INTRODUCTIONProfuse nasal bleeding due to craniofacial trauma important are commonly associated with fractures of the facial bones and skull base (1). Several of these control techniques are described epistaxis, and the posterior tapenade with a Foley associated with anterior packing one of the most used, both by the relative ease of the procedure as the wide availability of materials (2).
We report a case of using Foley catheter to control bleeding nose after polytrauma outcome with a severe and unusual.
CASE REPORT50 year-old-man crashed presenting high loss of consciousness, deformity of the face and profuse nosebleeds. It was attended by emergency services and taken to the nearest hospital. Pa ¬ kept you lowered level of consciousness during the service showing score 6 Scale Glasgow. The measures were supportive, stabilizing the airway by endotracheal intubation, volume resuscitation, and stabilization of the cervical spine, posterior nasal tampanomanto with Foley catheter in the left nostril and bilateral anterior gauze, which is effective. Performed plain radiographs of the cervical spine and face which was evidenced in facial bone fractures. Patient developed worsening of clinical well being routed to the larger hospital after stabilization.
Performed computed tomography, facial bones and cervical spine which showed multiple fractures in the bones of the face and skull base as well as fracture of the odontoid process of the 2nd vertebra. Also evidenced intracerebral migration of Foley catheter with path to the posterior portion of the right parietal lobe through the ethmoid fracture. (Figure 1)
Patient underwent craniotomy after 48 hours of trauma for drainage of subdural hematoma, viewing the withdrawal of the probe and control bleeding in his path. Patient referred to intensive care being kept sedated and on controlled breathing. Showed clinical improvement and neurological stimuli when responding to reduced sedation.
Due to nasal drainage of cerebrospinal fluid with high flow underwent endoscopic sinus surgery on the 10th day of hospitalization for closing cerebrospinal fluid fistula high output in the ethmoid sinus, the migration path of the probe.
The patient developed mild neurologic improvement, keeping vigil with important cognitive and left hemiplegic. Released from the intensive care unit on the 39th day of hospitalization being held in ward with tracheotomy and device pressure continuous positive airway pressure (CPAP) pending clinical stabilization after 3 episodes of pneumonia, for realization of fracture fixation on process odontoid.
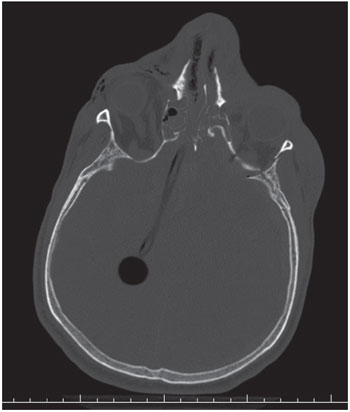
Figure 1. Axial CT scan of the skull showing through penetration of the ethmoid bone fracture path and intra cerebral Foley catheter.
Severe cranial trauma with changes in facial architecture, require special attention, by signposting high impact injuries and also by the common association with skull base fractures (3). The management of severe epistaxis associated with these fractures requires care possible weakness of this nasal wall.
The techniques of posterior tapenade with Foley catheter associated with anterior packing are widely discussed and generally do not differ greatly in the literature, but the actual mechanism of action is not consensus. The main theses are that compression in the rear walls of the nasal cavity cause occlusion of bleeding vessels of the balloon would only serve as a platform to support effectively the above buffer containing bleeding or a combination of these mechanisms (2).
The allocation of the Foley catheter in these situations becomes critical because during the procedure does not need to have a portion thereof inserted into the nasal cavity, thus causing errors in positioning. In this case the insertion should be done under direct vision / indirect probe, where the floor of the nasal cavity, and confirmation of the presence of the same in the oropharynx before inflating the balloon are essential as is the use of larger diameter catheter possible (4) .
Just as in the allocation of other probes to confirm the position with imaging test imposes greater security and the lateral skull radiograph usually enough to confirm this.
In the medical literature there described 3 cases of intracranial migration of Foley catheter during packing later, all related to profuse epistaxis after severe craniofacial trauma and restricted to anterior and middle tank (3, 4, 5). In our report but the probe maintained a straight path being positioned in the left parietal lobe.
Other reports of nasogastric tube after penetrating trauma, surgery on the skull base and also not related to trauma are described, demonstrating the anatomy of the region of weakness (6, 7, 8).
CONCLUSIONThis is a rare but possible complication in the treatment of severe nose bleeds associated with fracture of the skull base. This brief report highlights the risks related to the method and suggests some care to prevent complications, the main one being to verify the presence of the balloon probe oropharynx before the final positioning of the probe.
REFERENCES1. Hartley C, FRKD, Axon PR, MB, BS. The Foley catheter in epistaxis management - a scientific appraisal. Journal of Laryngology and Otology, 1994;108: 399-402.
2. Lee WC, Ku PKM, Hasselt CA. Foley Catheter Action in the Nasopharynx. Arch Otolaryngol Head Neck Surg, 2000;126:1130-1134.
3. Pawar SJ, Sharma RR, Lad SD. Intracranial migration of Foley catheter - an unusual complication. Journal of Clinical Neuroscience, 2003;10(2):248-249.
4. Woo HJ, Bai CH, Song SY, Kim YD. Intracranial placement of a Foley catheter: A rare complication. Otolaryngology-Head and Neck Surgery, 2008;138:115-116
5. Blasco V, Heng Ban L, Velly L, Leone M, Gouin F. Brain placement of a duble balloon catheter after extensive craniofacial trauma. Annales Françaises d´Anesthésie et de Réanimation, 2008;27:843-845.
6. Arslantas A, Durmaz R, Cosan E, Tel E. Inadvertent insertion of a nasogatric tube in a patient with head trauma. Child's Nerv Syst, 2001.17:112-114.
7. Pandey AK, Sharma Ak, Diyora BD, Sayal PP, Ingale HA, Radharkrishnan M. Inadvertent Insertion of Nasogastric Tube into the Brain. JAPI, 2004;52:322-333.
8. Genú PR, et al. Inadvertent Intracranial Placement of a Nasogastric Tube in a Patient With Severe Craniofacial Trauma: A Case Report. J Oral Maxillofac Surg, 2004;62:1435-1438.
1) President of the Brazilian Society of Laryngology and Voice (2001-2003). Director of the Center for Otolaryngology and Head and Neck of St. Paul.
2) Doctor in Otolaryngology, Faculty of Medicine, USP - Ribeirão Preto. Physician Assistant at the Center for Otolaryngology and Head and Neck of St. Paul.
3) Medical (a). Resident Center for Otolaryngology and Head and Neck of St. Paul.
Institution: Center for Otolaryngology and Head and Neck of São Paulo. São Paulo / SP - Brazil. Address for correspondence: - Alameda Nhambiquaras, 159 - Moema - São Paulo / SP - Brazil - Zip code: 04090-010 - Telephone: (+55 11) - 5573-1970 - E-mail: japorl@uol.com.br
Article submitted on August 18, 2010. Approved on October 24, 2010.