INTRODUCTIONThe granulomatous diseases are affections characterized by the presence of the granuloma, a result from the organism defense and wound healing process. It can be classified in two types: specific (hanseniasis, leishmaniasis and tuberculosis) and non-specific (Wegener's granulomatosis and sarcoidosis) (1).
In some Brazilian regions the infectious diseases are frequent, with specific granuloma, such as hanseniasis, cutaneo-mucous leishmaniasis, tuberculosis and (PCM) paracoccidioidomycosis. This relates to the social environment where these patients live, with strong poverty and consequent people's undernutrition, household agglomeration and more concomitant diseases, which allows for a major dissemination of such diseases (2).
The otorhinolaryngological clinical manifestations that may be found in these diseases are the nasal crusts, nasal obstruction, septal perforations, laryngeal or oral vegetative lesions, mucous ulcers, cervical lymph adenomegalias and otorrhoea (3). The head and neck predominant mucous manifestations vary according to the etiological agent:
Hanseniasis, for instance, caused by
Mycobacterium leprae, frequently affects the nasal cavities mucous, irrespectively of the clinical form, even before the appearing of lesion on the skin or other parts of the body, whether or not in the presence of clinical complaints. Mucosa infiltrations, lepromas, ulcerations and septal perforation may appear (4, 5).
Leishmaniasis with mucous affection is a form of tegumentary leishmaniasis relating to the
L. braziliensis, L. panamensis and less frequently to the
L. amazonensis. The nasal mucosa is the favorite place for lesions and the consequence is nasal obstruction, epistaxis, frontal nasal septum granuloma and later nasal septum perforation and drop of the nasal tip. Other places affected by frequency order are the pharynx - edematous infiltration, granulation and fibrosis - and the larynx - granuloma leading to dysphonia (6, 7, 8, 9, 10).
As for otorhinolaryngological manifestations, the oropharyngeal lesions of ulcerovegetative aspect and laryngeal and labial deformities are remarkable in the paracoccidioidomycosis, caused by Paracoccidioides brasiliensis (11, 12).
However, despite their importance, there are a few studies approaching the granulomatous diseases otorhinolaryngological manifestations, as happens for example with hanseniasis (4, 13).
The purpose of this study is exactly verify the clinical frequency of head and neck manifestations provoked by paracoccidioidomycosis, hanseniasis and leishmaniasis to the oral, nasal, otologic, pharyngeal and laryngeal regions.
METHODRetrospective research of the records of patients with such diseases, in the period of January 2005 through October 2007, in the infectology service of a tertiary hospital. All patients with other diseases that could lead to affection of the head and neck were excluded. The patients with concomitant diagnosis of paracoccidioidomycosis and tuberculosis were also excluded.
The diagnosis of each disease was confirmed by sorology or the lesions biopsy. Leishmaniasis was also diagnosed by the Montenegro's test.
RESULTS142 patients were evaluated with the following diseases: leishmaniasis (93 cases), paracoccidioidomycosis (39 cases) and hanseniasis (10 cases).
Out of 93 patients with leishmaniasis, 20 (21.5%) presented head and neck manifestations. From these, 16 patients (17.2%) had mucous affection. In the individuals with paracoccidioidomycosis, 25 cases (64.1%) with such type of lesion and in hanseniasis no one had mucous affection. The most common mucous symptoms and signs found in leishmaniasis were septal perforation and nasal mucosa ulcer, both with 8 cases (50% of the mucous affection each), followed by epistaxis with 5 cases (31.2% of the mucous manifestations). In the PCM, the ulcerated lesion of the oropharyngeal region was found in 60% of the cases with mucous lesion. In the 10 cases evaluated with hanseniasis only two presented head and neck affection, 1 with lesion in the external ear and 1 with lip nodular lesion.
The distribution of mucous lesion places in the leishmaniasis and paracoccidioidomycosis present a predominance of nasal lesions in the leishmaniasis (81%) (Chart 1) and oropharyngeal lesions in the paracoccidioidomycosis (72%) (Chart 2).
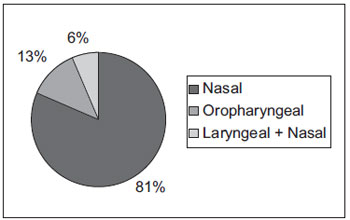
Chart 1. Percentage of the mucous lesion place in Leishmaniasis.
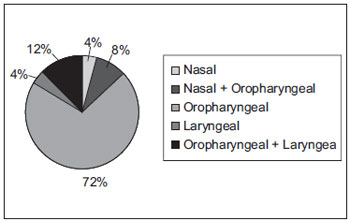
Chart 2. Percentage of the lesion place in Paracoccidioidomycosis.
The large percentage of head and neck affection of these granulomatous diseases, such as, for example, 21.5% of the patients with leishmaniasis evaluated reflect the importance of such affections for the otorhinolaryngologist. We should also take into account that this value could be major if these patients had been submitted to nasal and laryngeal endoscopy.
In their study of endoscopic evaluation of patients with hanseniasis, Martins et al (4) found nasal mucosa changes in all 173 patients evaluated (100%). A percentage close to that of Martins was found by Barton et al (5): 95% with early lesion of the nasal mucosa in patients with hanseniasis in forms LL (Virchovian form) and BL (multibacillary). Nasal complaints were also frequent according to Silva et al (13). In our study, cervico-facial signs were found in only 2 to 10 patients evaluated (20%), and none of them was a mucous sign or symptom. Such difference shows the need for nasal endoscopic evaluation of all patients with this affection, which was not performed in this research.
By evaluating 853 patients with American Tegumentary Leishmaniasis in an endemic zone in the Southeast of Bahia, Barreto et al (6) observed that 67% of the patients had some cutaneous lesions, while 33% had mucous or cutaneo-mucous lesions. We confirmed that out of 93 patients with leishmaniasis evaluated, 82.8% had the isolated cutaneous form and 17.2% had mucous affection.
The mucous leishmaniasis is caused mainly by
L. braziliensis and
L. panamensis, and the nasal mucosa is the most impacted part (7). Within the nasal affection, the most common symptoms and signs were septal perforation (50%), the ulcer to nasal mucosa (50%) and epistaxis (31.2%). A similar percentage was found by Carvalho and Dolci (8) with evaluation of 41 records of patients with diagnosis of nasal leishmaniasis they observed the nasal obstruction, nasal crusts and epistaxis were the most common initial symptoms. They found septal perforation in 26 patients (63.4%).
In 35 patients observed by Falqueto and Sessa (9) with the cutaneo-mucous form, 25 had nasal lesions (71.5%). In our casuistics, that includes the cases with the cutaneo-mucous form and with isolated mucous form, 15 cases (93.7%) had nasal lesions.
The nose was the place of major prevalence of manifestations, probably because it is a temperature region where the macrophage has minor phagocytosis capacity (9).
In another review by Sessa (10) with 118 patients with leishmaniasis relating to mucous affection, 97 (82%) presented exclusively nasal lesions, and in 45 (37%) there was destruction of the septum in a variable level. In 14 (12%) there was association of nasal lesions with other oropharyngeal, larynx and mouth lesions; only in 8 patients (7%) there was no nasal lesion. In our study, only one patient with mucous affection did not present nasal lesion (6.2%) and 14 had exclusively nasal lesion (81.2%).
As to the PCM, 25 autopsies carried out and 173 patients serviced by Franco et al (11), affected by
Paracoccidioides brasiliensis, confirmed that 60% of the autopsies and 48% of the patients had mucous affection in the upper airways. Out of our 39 patients with paracoccidioidomycosis, 25 (64.1%) has the same affection. From these, 23 (92%) had oropharyngeal manifestation, a figure that helps to confirm this region as the one of the most frequent signs and symptoms of the upper airways in the paracoccidioidomycosis.
The statement of head and neck symptoms and signs in patients with leishmaniasis, paracoccidioidomycosis and hanseniasis remark the need for all of them undergo an otorhinolaryngological evaluation. In addition to these diseases, it would be an adequate procedure to carry out a full otorhinolaryngological evaluation in all the patients with some type of granulomatous disease.
We emphasize the need for studies of these affections and a full otorhinolaryngological evaluation in these patients, even where there is no complaint.
CONCLUSIONHead and neck signs and symptoms are common in patients with leishmaniasis and paracoccidioidomycosis. The nasal manifestations prevail in leishmaniasis and oropharyngeal manifestations in the paracoccidioidomycosis.
BIBLIOGRAPHICAL REFERENCES1. Bailey BJ, Littlejohn MC. Granulomatous diseases of the Head and Neck, v. 1, chapter 15.
2. Lombardi FMO. Hanseníase, epidemiologia e controle - São Paulo: Imprensa Oficial do Estado: Arquivo do Estado. 1990.
3. Ribeiro FAQ, Lopes Filho O. Doenças Granulomatosas em ORL em Tratado de ORL - Otacílio & Campos, parte I, c. 8.
4. Martins ACC, Castro JC, Moreira JS. Estudo Retrospectivo de dez anos em endoscopia em cavidades nasais de pacientes com hanseníase. RBORL. 2005, 71(5):609-616.
5. Barton RPE, Davey TF. Early leprosy of the nose and throat. J Laryngol Otol. 1976, 90(10):953-61.
6. Barreto et al. Bol. Oficina San. Panam. 1981, 90:415-419.
7. Lessa MM et al. Leishmaniose Mucosa: aspectos clínicos e epidemiológicos. RBORL. 2007, 73(6):843-847.
8. Carvalho T, Dolci JEL. Avaliação clínica da influência do uso de glucantine em pacientes com Leishmaniose nasal. Acta ORL. 2006, 24(2):77-82.
9. Scott P. Impaired macrophage leishmanicidal activity at cutaneous temperature. Parasite Immunol. 1985, 7:277-88.
10. Falqueto A, Sessa PA. Leishmaniose Tegumentar Americana. In: Veronesi R, Focaccia R, editores. Tratado de Infectologia. 3ª ed. cap. 96. Rio de Janeiro: Atheneu; 2005, p. 1545-59.
11. Franco M, Mendes RP, Moscardi-Bacchi M et al. Paracoccidioidomycois. Baillière´s Clin Trop Med Commun Dis. 1989, 4:185-220.
12. Martinez R. Paracoccidioidomicose (Blastomicose Sul-Americana). In: Veronesi R, Focaccia R, editores. Tratado de Infectologia. 3ª ed. cap. 84. Rio de Janeiro: Atheneu; 2005, p. 1373-1403.
13. Silva GM, Patrocínio LG, Patrocínio A, Goulart MB. Avaliação Otorrinolaringológica na Hanseníase Protocolo de um Centro de Referência. Arquivos Internacionais de Otorrinolaringologia. 2008, 12(1):77-81.
1. Resident Doctor of Otorhinolaryngology.
2. Otorhinolaryngologist. Fellow in Otorhinolaryngology.
3. Otorhinolaryngologist. Assistant in the Sector of Otorhinolaryngology of the University Hospital of Universidade Estadual de Londrina.
4. Master's Degree by Unicamp in Otorhinolaryngology. Assistant Professor in the Sector of Otorhinolaryngology of the University Hospital of Universidade Estadual de Londrina.
5. Master in Medical Sciences by Universidade Estadual de Londrina. Coordinator in the sector of Otorhinolaryngology of the University Hospital of Universidade Estadual de Londrina.
Institution: University Hospital of Universidade Estadual de Londrina.Londrina / PR - Brazil.
Mail address:
Marco Aurélio Fornazieri
Avenida Robert Kock, 60 - Bairro Cervejaria
Londrina / PR - Brasil - CEP: 86038350
Tel: (+55 43) 3371-2000
E-mail: marcofornazieri@gmail.com
Article received on August 23, 2008.
Approved on September 21, 2008.