (12).
Among all conditions that show an involvement of AH on children's development, the low weight is one of the main concerns for parents. Low caloric ingestion can be related to different factors such as nasal obstruction caused by the presence of tonsil hypertrophy, the presence of chocking and asphyxiation and also emotional discomfort. Factors as hypoxemia and nocturnal respiratory acidosis, which are involved in the presence of AH, lead to an increase on respiratory activity, what also contributes to low weight. Another cause for that, mentioned by other authors, is the deficient secretion of GH (Growth hormone) (7) and a failure in its action. Despite, the origin of low weight condition is still unknown (8).
Marcus et al. showed that, after surgery, the weight gain on children becomes related to the energy loss during sleeping time, by displaying that the increase on respiratory activity due to nocturnal respiratory acidosis, hypoxemia and to period of apnea might be the causes of low weight. Many other scientific articles confirm the weight gain process on children submitted to adenotonsillectomy (7,8). These results agree on positive findings demonstrated by parents and guardians, who were interviewed, in relation to the weight gain of their children, by reporting that 79% of the children did not lose weight 5 months after surgery.
Another factor, still related to the development of children with AH, is growth, which is of endogenous feature and a more preoccupying issue (7,8). Alterations on growth when observed by a pediatrician must be researched and associated to other signs and symptoms, such as emotional, sleeping, speech and deglutition disorders, by helping on diagnosing and proper intervention (7).
The GH, the hormone that is intensively produced by hypophysis, mainly during the slow-wave sleep (7), is one of the hormones that have higher relation with growth activity in the postnatal period (9). GH operates through the activation of the Insulin-like Growth Factors (IGF), and the IGF-1 is the most important one during this period (7,9) and also the main mediator of the growing development actions of the GH (8). These ones, for being connected to specific receivers, activate second messengers which work on the cellular nucleus, causing then effects on growing (9). Another factor produced through GH stimulus is the Insulin-like Growth Factor Binding Protein-3 (IGFBP3) (7-9). This factor is the main IGF-1 path and also is responsible for its life extension (8). GH secretion is involved in children with AH and who are affected by sleeping disorders caused by irregular respiratory standard such as sleeping apnea. These children own looseness on the air passages during REM sleep; if REM sleep is associated to palatine tonsils and adenoids, it causes sleeping apnea and later awakening in order to recover respiration (13), what has a negative effect on growth. Besides, IGF-1 has been reduced in cases of malnutrition, what can be related to low weight, as mentioned before, affecting most of these children (9).
Adenotonsillar Hypertrophy is associated to many children with sleeping disorder that may vary from obstructive disorders, leading to snoring, up to Obstructive Sleep Apnea Syndrome (17). Besides AH, there are other conditions that lead to this syndrome, such as infant severe obesity, craniofacial syndromes, metabolic and cardiopulmonary disorders and even neuromuscular disease.
When evaluating a child with suggestive history of Obstructive Sleep Apnea Syndrome, it is necessary firstly to evaluate the presence of Adenotonsillar Hypertrophy. If its presence is confirmed, the submission to an examination by an ENT doctor is mandatory in order to a possible adenotonsillectomy. If there is no sign of AH, other causes of OSAS must be questioned. In case of any comorbity, this child must be forwarded to a polissonography study. If it is positive, the child must be forwarded to a specialist to treat the related comorbity, besides evaluating for a possible use of CPAP (Continuous Positive Airway Pressure). In cases in which no other comorbity is related to OSAS or the polissonography study of such child is negative, even so such patient must be forwarded to an otorhinolaryngologist to have airways evaluated (14).
It is important that snoring is not forgotten. Snores caused by small obstructive disorders must not be considered benign. The presence of snoring is related to children with reduced neurocognitive performances, attention, memory and intelligence disorder (18). Parents usually search for medical attention when they are disturbed by the night respiratory difficulties, while behavioral, emotional and neurocognitive difficulties are less considered (15), even if they are mentioned by parents or guardians (14).
During last years, behavioral, emotional and neurocognitive repercussions related to sleep disorders, more precisely the OSAS, have been evaluated in several series comparing pre- and postoperative phases of patients who underwent Adenotonsillectomy through different protocols such as OSA-18 (15,16,18), BASC (The Behavioral Assessment System for Children) (14) and CBCL (The Child Behavior Checklist) (15) e OSD-6(17). Even when different protocols are used, the results concerning the improvement of behavior and children's quality of life who underwent such surgery is, generally, mentioned in all series being effective both in 1-month follow-up up to 18-month follow up after the surgery (14-18).
In Mitchell et al. there are some parameters such as hyperactivity, attention and concentration, parents' concern and frustrations with children who do not demonstrate improvement after the surgery. On the other hand, in Mitchell and Kelly, the abnormalities reported by parents with somatization, hypersensitiveness to small discomforts, hyperactivity, aggression, presence of atipicity and depression were smaller after the surgery, being kept for a long time after it. The number of children with behavior disorders was statistically lower and statistically significant after the surgery. Such results agree with the results obtained in this study based on the application of the questionnaire obtained from Serres et al. The improvement of all behavior disorders evaluated such as impatience, irritability and lack of attention was observed according to evaluation done 5 months after the surgery.
CONCLUSION The results demonstrated based on the evaluation of children with AH in the pre and 5-month postoperative show that the adenotonsillectomy is efficient, and is the best way to improve the patients' quality of life.
The application of a questionnaire like that shows the satisfaction of parents and guardians regarding the results of the surgery, providing the doctors with the guarantee of effectiveness of the treatment performed.
BIBLIOGRAPHY1. Chen Y, Rennie DC, Lockinger LA, Dosman JA. Effect of environmental tobacco smoke on cough in childrem with a history of tonsillectomy or adenoidectomy. Eur Respir J. 1998, 11:1319-1323.
2. Avelino M, Pereira F, Carlini D, Moreira G, Fujita R, Weckz L. Avaliação polissonográfica da síndrome da apnéia obstrutiva do sono em crianças, antes e após adenoamigdalectomia. Rev Bras Otorrinolaringol. 2002, 68(3):308-311.
3. Lourenço E, Lopes K, Pontes Júnior A, Oliveira MH, Umemura A, Vargas AL. Estudo comparativo e nasofibroscópico do volume adenoideano em crianças respiradoras bucais. Rev Bras Otorrinolaringol. 2005, 71(1):23-28.
4. Di Franceso R, Fortes F, Komatsu C. Melhora da qualidade de vida em crianças pós-amigdalectomia. Rev Bras Otorrinolaringol, 2004, 70(6):748-751.
5. Di Francesco R, Passerotii G, Paulucci B, Miniti A. Respiração oral na criança: repercussões diferentes de acordo com o diagnóstico. Rev Bras de Otorrinolaringol. 2004, 70(5):665-670.
6. Sebusiani B, Pignatari S, Armínio G, Mekhitarian Neto L, Stamm A. Hipertensão Pulmonar em pacientes com hipertrofia adenoamigdaliana. Rev Bras Otorrinolaringol. 2003, 69(6):819-823.
7. Di Franceso R, Junqueira P, Frizzarini R, Zerati FE. Crescimento pondero-estatural de crianças pós adenomigdalectomia. Rev Bras Otorrinolaringol. 2003, 69(2):193-196.
8. Ersoy B, Yücetürk A, Taneli F, Ürk V, Uyanik B. Changes in growth pattern, body composition and biochemical markers of growth after adenotonsillectomy in prepubertal children. International Journal of Pediatric Otorhinolaryngology. 2005, 69:1175-1181.
9. Behrman R, Kliegman R. Nelson Princípios de Pediatria, Quarta Edição, Editora Guanabara Koogan; 2004, pp. 650-653.
10. Weil-Olivier C, Sterkers G, François M, Garnier J M, Reinert P, Cohen R. L'Amigdalectomie en 2005. Archives de Pédiatrie. 2006, 13:168-174.
11. Derkay C, Darrow D, Welch C, Sinacori J. Post-Tonsillectomy Morbidity and Quality of Life in Pediatric Patients with Obstructive Tonsils and Adenoid: Microdebrider vs Eletrocautery. Otolaryngology - Head and Neck Surgery. 2006, 134:114-120.
12. Escario J, Martín Del Castillo F, Campderá J, Grãs Albert J, Pérez Piñero B, Villafruela Sanz M. Indicaciones de Adenoidectomía y Amigdalectomía: Documento de Consenso ente la Sociedad Española de Otorrinolaringologia y Patologia Cervicofacial y la Asociación Española de Pediatria. Acta Otorrinolaringol Esp. 2006, 57:59-65.
13. Shine NP, Coates H, Lannigan F. Obstructive Sleep Apnea, Mobid Obesity and Adenotonsillar Surgery: A Review of the Literature. International Journal of Pediatrc Otorhinolaringology. 2005, 69:1475-1482.
14. Mitchell R, Kelly J. Long-Term Changes in Behavior After Adenotonsillectomy for Obstructive Sleep Apnea Syndrome in Children. Otolaryngology - Head and Neck Surgery. 2006, 134:374-378.
15. Goldstein N, Fatima M, Campbell T, Rosenfeld R. Child Behavior and Quality of life Before and After Tonsillectomy and Adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002,128:770-775.
16. Mitchell R, Kelly J, Call E, Yao N. Long-Term Changes in Quality of Life After Surgery for Pediatric Obstructive Sleep Apnea. Arch Otolaryngol Head Neck Surg. 2004, Apr,130(4):409-12.
17. de Serres L, Derkay C, Sie K, Biavati M, Jones J, Tunkel D, Manning S, Inglis A, Haddad J, Tampakopoulou D, Weinberg A. Impact of Adenotonsillectomy on Quality of Life in Children with Obstructive Sleep Disorders. Arch Otolaryngol Head Neck Surg. 2002,128:489-496.
18. Mitchell R, Kelly J. Quality of Life after Adenotonsillectomy for SDB in Children. Otolaryngology - Head and Neck Surgery. 2005, 133:569-572.
1. Otorrhinolaryngology Professor of Otorhinolaryngology of the Hospital de Clínicas da Universidade Federal do Paraná.
2. Physician of the Pediatric Otorhinolryngology Division of the Otorhinolaryngology Department of the Hospital de Clínicas da Universidade Federal do Paraná.
3.Otorhinolaryngology Physician.
4. Graduated doctor by Universidade Federal do Paraná.
5. PhD and Professor of the Otorhinolaryngology Discipline at UFPR. (Head of the Otorhinolaryngology service of the Hospital de Clínicas da Faculdade de Medicina da Universidade Federal do Paraná).
Universidade Federal do Paraná - UFPR
Andrea Thomaz Soccol
Mail Address:
Rua General Carneiro, 181, 5º andar Anexo B
Curitiba / PR - CEP 80060-900
Phone: (41) 3360-1800. E-mail: andreasoccol@yahoo.com.br
This article was submitted to SGP (Sistema de Gestão de Publicações) of R@IO on October 24th, 2007 and approved on June 22nd, 2007 at 22:23:38.