INTRODUCTIONTinnitus is the sound perception without a source of external acoustic stimuli. It is highly prevalent, reaching approximately 50 million people in the United States (1). In Europe, this value is estimated between 7%-14% of population, and 1.0-2.4% of these people have a severe and debilitating tinnitus (1). It is known that tinnitus is a symptom, and it is present in several clinical affections (1).
The temporomandibular joint disorders (TMJD) are a term involving many clinical problems impairing the chewing muscles, temporomandibular joint and associated structures or both (2, 3). TMJD are very common in population, studies show that 50% of the population shows one or more TMJD signals (4-6). However, only 3.6-7.0% needs some kind of treatment (6).
The interaction between the otological symptoms - such as tinnitus - and TMJD is a subject having an old approach (6-9), which is complex and associated with different areas, e.g., medicine and dentistry. Such facts can be proven with works like those of COSTEN (1934) (9), and the current works performed by RAMIREZ et al (2005, 2007) (10-11). In TMJD patients, the presence of tinnitus ranges between 50 and 75% (5, 12-14), what makes a higher prevalence clear in these individuals in comparison with the general population (5-6, 15).
The etiologic factors, as well as the pathogenesis of this interrelation between tinnitus and TMJD have not yet been clearly defined (6,8,12), and there have been many theories intending to justify this correlation, like the one mentioning the existence of an anatomic relation between the auditory system and the stomagnatic system (10-12). Yet, as TMJD are frequent, these patients can equally show other affections that are causative of tinnitus.
Accordingly, this study has the objective of evaluating the event of TMJD treatment by a semi-qualitative scale, apart from its etiology.
METHODThe project of this work was submitted to the Ethical Committee and Research with Human Beings (CEPSH) at UFSC and approved under Record number 213/08.
It is about a longitudinal, prospective, uncontrolled study, which was performed in the occlusion ambulatory of the graduation degree of Dentistry at the Federal University of Santa Catarina and in the Department of Otorhinolaryngology and Surgery of Head and Neck at the University Hospital of the Federal University of Santa Catarina.
To complete this study, patients were selected at an age higher than 18, and they were admitted to start evaluation at the occlusion ambulatory of the graduation degree of Dentistry at the Federal University of Santa Catarina, in the period between October 08, 2008 and August 23, 2009, volunteer participants in the research.
In the present work, patients were included because they: 1) Agreed with the free and clarified agreement term 2) Were civilly over aged; 3) Had a temporomandibular joint disorder diagnosed by a specialist of the field; 4) Had the tinnitus symptom and 5) Had not started the dental treatment for TMJD until the moment of the first interview. Patients were excluded because they: 1) Quit their participation in the research; 2) Did not perform the audiometric exam; and 3) Did not finish the treatment proposed by the professional dentist.
At a first moment, at the time of admission consultation, it was performed an anamnesis by answering a questionnaire, in which items were evaluated, such as the patient's age, sex, how long the patient has tinnitus, characteristics of tinnitus - location of the symptom and degree of intensity, in which it was measured by providing the patient with a visual analogue scale (Figure 1), exposure to noises (habit of going to dance clubs, live music shows, use high sound earphones, exposure at work and use of individual protective equipment - IPE), co-morbidities (systemic arterial hypertension - SAH -, mellitus diabetes - MD -, previous otologic surgery, hospital stay, contact with ototoxic drugs). Next, bilateral otoscopy, anterior rhinoscopy and oroscopy were performed. Eventually, the dental diagnosis of TMJD was identified, and the diagnosis and the proposed treatment were recorded and, when questionnaire was finished, it was requested a pure-tone threshold audiometry and a vocal audiometry was performed at a later time, provided that it was before starting the treatment.
After finishing the dental treatment for TMJD - which lasted around 5 months -, the second proposed evaluation was performed, and it consisted in measuring the intensity of the tinnitus by the same visual analogue scale of the first evaluation. In the case of cerumen cork, it was removed before applying the scale.
To perform audiometry, the SIBELMED AC-50D equipment was used in an acoustic cabin with an earphone and an osseous vibrator to evaluate the auditory thresholds by airway at the frequencies of 250, 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz and by osseous pathways at the frequencies of de 500, 1000, 2000, 3000 e 4000 Hz.
To analyze the data, it was expressed in the form of absolute numbers and percentages. To calculate averages and standard deviation, as well as outline the graphics and tables herein, the tool Microsoft Excel 2007 was used. To analyze the values of the visual analogue scale before and after the treatment, Wilcoxon Signed Rank Test was used with the software GraphPad Prism 4 for Windows, version 4.02. A significance level of (p) equal to 95% (p<0, 05) was adopted, according to the standards used in biological studies.
RESULTSIn the present study, the first sample had 42 patients, however - when applying the exclusion criteria, mainly the criteria to quit the dental treatment and not perform the audiometry -, there were only 15 patients left.
Accordingly, 15 patients were evaluated and showed temporomandibular joint disorders and tinnitus, during the period between October 08, 2008 and August 23, 2009. The average age was 37, 73±17, 11, ranging between 18 and 73. In the Figure 2, we showed a distribution by sex.
The tinnitus time showed an average of 24 months, a percentile 25 of 19 months and a percentile 75 of 72 months. The tinnitus was unilateral in 9 (60.0%) patients and bilateral in 6 (40.0%) patients. Among the patients showing a unilateral tinnitus, the most impaired side was the right one (66.6%).
At Table 1, we introduce the patients according to age, sex and intensity of tinnitus, before and after TMJD treatment, provided by the visual analogue scale.
When comparing the visual analogue scale scores before and after the dental treatment by using Wilcoxon Signed Rank Test for paired samples, a significant decrease (p<0,001) in the intensity of tinnitus was verified. In 4 (26.6%) patients, tinnitus disappeared.
With respect to exposure to noise, 10 (66.66%) patients did not show any exposure and 5 (33.33%) patients did. Among the exposed patients, 1 patient reported a chronic exposure to dance clubs, live shows and hear high sound with an earphone; 1 patient mentioned exposure to dance club and hear high sound with an earphone; 1 patient showed only one exposure to dance clubs and, eventually, 2 patients mentioned only one exposure to noises at work (door manufacturing; and the other one, drilling the asphalt).
As to the co-morbidities, 3 (20.00%) of patients showed HAS - 1 patient was using atenolol only; 1 patient was using alpha-methyldopa, hydrochlorotiazide, enalapril and acetylsalicylic acid; 1 patient was using losartan. We did not find predecessors of ototoxicity, MD, previous otological surgery in our sample.
At the physical examination, 11 (73.33%) did not show any alteration, whereas in 4 (26.66) patients, the alterations described in Table 2 were noticed.
In relation to the pure-tone threshold audiometry, this one was normal in 10 (66.6%) patients, whereas in 5 (33.3%) patients, it was observed some degree of hearing loss, as described by Table 3.
In Figure 3, we show the distribution of the patients according their dental diagnoses of TMJD.
The treatment of temporomandibular joint disorders in all the patients was performed as a dental orthosis - Michigan plate - to be continuously used. For cases of muscle disorders with an intense pain, a non-hormone anti-inflammatory (AINH) and physiotherapy were associated, while in case of iatrogenic, the dental orthosis causing the problem was removed and, subsequently, Michigan plate was associated.
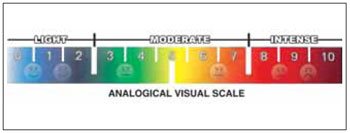
Figure 1. Visual analogue scale.
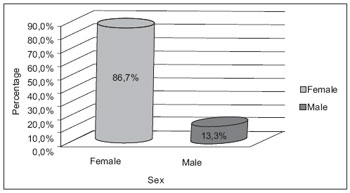
Figure 2. Distribution of patients according to sex.
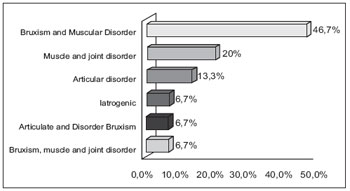
Figure 3. Distribution of patients according to dental diagnosis.
The relation between temporomandibular joint disorders and otological symptoms - such as tinnitus - is not thoroughly explained and clarified (1,3,7); its existence is very likely (1-2,5-7,11-13). Since the first half of the last century, it has been pursued to determine the etiology of the aural symptoms with TMJD, and anatomical, neurological and emotional associations have been verified (5-6), and the multi-cause hypothesis is still the most accepted in scientific environments (12-14).
According to the reviewed literature, it has been verified that, in the great majority of studies performed with patients having tinnitus and temporomandibular joint disorders, impairment prevailed in the female gender (1-2, 11, 13), as observed by ourselves.
As to tinnitus characteristics, in PARKER and CHOLE'S stud (1995) (9), a significant difference was not observed between unilateral and bilateral impairments, whereas, in our study, a prevailing unilateral tinnitus was observed. Regarding the impairment time length, WRIGHT and BIFANO (1997) (15) showed a range from 4 months to 40 years, and our statistics is compliant with the aforementioned work.
As to the effect of the temporomandibular joint disorder treatment over tinnitus, WRIGHT and BIFANO (1997) (15) evaluated TMJD patients showing tinnitus, and they noticed a significant improvement in tinnitus symptomatology after their temporomandibular joint disorder treatment. In 1998, GARANHANI (12) performed a literature review and noticed that the conservative treatment to manage temporomandibular joint disorder brings favorable results in the enhancement of otological symptoms like tinnitus.
WRIGHT and BIFANO (2000) (14), when studying patients with tinnitus, vertigo and otalgia of non-otologic causes and TMJD, they observed an improvement in tinnitus in 64% of patients after a conservative TMJD treatment. We also observed an improvement in a similar population; however, we did not exclude patients with audiometry audiometric alterations.
There is still TORII and CHIWATA'S case report (2007) (16), in which the patient reported aural symptoms to the right (tinnitus, otalgia, vertigo) with an unknown etiology, as well as severe pains when palpating on the right TMJ, and the symptoms were eliminated after her conservative TMJD treatment was performed.
De FELICIO et al (2008) (10) attempted to evaluate the frequency and the association between the otological and orofacial symptoms of TMJD, as well as the effect of the conservative therapy over the orofacial muscles. The authors achieved an improvement in tinnitus after the treatment, 20% of patients had tinnitus; yet, the authors did not mention the way the otological symptoms evolved.
BÖSEL et al (2008) (17), on the other hand, when performing a study with patients showing chronic tinnitus and TMJD, they did not observe an effect of the TMJD treatment over tinnitus and, consequently, they implied that the presence of tinnitus in patients with temporomandibular joint disorders would be but a coincidence.
However, URBAN et al (2009) (3), after reviewing literature, they observed the existence of a significant association between the otological symptoms and TMJD, as well as a reduction in these symptoms after several kinds of TMJD-treatment therapies had been performed, hence suggesting new studies with control groups, with a view to evaluating the correct etiology of this association.
The present study verified a significant improvement in tinnitus after performing conservative TMJD treatments. Among the factors that may justify such a result, we can emphasize that our case study has a lower average age, with a minimum exposure to noises and a presence of chronic diseases, and a few individuals have audiometric alterations, what must have reduced the presence of other affections as likely causes of tinnitus, besides the TMJD that must be regarded as a likely isolated or simultaneous etiology.
REFERENCES1. Silveira AM, Feltrin PP, Zanetti RV, Mautoni MC. Prevalência de portadores de DTM em pacientes avaliados no setor de otorrinolaringologia. Rev Bras Otorrinolaringol. 2007, 73(4):528-32.
2. Bruto LH, Kós AOA, Amado SM, Monteiro CR, Lima MATd. Alterações Otológicas nas Desordens Têmporo-Mandibulares. Rev Bras de Otorrinolaringol. 2000, 66(4):327-32.
3. Urban VM, Neppelenbroek KH, Pavan S, Alencar Junior FGPd. Associação entre otalgia, zumbido, vertigem e hipoacusia com desordens temporomandibulares. RGO. 2009, 57(1):107-15.
4. Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann of Otol Rhinol and Laryngol. 1934, 43:1-15.
5. Ramírez LM, Sandoval GP, Ballesteros LE. Los desordenes temporomandibulares: clinica craneo-cervicofacial referida. Med Oral Patol Oral Cir Bucal. 2005, 10:E18-E26.
6. Ramírez LM, Sandoval GP, Ballesteros LE. Síntomas óticos referidos en desórdenes temporomandibulares.Relación con músculos masticatorios. Rev Méd Chile. 2007, 135:1582-90.
7. Felício CMd, Faria TG, Silva MAMRd, Aquino AMCMd, Junqueira CA. Desordem temporomandibular: relações entre sintomas otológicos e orofaciais. Rev Bras Otorrinolaringol. 2004, 70(6):786-93.
8. Pascoal MIN, Rapoport A, Chagas JFS, Pascoal MB, Costa CC, Magna LA. Prevalência dos sintomas otológicos na desordem temperomandibular: estudo de 126 casos. Rev Bras Otorrinolaringol. 2001, 67(5):627-33.
9. Parker WS, Chole RA. Tinnitus, vertigo, and temporomandibular disorders. Am J Orthod Dentofac Orthop. 1995, 107(2):153-8.
10. De Felício C, Melchior M, Ferreira C, Rodrigues Da Silva M. Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. Cranio. 2008, 26(2):118-25.
11. Tuz H, Onder E, Kisnisci R. Prevalence of otologic complaints in patients with temporomandibular disorder. Am J Orthod Dentofacial Orthop. 2003, 123(6):620-3.
12. Garanhani RR. Sintomas otológicos na disfunção craniomandibular. [Monografia]. Florianópolis: Universidade Federal de Santa Catarina, Curso de Odontologia; 1998.
13. Mota LAA, Albuquerque KMGd, Santos MHP, Travassos RdO. Sinais e Sintomas Associados à Otalgia na Disfunção Temporomandibular. Arq Int Otorrinolaringol. 2007, 11(4):411-5.
14. Wright EF, Syms CA 3rd, Bifano SL. Tinnitus, dizziness, and nonotologic otalgia improvement through temporomandibular disorder therapy. Mil Med. 2000, 165(10):733-6.
15. Wright E, Bifano S. Tinnitus improvement through TMD therapy. J Am Dent Assoc 1997; 128: 1424-32.
16. Torii K, Chiwata I. Occlusal management for a patient with aural symptoms of unknown etiology: a case report. Journal of Medical Case Reports. 2007, 1:85.
17. Bösel C, Mazurek B, Haupt H, Peroz I. Chronischer Tinnitus und kraniomandibuläre Dysfunktionen: Einfluss funktionstherapeutischer Maßnahmen auf die Tinnitusbelastung. HNO. 2008, 56:707-13.
1) Junior Doctor in Otorhinolaryngology at Hospital do Servidor Público Municipal de São Paulo. Junior Doctor.
2) Doctor in Otorhinolaryngology from the University of São Paulo. Assistant Professor of UFSC's Surgery Department.
3) Doctor in Dentistry from Federal University of Santa Catarina. Assistant Professor of UFSC's Dentistry Department.
4) Junior Doctor in Clinical Medicine at Hospital Regional de São José Dr. Homero de Miranda Gomes. Junior Doctor.
5) Junior Doctor in Otorhinolaryngology at EPM-UNIFESP. Junior Doctor.
6) Master in Otorhinolaryngology from Pontifícia Universidade Católica do Rio de Janeiro. Assistant Professor of UFSC's Surgery Department.
Institution: Federal University of Santa Catarina - UFSC. Florianópolis / SC - Brazil. Mailing address: Guilherme Webster - Rua Castro Alves - 355 - Bairro aclimação - São Paulo / SP - Brazil - ZIP Code: 01532-001 - Telephone: (+55 11) 6953-9011- Email: guilhermewebster@uol.com.br
Article received on April 1, 2011. Article approved on May 21, 2011.