INTRODUCTIONFibromyalgia (FM) is a non-inflammatory musculoskeletal chronic syndrome, whose etiology is unknown, characterized by a diffuse pain, increase in palpation sensitivity and such symptoms as tiredness, insomnia, anxiety, depression, cold intolerance and otologic complaints. Although the FM-controlling physiological mechanisms have not been determined, neuroendocrine, genetic or molecular factors can be involved (1, 2).
Recent researches reveal biochemical, metabolic and immunoregulation abnormalities. The most accepted mechanism to understand FM's physiopathology is that of an alteration in any central mechanism of pain control, which could result in a neurohormonal dysfunction. Such a dysfunction would include a deficit of inhibitor neurotransmitters in spinal or supraspinal levels (serotonin, enkephalin, norepinephrine, etc.), or a hyperactivity of exciting neurotransmitters (P substance, glutamate, bradykinin and other peptides), or both conditions could be present. These dysfunctions could be triggered by a viral infection, mental stress or a physical trauma and they could be genetically predetermined (1).
Several abnormalities have been observed in FM patients, some of which are notable: a) release of P substance (neurohormone) at high levels in the cerebrospinal fluid; b) deficit of serotonin in the platelet; c) low level of adenosine triphosphate; d) abnormal metabolism of carbohydrates in the red blood cells; e) abnormal regulation of cortisol production; and f) reduction of blood flow in certain brain structures (3).
The influence of genetic or molecular mechanisms can be involved. Several studies have approached the frequency in FM patients' diverse relatives, suggesting that these factors can play a relevant role on its etiopathogenesis (2).
Recent studies demonstrate that the frequency of polymorphisms of the genes catechol-O-methyltransferase (COMT) with a L/L genotype was higher in FM patients, indicating that this genotype produces a damaged enzyme unable to metabolize the catecholamines of the system effectively. Although the FM involves a polygenic situation and environmental factors, the molecular study can help identify susceptible individuals (2).
It has been widely attempted to clarify the organic FM pathogenesis in the last decade, researches in genetics, biogenic amines, neurotransmitters, hormones of the hypothalamus-pituitary-adrenal axis, oxidative stress, mechanisms of pain relief, central sensitivity and autonomic function in FM reveal a series of abnormalities, indicating that a wide range of factors and mechanisms can be involved in the pathogenesis of this disease (4).
Studies demonstrate that there is a lack of regulation in the central nervous system at FM and they tackle the dysautonomia as a potential mechanism participating in the genesis and maintenance of the symptomatology and co-morbidities (4).
ALVARES and LIMA (5) and MARTINEZ et al. (6), mention that the occupational overload comprises an important etiologic factor and it can be preceded by the work-related musculoskeletal disorders (WMSD/RSI).
Researches reveal that various FM symptoms can be confused with those of leprosy reactions and that both diseases can occur on a simultaneous basis (7). Furthermore, it is mentioned that FM patients can show a high level of thyroid-stimulating hormone (TSH), hence indicating an association with hypothyroidism.
FM prevalence is approximately 2% of the general population; it is responsible for 15% of the consultations in rheumatology ambulatories and between 5% and 10% in general clinical ambulatories. The female-to-male ratio is approximately 6 to 10:1. The highest prevalence is within the age group between 30- and 50, and it can occur in childhood and senior age as well (1, 10).
FM diagnosis, as per the criteria determined by the American School of Rheumatology in 1990, are as follows (1):
a) diffuse pain lasting for a minimum of three months in the following areas: pain on the left and right sides of the body, pain above and below the waist line, pain in the axial skeleton (cervical column or anterior thoracic column, or thoracic column or lumbar column). Pain on the shoulder or on the buttock is considered a pain for each side concerned;
b) pain in at least 11 out of the 12 palpated points called "tender points" with a nearly 4-kg strength. In order to consider a "tender point" positive, the patient must declare that palpation was painful. The presence of the painful points is the essential finding of the study.
Disorders in the oculomotor function are reported in FM and they can be derived from the dysfunction in the mechanisms responsible for their regulation as a result of the reduction of the blood supply into the labyrinth (11).
Because of their manifestations and impairment areas, several rheumatologic diseases can cause vestibular alterations, and the otoneurologic tests are fundamental tools to confirm the vestibular disorders and their relations with the central nervous system (CNS) (12).
The objective of the present study was to evaluate the vestibular behavior in fibromyalgia patients.
METHOD25 female FM patients aged between 26 and 65 (average age of 52.2; standard deviation of 10.3) were submitted from the Rheumatology Ambulatory of the Federal University of Paraná (HC-UFPR) to the Otoneurology Department of an Institution in the city of Curitiba/PR.
It is about a transverse study and the patients were evaluated regardless of type and time of treatment.
Individuals diagnosed of fibromyalgia without middle ear pathologies were included in the research. Individuals showing an otological alteration or other abnormalities that would make the exam impracticable were excluded from the research.
The research was approved by the Institutional Ethical Committee under record Nº 0187/2009 and after being authorized by the patients' signatures in the Free and Clarified Agreement Term, they were submitted to the following procedures:
The patients were submitted to the following procedures:
Anamnesis A questionnaire was applied with an emphasis on otoneurological signals and symptoms, personal and family histories.
Otorhinolaryngological Evaluation It was performed with the intention to excluding any alteration that might interfere with the exam.
Vestibular Evaluation The patients were submitted to the following tests integrating the vestibular exam:
Firstly, vertigo and positional/positioning, spontaneous and semi-spontaneous nystagmus were surveyed.
Secondly, to perform vectoelectronystagmograph a Berger VN316 three-recording channels thermosensitive equipment was used. An active electrode was placed firmly with electrolyte paste in the lateral angle of each eye and in the posterior median line, making an isosceles triangle to allow the horizontal, vertical and oblique eye movements to be identified, as well as especially to calculate the angular speed of the slow component of the nystagmus (ASSC).
A Frante pendular rotary chair, a Neurograff EV VEC visual stimulator and a Neurograff NGR 05 air were used.
The following eye and labyrinth tests to VENG were performed in accordance with the criteria suggested by the authors MANGABEIRA-ALBERNAZ et al. (13).
-Eye movement calibration in this exam stage, the evaluated clinical feature was the trace conformity, making the researches compatible with each other.
-Research of spontaneous nystagmus (open and closed eyes) and semi-spontaneous (open eyes). In this record, the occurrence, direction, inhibitory effect in eye fixation (IEEF) and the value of maximum nystagmus ASSC.
-Research of pendular tracking to evaluate the occurrence and type of curve.
-Research of the optokinetic nystagmus at the speed of 60º per second in the clockwise and counterclockwise courses, in the horizontal direction. The occurrence, direction, maximum ASSC were evaluated as to the clockwise and counterclockwise movements of nystagmus.
-Research of pre-rotary and post-rotary nystagmus at the rotary decreasing pendular test, by stimulating the lateral, anterior and posterior semicircular ducts. To stimulate the lateral semicircular ducts (horizontal), head was inclined 30% forward. On the next stage, to sensitize the anterior and posterior semicircular ducts (vertical), the head position was 60o backward and 45o to the right; next, 60o backward and 45o to the left, respectively. The occurrence, direction, frequency to the clockwise and counterclockwise rotations of nystagmus were observed.
-Research of the pre-caloric and post-caloric nystagmus performed with the patient in such a position to incline the head 60o backward in order to properly stimulate the lateral semicircular ducts. The time to irrigate each ear with air at 42oC and 20oC was 80s for each temperature and the responses were recorded with the eyes closed and, next, with eyes open to observe IEEF. In this evaluation, the direction, absolute ASSC values and the ratio calculation of the directional preponderance and the labyrinthic prevalence of the post-caloric nystagmus were observed.
Statistical AnalysisThe Test of Proportional Differences was performed in order to compare the results of the vestibular exam (analysis of the normal and changed results) and those of Fischer's Test (associating the results of the vestibular exam with walking disequilibrium and tinnitus). 0.05 or 5% was defined as the rejection level at a null hypothesis.
RESULTSThe frequency of the otoneurological signals and symptoms in FM patients is found on Table 1.
The frequency of diverse clinical signals can be observed in Table 2.
The research of positional nystagmus was not performed due to the patients' physical impracticality and the following evidences; calibration of eye movements, research of spontaneous nystagmus with open and closed eyes, semi-spontaneus nystagmus, pendular track and optokinetic nystagmus did not show alterations.
At the caloric test, five bilateral labyrinthic hyporeflexia cases (20,0%), three unilateral labyrinthic hyperreflexia cases (12,0%), two asymmetrical labyrinthic prevalence cases (LP) (8,0%), one unilateral labyrinthical hyporeflexia case (4,0%) and one bilateral labyrinthic hyperreflexia case (4,0%) occurred. In thirteen cases (52.0%), the exam was within the normality standards (normoreflexia) as shown by Table 3.
In twelve cases, (48.0%) peripheral vestibular dysfunctions occurred, out of which eight deficit peripheral vestibular dysfunction cases (32.0%) and four irritating peripheral vestibular dysfunction cases (16.0%). The vestibular exam was normal in thirteen cases (52.0%), as shown by Table 4.
When applying the Ratio Test, it proves that there is no significant difference between the ratios of normal and changed exams (p = 0.7785).
The Correlation between the result of the vestibular exam and the presence of walking disequilibrium can be observed on Table 5.
When applying Fischer's Test, it proves that there is a significant difference between the rations of patients with normal vestibular exam (NVE) and the changed vestibular exam (CVE) with and without a walking disequilibrium (p= 0.0131).
The Correlation between the result of the vestibular exam and the presence of tinnitus can be observed on Table 6.
When applying Fischer's Text, it proves that there is a significant difference between the ratios of patients with NVE and CVE with and without tinnitus
(p = 0.0002).
DISCUSSIONAt anamnesis, the occurrence of wide-ranging otoneurological and clinical symptoms were verified, some of which can be mentioned as the highest prevalent ones, namely: difficulty or pain when moving neck and pain spread to arm or shoulder (92.0%) in each, dizziness (84.0%) and headache (76.0%); depression (80.0%), anxiety (76.0%) and insomnia (72.0%). The symptoms are varied and the pain is manifested in muscular and periarticular areas, becoming gradually generalized. According to the literature, the dizziness and tinnitus symptoms are commonly mentioned in FM (1, 2, 11, 14, 15). For HADJ-DJILANI and GERSTER (15) the otoneurolgical symptoms can derive from musculoskeletal abnormalities that are common in FM and they can impair the proprioception by causing an instability sensation.
JACOMINI and SILVA (4) mention that the association between the otorneurological signals and symptoms and FM is demonstrated in a number of studies revealing that there is a lack of regulation of the autonomous nervous system, hence causing dysautonomia. The authors suggest that FM is a generalized form of reflex sympathetic dystrophy. Studies performed in animals show that the trauma can unleash a permanent sympathetic hyperactivity, the pain neurotransmitters are changed and abnormally activated by noradrenaline, what would explain the mechanism known in medicine as sympathetically maintained pain. This type of pain is characterized by post-trauma installation, for its independence from any tissue damage and for the presence of allodynia. For the authors, the sympathetic hyporeactivity provides a coherent explanation for permanent fatigue and other symptoms associated with vertigo, mental confusion and weakness.
Emerging genome investigations have contributed to clarify the participation of the sympathetic system in FM. The catechol-O-methyltransferase (COMT) is an enzyme that disables catecholamines and drugs containing the catechol group. The COMT-coding gene is mapped and the influence of polymporphism of this gene has been investigated in an attempt to elucidate its involvement in the pathogenesis of a variety of psychiatric disorders and pain perception. The meaning of polymorphism of the gene expressing COMT was studied in FM, and, three polymorphisms are considered: LL (low/low), LH (low/high/intermediate) and HH (high/high) that determine the degrading rate of catecholamines or other catecholic drugs (16).
GURSOY et al. (16) reported that 73.8% of the women showing FM had a low or intermediate enzymatic activity and 26.2% had a high enzymatic activit. This result, LL variant - a lot noticed - and HH variant - little noticed, results in a low or high degradation of catecholamines, respectively. This means that the lower the enzymatic activity the more catecholamine is found. Such results confirm the idea of the hyperactive sympathetic system in FM and prove the involvement of COMT polymorphism in FM.
Current evidences maintain the hypothesis of a neuromodulation disorder of pain, involving the CNS especially. The suggested physiopathology is related to a primary disorder in the central mechanism of pain in FM individuals, as a result of neurotransmitter alterations. The neurohormonal dysfunction would include a deficit of inibitory neurotransmitters (serotonin, enkephalin, norepinephrine, and others) or a hyperactivity of the exciting (P substances, glutamate, bradykinin and other peptides), or both situations simultaneously (1).
The serotonin deficit contributes to sleep disorders and increase in pain, influencing the release of P substance. The reduction of tryptophan levels (predecessor of serotonin and neuromodulator) and other aminoacids an an increase in the concentration of the P substance, endorphins and 5-hydroxyindoleacetic acid were found in the blood and liquor of FM individuals (1).
As to the vestibular evaluation, a change in the peripheral vestibular system was observed in 12 patients, and this change was found in the caloric test prevailed by the deficit peripheral vestibular dysfunctions. ROSENHALL, JOHANSSON and ORNDAHL (11) mentioned a presence of positioning nystagmus, spontaneous nystagmus with open eyes and no eye fixation, alteration in saccadic movements, speed of the pendular tracking and hyperreflexia to caloric stimulation. They found 35% of CNS-involved vestibular system dysfunction. ZEIGELBOIM et al (12) and BAYAZIT et al. (14) observed a peripheral dysfunction only in the caloric test with the presence of hyporeflexias and hyperreflexias. When comparing the ratios between the normal and changed tests, no significant difference was evident. When comparing the normal and changed vestibular exams, with and without symptoms of walking disequilibrium and tinnitus, we had a significant diferent between the ratios.
BAYAZIT et al. (17) performed the vestibular evoked myogenic potential test -VEMP and they observed a significant alteration in the latency n23 and in the interpeak latency of waves p13-n23, demonstrating a relevant otoneurological involvement of this exam in fibromyalgia patients.
In the researched literature, with regard to the otoneurological aspect, we found a few studies to compare our findings with.
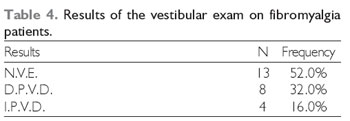
Legend: N - number of cases; N.V.E. - normal vestibular exam; D.P.V.D - deficit peripheral vestibular dysfunction; I.P.V.D - irritating peripheral vestibular dysfunction.
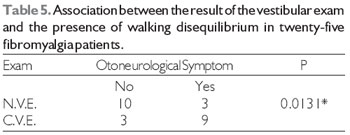
Legend: N.V.E. - normal vestibular exam; C.V.E. - changed vestibular exam.
When applying Fischer's Test, the significance level of 5% (á= 0.05) was considered, proving that there is a significant difference between the ratios of patients with normal vestibular exam (NVE) and changed vestibular exam (CVE) with and without a walking disequilibrium because p = 0.0131.
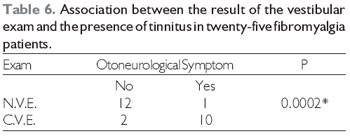
Legend: N.V.E. - normal vestibular exam; C.V.E. - changed vestibular exam.
1) The most evident otoneurological symptoms were: difficulty or pain during neck movements and pain spread to shoulder or arm (92.0%) in each, dizziness (84.0%) and headache (76.0%). And the most reported diverse clinical symptoms were: depression (80.0%), anxiety (76.0%) and insomnia (72.0%).
2) The change in the vestibular exam occurred in 48.0% of the patients, and it was found in the caloric test.
3) Alteration in the peripheral vestibular system was prevalent.
4) Deficit peripheral vestibular dysfunctions were prevalent.
This study allowed the importance of the labyrinthic exam to be checked, hence emphasizing that this type of population should be studied better, since several rheumatologic diseases can cause relevant vestibular alterations as a result of their manifestations and impairment areas.
REFERENCES1. Helfenstein M, Feldman D. Síndrome da fibromialgia: características clínicas e associações com ouras síndromes disfuncionais. Rev Bras Reumatol. 2002, 42(1):8-14.
2. Matsuda JB, Barbosa FR, Morel LJF, França ZC, Zingaretti SM, Silva LM, et al. Polimorfismos dos genes do receptor de serotonina (5-HT2A) e da catecol-O-metiltransferase (COMT): fatores desencadeantes da fibromialgia? Rev Bras Reumatol. 2010, 50(2):141-5.
3. Roberto M, Papt TR. Fisiopatologia da fibromialgia. Acta Fisiátrica. 2004, 11(2):78-81.
4. Jacomini LCL, Silva NA. Disautonomia: um conceito emergente na síndrome da fibromialgia. Rev Bras Reumatol. 2007, 47(5):354-61.
5. Alvares TT, Lima MEA. Fibromialgia: interfaces com as LER/DORT e considerações sobre sua etiologia ocupacional. Ciênc. Saúde Coletiva. 2010, 15(3):803-12.
6. Martinez JE, Domingues C, Davolos FJC, Martinez LC, Gozzano JOA. Fibromyalgia patients quality of life and pain intensity variation. Rev Bras Reumatol. 2008, 48(6):325-8.
7. Carneiro SCS. Fibromialgia e reação hansênica. Rev Bras Reumatol. 2006, 46(1):77-9.
8. Rezende LS, Rezende LS, Radominski SC, Paiva ES. A relevância da dosagem do hormônio estimulante da tireoide em pacientes com fibromialgia. Rev Bras Reumatol. 2006, 46(1):73-4.
9. Freire M, Teodoro RB, Oliveira LB, Cunha SFC, Ferreira BP, Borges MF. Concomitância de fibromialgia em pacientes portadores de hipotireoidismo e de alterações tireoideanas em pacientes com fibromialgia. Rev Bras Reumatol. 2006, 46(1):11-5.
10. Provenza JR, Pollak DF, Martinez JE, Paiva ES, Helfenstein M, Heymann R, et al. Projeto diretrizes - Fibromialgia. Sociedade Brasileira de Reumatologia, 2004. disponível em: http://www.unifesp.br/grupos/fibromialgia/fibromialgia.pdf.
11. Rosenhall U, Johansson G, Orndahl G. Otoneurologic and audiologic findings in Fibromyalgia. Scand J Rehab Med. 1996, 28:225-32.
12. Zeigelboim BS, Klagenberg KF, Liberalesso PBN, Jurkiewicz AR. Avaliação vestibulococlear na fibromialgia. Rev CEFAC. 2010, 12(4):677-82.
13. Mangabeira-Albernaz PL, Ganança MM, Pontes PAL. Modelo operacional do aparelho vestibular. In: Mangabeira-Albernaz PL, Ganança MM. Vertigem. 2ª.ed. São Paulo: Moderna; 1976. p. 29-36.
14. Bayazit YA, Gürsoy S, Özer E, Karakurum G, Madeci E. Neurotologic manifestation of the fibromyalgia syndrome. J Neurootol Sci. 2002, 196:77-80.
15. Hadj-djilani A, Gerster JC. Hearing and vestibular abnormalities in primary fibrosis syndrome Meniere´s disease and fibrositis syndrome. J Rheumatol. 1984, 1(5):678-80.
16. Gursoy S, Erdal E, Herken H, Madenci E, Alasehirli B, Erdal N. Significance of catechol-O-methyltransferase gene polymorphism in fibromyalgia syndrome. Rheumatol Int. 2003, 23:104-7.
17. Bayazit YA, Celenk F, Gunduz AG, Gunduz B, Ondag N, Meray J. Vestibular evoked miogenic potentials in patients with fibromyalgia syndrome. J Laryngol Otol. 2010, 124:610-5.
1) Doctor in Human Communication Sciences from UNIFESP/EPM. Assistant Professor of Phonoaudiology Degree, Coordinator of the Post-Degree Program in Communication Disorders and Head of Tuiuti University of Paraná's Vestibulometry Department.
2) Specialist in Clinical Audiology from Tuiuti University of Paraná.
Institution: Otoneurology Laboratory of Tuiuti University of Paraná (UTP). Curitiba / PR - Brazil. Mailing address: Bianca Simone Zeigelboim - Rua Gutemberg, 99 - 9º andar - Curitiba / PR - Brazil - ZIP Code: 80420-030 - Telephone: (+55 41) 3331-7807 - Email: bianca.zeigelboim@utp.br
Article received on December 14, 2010. Article approved on March 27, 2011.