INTRODUCTIONThe cholesteatomas are cystic lesions coated by stratified squamous epithelium and filled by keratin, and are located in the temporal bone pneumatized areas (1). They have gradual growth, cause osseous erosion and may invade adjacent structures. This osseous destruction's etiopathogenesis is controversial, but some hypothesis considered include mechanical compression, osteoclastic action, production of proteolytic enzymes and cytosines (2).
Due to this destructive and insidious behavior the cholesteatoma may cause a number of complications. Such complications may be divided into intracranial and extracranial complications and are responsible for severe sequels and even the patient's death.
The intracranial complications include meningitis, brain abscess, thrombophlebitis of the lateral sinus, extradural abscess and otitic hydrocephalus.
In the pre-antibiotic era, the intracranial complications following the otologic diseases occurred in 2,3-6.4% of the cases and the mortality rate was of approximately 75%. In the post-antibiotic era, the incidence was reduced to 0,04-0,15% of the cases. The mortality also had a significant reduction, but some authors still report values that may reach 34% (3).
According to Smith e Danner (4), meningitis is the most common intracranial complication. Bento, Miniti and Marone (5) describe three dissemination passages for the occurrence of otogenic meningitis. hematogenic, congenital dehiscence (such as Hyrtl's fissures) or preformed (osseous erosion).
The brain abscess is the second most frequent, but most lethal complication. It's different from the meningitis that may occur for chronic otitis media, but it's the most frequent during acute otitis media episodes; the brain abscess is almost exclusively a consequence of the chronic otitis media. The most affected parts are the temporal lobe and cerebellum. The risk for a patient with chronic otitis media to develop a cranial abscess is of 1 in 10.000 patients per year, but in adults who's had the disease since the childhood this risk may increase to 1 in 200 patients per year (6, 7).
The presence of thrombophlebitis or the lateral sinus thrombosis during otologic infections occurs due to this sinus' vicinity to the middle ear and the mastoid cells (4). The sinus affection may result from osseous erosion, with the infection direct extension or may occur through the mastoid emissary veins thrombophlebitis. According to Isiris et al, after introduction of antibiotics and simple surgical procedure this complication mortality rate decreased to 10% (7).
The occurrence of extradural abscess is generally insidious and subtle, therefore many times the diagnosis is made incidentally during an image examination or surgical procedure. Dura mater irritation may seldom occur and consequently a worsening of ear ache and headache (4).
In 1931, Symonds reported and named for the first time the otitic hydrocephalus (8). Despite more than 70 years have elapsed, this complication physiopathology has not been defined yet. It's described as intracranial hypertension symptoms and signals, relating to the cerebrospinal fluid, except for the pressure that presents values larger than 300mmH2O (10). The name is considered to be unsuitable because it doesn't occurs only during otologic cases and the patients don't have dilatation of ventricles which characterizes the real hydrocephaly (4).
Subperiosteal abscess, Bezold's abscess, coalescing mastoiditis, petrositis, perichondritis, peripheral facial paralysis, labyrinthitis and labyrinthic fistula.
The subperiosteal abscess is the most frequent extratemporal complication (4, 11). It's more common in small children with acute otitis media, but may also occur in patients with chronic otitis media with or without cholesteatoma (4).
The Bezold's abscess is a cervical abscess that starts in the mastoid tip cells. It occurs in adults and older children in whom the mastoid pneumatization has already reached the tip. Like the subperiosteal abscess, the Bezold's abscess occurs more frequently in acute otitis media (12, 11).
Labyrinthic fistula is the most frequent complication in the cholesteatomatous disease. The lateral semicircular canal is the most affected labyrinthic portion and it's affected in approximately 90% of the cases (4, 13, 14). Although cochlear fistula is rare, it's more associated with the neurosensorial hearing loss (15).
The petrous apex composes the temporal bone anteromedial portion. It's pneumatized in about 30% of the individuals (16). It goes on with other temporal bone regions and may then be affected during middle ear and mastoid infections. The petrositis consists of dangerous infections due to the vicinity to the medial and posterior cranial cavity (4).
The incidence of peripheral facial paralysis associated to cholesteatoma is of approximately 1.1% (17), but this number may increase according to the affected region. When the tumor occurs in medial regions (such as petrous apex and internal acoustic meatus), the incidence may reach 20% (18, 19). There are several physiopathologies suggested in the literature to be responsible for the facial paralysis in the cholesteatomatous disease. They include ostitis, osseous erosion, compression with ischemia and direct bacterial or neurotoxins inflammation produced by the cholesteatoma's matrix (20).
The objective of this study is to document the patients with complicated cholesteatomatous chronic otitis media who were interned in the otorhinolaryngology nursery of the Clinical Hospital of São Paulo, between the years of 2001 and 2008.
METHODThis is a retrospective work and records of patients with complicated cholesteatomatous chronic otitis media were reviewed. The inclusion criteria were patients with complicated cholesteatomatous chronic otitis media with need for treatment internment. All patients were interned in the Otorhinolaryngology nursery of the Clinical Hospital of the Medicine College of the University of São Paulo in the period between 2001 and 2008. Patients with complications of the cholesteatomatous disease that were controlled in ambulatory were excluded.
The study included patients of both sexes and all ages.
The patients were initially attended in the otorhinolaryngology, neurosurgery or pediatrics emergency services. All patients were submitted to full otorhinolaryngological exam, laboratorial exams, computerized tomography with contrast and internment.
Upon interment the antibiotic chosen was empiric, based on the literature data. In some patients the medication was modified after the management result and antibiogram or under recommendation of the infectious diseases staff.
In case of suspicion of intracranial complication a neurosurgery evaluation was requested.
Where required evaluations were requested from other medical staffs for controlling associated diseases which could commit the patients' evolution.
RESULTSA total of thirty-four patients were interned in the Otorhinolaryngology nursery because of cholesteatomatous chronic otitis media complications in the period between 2001 and 2008.
The patients ranged from 7 to 83 years of age and 55% were between 10 to 30 years old (Chart 1).
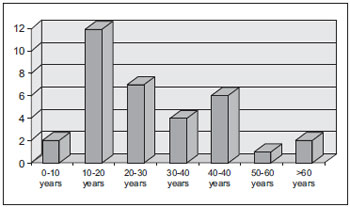
Chart 1. Age upon internment.
Twenty-six patients are of male sex and 73% of the patients are white.
Upon internment, 59% of the patients were illiterate or hadn't finished elementary school (Chart 2).
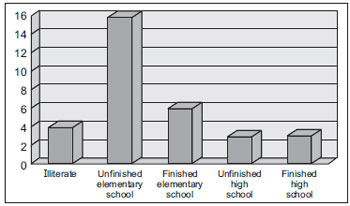
Chart 2. Education degree.
The right side was affected in 19 patients and the left side in 13 patients. Two patients were bilaterally affected.
Most patients (59%) had presented otologic symptoms since their childhood (Chart 3) and 11 patients had already been submitted to some otologic surgical procedure.
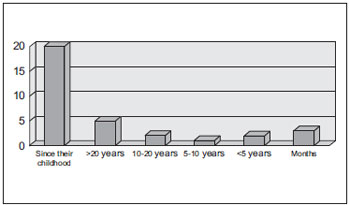
Chart 3. Beginning of otologic symptoms.
Fifteen patients had only one complication. The remaining nineteen had more than one complication (Chart 4).
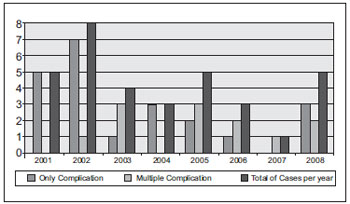
Chart 4. Number of complications per patient, divided annually.
Intracranial complications occurred in 17 patients (50%). Out of these, four (11%) patients also had extracranial complications. The venous thrombosis and the brain abscess were the most common intracranial complications and affected 9 patients each. The extradural abscess occurred in 5 patients and meningitis in 4 patients. One patient had (CAI) internal auditory meatus abscess.
Twenty-one patients (62%) presented extracranial complications.
Out of these eleven patients had subperiosteal abscess. The cutaneous fistula was the second most common extracranial complication and occurred in five patients. Three patients had peripheral facial paralysis. The Bezold's abscess was diagnosed in two cases. Six patients had a suggestive case of labyrinthic affection (Table 1).
One of the patients with facial paralysis indicated the beginning of the case about six months ago. During interment the patient didn't have adequate clinical conditions for surgery. Before the surgical procedure ambulatory clinical stabilization was carried out.
All other patients were submitted to surgery in the same internment. The radical mastoidectomy was performed in 21 patients and in one case tympanomastoidectomy was chosen. Out of 11 patients who had already been submitted to some otologic procedure 10 underwent radical mastoidectomy and the patient who had internal auditory meatus abscess was submitted to petrosectomy.
When secretion collection was possible, the material was forwarded for management. In only four patients the result was negative. The multibacterial flora was the most common and the mostly found bacteria were
Pseudomonas aeruginosa, Proteus spp, Staphilococcus aureus and
Bacterioides spp (Chart 5).
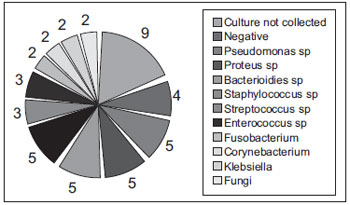
Chart 5. Result of the cultures collected in the intraoperative.
No patient died and in the six-month follow-up there didn't occur any incapacitating neurological sequels.
DISCUSSIONNowadays the incidence of the cholesteatomatous disease is highly associated with the country's development level and is more frequent in the less developed countries (19,21,22). Some socioeconomic factors are mentioned in the literature relating to high rates of complicated chronic otitis media. These may include overpopulation, poverty, ignorance and poor personal hygiene (23). The complication rate is also inversely proportional to the search for suitable medical service. Therefore, it's no surprise that the most affected population is that endowed with less resources. In our study we use the education degree as a parameter to evaluate the patients' socioeconomic level. We observed that 62% of the patients were illiterate or hadn't finished elementary school. A study carried out by Vikram et al (23) indicated that most of the patients with chronic otitis media are illiterate. It was also confirmed that these patients had a higher risk of complication.
Epidemiologically there was a masculine predominance confirming previous reports (22,24).
Differently from other studies with the use of magnetic resonance for all the patients with probable intracranial complications (14), none of our patients with tomographic suspicion of complication was submitted to other image exams.
Like in most of the literature works, the brain abscess was the most commonly found intracranial complication (4,22). The most affected parts were the temporal lobe and cerebellum, which also confirms the literature. However, we have found the same number of abscesses in each of these locations. This fact disagrees with other works that believe the temporal region abscesses are twice more frequent (24,25).
Another complication reported was the sigmoid sinus thrombosis. In the literature this complication rate varies from 17 to 34% (4,19,26). Our numbers are within those from the reports (26.4%). Out of the nine patients, seven presented other complications from which five were intracranial. The best approach still causes a lot of controversy. Many authors believe in the sinus spontaneous recanalization after adequate clinical or surgical treatment, without the need for the sinus direct manipulation (27). Others think the affected sinus draining is required (14,22). In our service the procedure is the sigmoid sinus puncture with thin needle whenever there is thrombosis suspicion. In case of pus releasing an opening is made to the sinus for the infection full draining.
Six patients (17%) had labyrinth affection. In five cases, the need for internment was due to other relating complication and the suspicion of labyrinthic fistula was incidental during the tomographic exam. Only one patient had only labyrinthic affection with signs of infectious labyrinthitis. During the surgery it was confirmed that in all cases there was lateral semicircular canal affection. In two patients the vestibule was also affected. Upper semicircular canal fistula was identified in only one case.
The labyrinthic fistula percentage in our study was larger than that documented in the literature (7%) for chronic cholesteatomatous otitis media (22,28). The reason for such a high number is maybe because most of our patients had had complicated cholesteatomatous disease for a long time.
The facial paralysis resulting from cholesteatoma is rare (1.1%), in spite of the incidence of nerve dehiscence relating to the fact cholesteatoma changes the values between 12.6 to 33.3% (2). According to Lela Mirigov, acute mastoiditis complicated by peripheral facial paralysis must be associated with cholesteatoma in 66% of the cases (29). The early surgery is undoubtedly the best treatment (1,2). Every tumor must be removed and the nerve decompressed without opening the cladding. Out of the three cases that included facial paralysis, two were submitted to radical mastoidectomy with nerve decompression. The patients had House-Brackmann II and III. In spite the facial paralysis associated with cholesteatomatous disease has a bad prognostic (16), both patients had a full recovery of the facial movements.
Like other literature articles, our group believes the best surgery for complicated cholesteatomatous otitis media is the radical mastoidectomy (3,22). We also believe the infectious focus elimination must be made as early as possible. Out of 17 patients with intracranial complication, ten were submitted to mastoidectomy in the first 24 hours of internment. The other patients were interned in other clinics and submitted to the surgery as soon as the otorhinolaryngology evaluation was requested.
The germs found were similar to those of prior reports. According to a work published in 2008 with 62 cases of complicated cholesteatomas, the germs most frequently found were
Pseudomonas, Staphilococcus aureus and
Proteus (21). Practically the same germs found by Bento, Brito and Ribas in a work published in 2006 (22). In this last edition, the
Bacterioides was one of the most frequent bacteria, similarly to our study.
In our study the anaerobes didn't play an important etiologic role. (3,24) This result disagrees with the research carried out by Mathews and Oliver (30), that isolated anaerobes in 40% of the cholesteatomas managements. Such discrepancy is maybe due to an inadequate technique in the management of cultures for anaerobes. One of the reasons was the delay to sow the cultures due to the fact the surgeries occurred out of business hours.
CONCLUSIONEvery patient with suspicion of complication needs to be followed up by several medical specialities, and must be submitted to full physical exam and computerized tomography with contrast.
The treatment must be aggressive with interment, intravenous antibiotic and early draining of the infectious focus in order to reduce the morbimortality rate.
BIBLIOGRAPHICAL REFERENCES1. Testa JRG, Vicente AO, Abreu CEC, Benbassat SF, Antunes ML, Barros FA. Colesteatoma causando paralisia facial. Rev Bras Otorrinolaringol. 2003, 69:657-662.
2. Moody MW, Lambert PR. Incidence of Dehiscence of the Facial Nerve in 416 Cases of Cholesteatoma. Otology and Neurotology. 2007, 28(3):400-404.
3. Hafidh MA, Keogh Ivan, Walsh RMC, Walsh M, Rawluk D. Otogenic intracranial complications. A 7-year retrospective review. American Journal of Otolaryngology-Head and Nack Medicine and Surgery. 2006, 27:390-395.
4. Smith JA, Christopher JD. Complications of Chronic Otitis Media and Cholesteatoma. Otolaryngol Clin N Am. 2006, 39:1237-1255.
5. Bento RF, Minitti A, Marone SAM. Complicações intratemporais e intracranianas das otites médias. In: Tratado de Otologia-São Paulo: Editora da Universidade de São Paulo: Fundação Otorrinolaringologia: FAPESP; 1998, p. 233-240.
6. Nunez DA, Browning GG. Risks of developing na otogenic intracranial abscess. J Laryngol Otol. 1990, 104:468-472.
7. Ustündag E, Keskin G, Almaç A. Management of Lateral Sinus Thrombosis in Chronic Otitis Media. Otology and Neurotology. 2006, 27(8):1098-1103.
8. Symonds CP. Otitic hydrocephalus. Brain. 1931, 54:55.
9. Doyle KJ, Brackmann DE, House JR III. Pathogenesis of otiitic hydrocephalus: clinical evidence in support of Symond's (1937) theory. Otolaryngol Head Neck Surg. 1994, 111:323-327.
10. Sennaroglu, L, Kaya S, Gursel B, Saatçi I. Role of MRI in the Diagnosis of Otitic Hydrocephalus. The American Journal of Otology. 1996, 17:784-786.
11. Spiegel JH, Lustig LR, Lee KC, Murr AH, Schindler RA. Contemporary Presentation and Management of a Spectrum of Mastoid Abscesses. Laryngoscope. 1998, 108(6):822-828.
12. Furukawa K, Arai E, Kobayashi T et al. A case of Bezold´s abscess associated with cholesteatoma. Nippon Jibiinkoka Gakkai kaiho. 1992, 95(12):1901-1905.
13. Penido NO, Barros FA, Iha LCN, Abreu CEC, Silva RN, Park SW. Fístula labiríntica na otite media crônica colesteatomatosa. Rev Bras Otorrinolaringol. 2003, 69(4):521-525.
14. Voegels RL, Garcia M, Bogar P, Miniti A, Bento RF. Fístula Perilinfática Devido à Colesteatoma: Estudo de 14 casos. Rev Bras Otorrinolaringol. 1994, 60(1):39-42.
15. Copeland BJ, Buchman CA. Management of labyrinthine fistulae in chronic ear surgery. Am J Otolaryngol. 2003, 24(1):51-60.
16. Harker LA, Shelton C. Complications of temporal bone infections. In: Cummings CW, editor. Cummings otolaryngology head and neck surgery. 4th edition. Philadelphia: Elsevier Mosby; 2005. p. 3013-3038.
17. Swartz JD. Cholesteatoma of the middle ear: dignosis, etiology and complications. Radiol Clin North Am. 1984, 22:15-34.
18. Atlas MD, Moffat DA, Hardy DG. Petrous Apex Cholesteatoma: Diagnostic and treatment dilemmas. Laryngoscope. 1992, 102:1363-1368.
19. Faye MB, Ba MC, Diakhate IC, Hossini A, Renaux. Cholestéatome compliqué d'abcès de la fosse postérieure. Rev Laryngol Otol Rhinol. 2006, 127(3):161-163.
20. Yetiser S, Tosun F, Kazkayas M. Facial Nerve Paralysis Due to Chronic Otitis Media. 2002, 23(4):580-588.
21. Naseeruddin K, Venkatesha BK, Manjunath D, Savantrewwa IR. Complications in primary and secondary acquired cholesteatoma: a prospective comparative study of 62 ears. American Journal of Otolaryngology-Head and Neck Medicine and Surgery. 2008, 29:1-6.
22. Bento R, Brito R, Ribas GC. Surgical management of intracranial complications of otogenic infection. Ear, Nose and Throat Journal. 2006, 85(1):36-39.
23. Vikran BK, Khaja N, Udayashankar SG, Venkatesha BK, Manjunath D. Clinico-epidemiological study of complicated and uncomplicated chronic suppurative otitis media. The Journal of Laryngology and Otology. 2008, 122:442-446.
24. Kangsanarak J, Navacharoen N, Fooanant S, Ruckphaopunt K. Intracranial complications of suppurative otitis media: 13 years' experience. The American Journal of Otology. 1995, 16:104-109.
25. Bradley PJ, Manning KP, Shaw MD. Brain abscess secondary to otitis media. J Laryngol Otol. 1984, 102:121-124.
26. Samuel J, Fernandes CM, Steinberg JL. Intracranial otogenic complications: A persisting probl. em. Laryngoscope. 1986, 96:272-278.
27. Agarwal A, Lowry P, Isaacson G. Natural history off sigmoid sinus thrombosis. Ann Otol Rhinol Laryngol. 2003, 112:191-194.
28. Dornhoffer JL, Milewski C. Management of the open labyrinth. Otolaryngol Head Neck Surg. 1995, 112(3):410-414.
29. Migirov L. Computed tomographic versus surgical findings in complicated acute otomastoiditis. Ann Otol Rhinol Laryngol. 2003,112(8):675-677.
30. Newland WJ. Otogenic brain abscesses: a study of 80 cases. J Laryngol Otol. 1965, 79:120-130.
1. Otorhinolaryngologist. Medical Doctor of the Otology Group of the Otorhinolaryngology Discipline of the Medicine College of University of São Paulo.
2. Free Professor in the Otorhinolaryngology Discipline of the Medicine College of the University of São Paulo. Assistant Doctor in the Otorhinolaryngology Discipline of the Medicine College of University of São Paulo.
3. Titular Professor of the Otorhinolaryngology Discipline of the Medicine College of University of São Paulo. Head of the Ophthalmology and Otorhinolaryngology Department of the Clinical Hospital of the Medicine College of the University of São Paulo.
Institution: Otorhinolaryngological Clinical Division of the Clinical Hospital of the Medicine College of the University of São Paulo.São Paulo / SP - Brazil
Mail address:
Ricardo Ferreira Bento
Rua Dr. Enéas Carvalho de Aguiar, 255 - 6º Andar - Sala 6021
São Paulo / SP - Brazil - Zipcode: 05403-000
Telephone/Fax: (+55 11) 3088-0299
E-mail: gazumartins@uol.com.br
Article received on August 30, 2008.
Approved on October 17, 2008.