INTRODUCTIONEpistaxis is defined as a bleeding of the nasal mucosa, and represents the most common emergency in otorhinolaryngology, with prevalence of about 10 to 12%, generally associated to prevailing factors such as systemic arterial hypertension, trauma and coagulopathy (1, 3, 7). The admission criteria are: severe epistaxis with clinical repercussion in patients with hypertension crisis, difficulty to the service control or associated to pathologies that require medical care (4). It may clinically be divided into anterior and posterior with significant differences in its manifestation and prognosis (2).
The etiology of epistaxis is divided into local and systemic causes. Local causes: Inflammatory-infectious (rhinitis, rhinosinusitis), traumatic (digital, fractures, nasal surgeries), anatomic (septal deviation and perforation), foreign body, chemical or climatic agents and nasal tumors (nasoangiofibroma, nasal polyposis, inverted papilloma, carcinoma). Systemic causes: The arterial hypertension is the most frequently associated clinical factor, blood dyscrasia, drugs (acetylsalicylic acid, anticoagulants, non-hormonal anti-inflammatory, antibiotics), neoplasms etc. It is important to find the bleeding site and define its etiology (local or systemic) for indication of the best treatment. The severe epistaxis, associated to prevailing factors such as systemic arterial hypertension and coagulopathy may need a surgical approach in the cases refractory to conservative treatment, such as cauterization and nasal splint (5,7,8).
Epistaxis and arterial hypertension are frequent in the population, but an association is still controversial; it occurs in patients with severe epistaxis and the pressure levels are higher when compared to other patients in emergency services (10). In some studies the arterial hypertension would determine structural alterations of the nasal vessels similar to those verified in the cerebral circulation and retinal examination. The loss of the elastic layer and of contractile properties of the arteries in the elderly would explain a more severe bleeding than that of younger people with arterial hypertension; the dilation of the vessels would represent some degree of degeneration of the vessels wall that would favor bleeding. The association of epistaxis, hypertension and hypertrophy of the left ventricular would be a consequence of the long duration of the hypertension (9).
The association with blood dyscrasia is more frequent with the use of non-hormonal anti-inflammatory, drugs that alter the metabolism of the arachidonic acid and the function of the platelets which leads to bleeding. In hemophilia, Von Willebrand's disease and thrombocytopenia there occurs intermittent nasal bleeding due to the abnormal coagulation function; epistaxis is the most common symptom in approximately 60% of the patients with Von Willebrand's disease (12).
The nasal trauma (digital, fractures and cranioencephalic traumatism) may cause epistaxis; the high prevalence in younger men probably regards the higher exposure to trauma in sports, traffic and urban violence (11).
The advance of endoscopic techniques and instruments for the treatment of severe posterior epistaxis and refractory anterior epistaxis has been preventing prolonged admissions and morbidities caused by the nasal splint, with endoscopic ligation of the sphenopalatine artery. If the bleeding is defined to be anterior, the chemical or electric cauterization (silver nitrate or trichloracetic acid) may be the ultimate treatment; another option is the anterior splinting (with vaseline-soaked gauze, glove finger or merocel), The posterior bleeding is normally highly intense and it is many times difficult to find the bleeding point, in the first service; antero-posterior splinting (with Foley probe or gauze) to stabilize the patient and identify factors that may contribute for such bleeding; then surgical center evaluation is indicated. After the bleeding point is found, the electrocauterization is carried out on profuse bleedings, and the endoscopic ligation of the sphenopalatine artery is indicated in case of difficult identification. It represents a safe surgical approach, because it prevents complications of the maxillary artery ligation (edema and facial anesthesia, oroantral fistula and dental desensitization), interrupts the nasal flow at terminal position, prevents regressive local bleeding and anastomosis in the bilateral carotid systems and assures a satisfactory control of bleeding with a rebleeding rate within that found in the maxillary artery ligation technique (0.5 to 15%) (5,7). Other types of treatment for refractory epistaxis include embolisation used as a complementary or alternative treatment, and its advantages are: finding of the bleeding region, diagnosis of associated diseases such as tumors and vascular lesions; it does not require general anesthesia, and disadvantages like: need for sophisticated equipment and specialized staff. The method limitations are for bleeding of ethmoidal arteries and atherosclerotic disease in carotid artery (1,6).
The objective is to evaluate the main associated prevailing factors in patients with epistaxis and its treatment.
METHOD Retrospective study of patients admitted with epistaxis between 2005 and 2006. Inclusion criteria: patients with epistaxis who need admission due to clinical repercussion of bleeding or other associated pathology, with one of the prevailing factors: arterial hypertension, cranioencephalic and face traumatism and coagulopathy (hematological pathologies and the use of anticoagulants). Exclusion criteria: patients with epistaxis who did not need admission were excluded. The patients were initially submitted to anterior and/or antero-posterior splinting for epistaxis control and the following laboratory exams were requested: hemoglobin, hematrocit, platelets number, prothrombin time (PT, INR) and activated partial thromboplastin time (aPTT), For patients who needed sphenopalatine artery ligation, the surgical procedures were carried out under general anesthesia with endoscopic viewing (optics of 30o of 4mm of diameter). Evaluation as for age, sex, prevailing factors and treatment.
Work approved by the Ethics Committee in Research of the Irmandade da Santa Casa de Misericórdia de Santos, under the number 88/2008.
RESULTSMost patients were men, in the proportion of 1,5 per 1 woman, and the age range varied from 1 to 88 years old ((37± 26, average ± DP), prevailing between 11 to 30 of 35% (n=21) and 51 to 60 years of 28% (n=17) Table 1. The prevailing factors were: arterial hypertension 36% (n=22), trauma 16% (n=10), coagulopathy 5% (n=3), nasal tumor (nasoangiofibroma) 3% (n=1) and patients in whom no prevailing factor was identified 40% (n=24) Table 2.
The treatment in 35 patients (58%) was nasal anterior splint, 16, (27%), antero-posterior nasal splint, in five patients (8%) the arterial ligation via endoscopy and in four patients the electrocauterization of the bleeding point (7%) (Graphic 1).
The patients submitted to anterior nasal splint (n=35) for 48h, antero-posterior splint for 72 hours (n=16) were received antibiotic therapy in all cases to avoid infectious complications. The procedure in the first 24 hours bleeding recurrence, after clinical stabilization, was removal of the antero-posterior splint under general anesthesia, electrocauterization (n=4) where the bleeding point was found, arterial ligation via endoscopy (cauterization) upon diffuse bleeding, four patients presented with arterial hypertension and in one patient we identified a prevailing factor. One patient had diagnosis of nasal tumor and was submitted to surgery. The patients with arterial hypertension, coagulopathy and cranioencephalic traumatism were forwarded to multidisciplinary equip for base pathologies. No patient had complication.
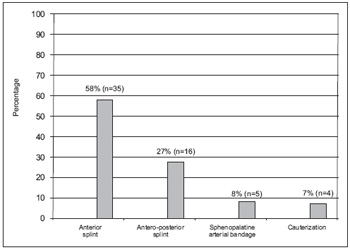
Graphic 1. Procedure in patients with epistaxis.
Epistaxis may manifest as a severe picture that requires hospital admission, affects all age ranges, occurs with a higher frequency in elder and male patients (7,8). In our study, the age range varied from 1 to 88 years and was prevalent from 11 to 30 years (35%) and 51 to 60 years old (28%), most patients being male. In children, it generally comes from the anterior region of the nasal cavity and is caused by local alterations; in most adults it's associated with systemic alterations and comes from the posterior part of the nasal cavity (7).
The severe epistaxis is normally associated to prevailing factors; in our study, the systemic arterial hypertension was the most frequent, 36% (n=22), trauma 16% (n=10) and coagulopathy 5% (n=3); in some other studies we have arterial hypertension (33% to 61%), coagulopathy (16.5%), trauma (9 to 38%) (7,11).
Epistaxis and arterial hypertension are frequent in the population, more evident in patients with severe epistaxis, with prevalence of 24 to 64% in these cases (10), the patients with arterial hypertension, 36% (n=22), had bleeding with clinical repercussion, and received antero-posterior splint, good evolution arterial pressure control in 18 patients and in four we needed to make ligation of the sphenoid artery.
Some studies show that in patients with severe bleeding coagulopathy is researched, but the alterations are more frequent in patients with the use of acetylsalicylic acid and non-hormonal anti-inflammatory, medications that alter the arachidonic acid metabolism and the function of the platelets and lead to bleeding (12); in our study, the patients, 5% (n=3), were interned for hematology with plateletpenia and had epistaxis during admission; we carried out anterior splint with Gelfoam to prevent trauma; for patients using anticoagulants, the service treatment was effective and they were not included in the study.
The epistaxis for external trauma was associated to cranioencephalic traumatism in male patients, 16% (n=10); our hospital is a reference in polytraumatized patients service. In our study, 40% (n=26), no prevailing factor was identified as a cause of bleeding, and one patient (3%) presented the diagnosis of nasoangiofibroma.
The treatment may be by anterior, antero-posterior splint, electrocauterization, endoscopic arterial ligation (with clip or cauterization) and embolisation; our study carried out anterior splint in 35 patients (58%), antero-posterior splint in 16 (27%), bleeding point electrocauterization in four patients (7%) and endoscopic arterial ligation in five patients (8%); no patient was submitted to embolisation; in the literature, the patients are submitted to conservative methods of treatment before the performance of endoscopic arterial ligation (4). The sphenopalatine artery ligation was successfully carried out in five patients (8%); we initially applied antero-posterior splint for epistaxis control and clinical stabilization, the cases refractory to conservative actions were evaluated in a surgical center for finding of the bleeding point and when it was identified we carried out electrocauterization; for cases with diffuse bleeding the sphenopalatine artery ligation with cauterization were indicated. The arterial embolisation is also a good option to treat the cases of severe epistaxis; no patient was submitted to such procedure in our study. In cases of severe epistaxis, with the recent advances of endoscopic techniques and instruments, these allow a fast and safe arterial ligation to be made early and prevent long internments and morbidity related to the use of splint (1). The time of internment ranged from 3 to 7 days as verified in other studies (1,4,7).
CONCLUSION
The main prevailing factors associated to epistaxis were systemic arterial hypertension, trauma and coagulopathy. The early endoscopic arterial ligation is indicated for patients with severe epistaxis and prevailing factors, because it prevents prolonged internments and morbidities associated to the nasal splint.
BIBLIOGRAPHICAL REFERENCES
1. Douglas R, Wormald PJ. Update on Epistaxis. Otorrinolaringology Head and Neck Surgery. 2007, 15 (3):180-83.
2. ChiuT, McGarry W. Prospective clinical study of bleeding sites in idiopatic adult posterior epistaxis. Otolaringology Head and Neck Surger. 2007, 137(3):390-93.
3. Chiu T, Dunn JS. An Anatomical Study of Arteries of the Anterior Nasal Septum. Otolaringology Head and Neck Surgery. 2006, 134(1):33-36.
4. Venosa A, Butugan O, Voegels RL et al. Epistaxe Severa: Estudo Retrospectivo. Rev Bras Otorrinolaringol. 1998, 64(1):57-60.
5. Thornton MA, Mahesh BN, Lang J: Posterior Epistaxis: Identification of Common Bleeding Sites. Laringoscope. 2005, 115(4):588-90.
6. Arbulú CZ, Tsuji RK, Lessa MM, Voegels RL, Butugan O. Grave complicação do tratamento de epistaxe: relato de caso. Rev Bras Otorrinolaringol. 2004, 70(1):124-128.
7. Santos, PR, Leonhardt FD, Ferri RG, Gregório LC. Ligadura endoscópica endonasal da artéria esfenopalatina para epistaxe severa. Rev Bras Otorrinolaringol. 2002, 68(4):511-14.
8. Ikino CMY, D' Antônio WEPA, Murakami MS, Miziara ID, Butugan O. Epistaxes recorrentes: Estudo dos fatores clínicos e laboratoriais associados. Rev Bras Otorrinolaringol. 1999, 65(2):149-53.
9. Lubianca Neto JF, Fuchs FD, Facco SR et al. Is epistaxis evidence of end-organ damage in patients with hypertension? Laryngoscope. 1999, 109(7):111-115.
10. Herkner H, Havel C, Mullner M et al. Active epistaxis at ED presentation is associated with arterial hypertension: American Journal of Emergency Medicine. 2002, 20(2):92-94.
11. Hussain G, Igbal M, Shah SA, Said M et al. Evaluation of aetiology and efficacy of management protocol of epistaxis: J Ayub Coll abbottabad. 2006, 18 (4):62-65.
12. Dizdar O, Onal IK, Ozakin E et al. Research for bleeding tendency in patients presenting with significant epistaxis: Blood Coagulation and Fibrinolysis. 2007, 18(1):41-43.
1. Specialist in Otorhinolaryngology, in course for Master's Degree (Post-Graduation) of the Discipline of Otorhinolaryngology of the Medical Sciences School at Santa Casa de São Paulo. Head of the Otorhinolaryngology Service at the Irmandade da Santa Casa de Misericórdia de Santos.
2. Trainee Doctor of the Otorhinolaryngology Service at the Irmandade da Santa Casa de Misericórdia de Santos.
Institution: Irmandade da Santa Casa da Misericórdia de Santos. Santos / SP - Brazil. Mail Address: Myrian Marajó Dal Secchi - Avenida Ana Costa, 254 - conj. 72 - Santos / SP - Brazil - Zip-Code: 11060-000 - Telephone: (+55 13) 3234-7736 - E-mail: dalsecchi@uol.com.br. Article received on November 20 2008. Approved on October 12 2009.