INTRODUCTIONAmong the highly organized tissues, bone has only one potential of rebuilding its original structure after a defect or fracture. In unstable conditions, direct or secondary cicatrisation is predominant, through intermediate formation of fibrocartilage followed by endochondral ossification. In stable conditions, bone is formed in a direct or primitive way, showing that two fundamental conditions should be performed: large blood supply and a solid base for bone deposit (1).
Though regenerative capacity of the bone is limited by lesion dimension, in such a way that extensive bone defects, caused by trauma, tumors, infections and anomaly of development, do not regenerate themselves spontaneously, representing a challenging problem to scientific community (2).
The orbit floor fractures frequently promote great bone defects that demand the use of grafts and/or implants for its reconstruction. Several materials were already used for this purpose (septal and conchal cartilage, silicon, among others).
Sclera is the external, thick, white, fibrous and highly resistant layer of the eye, which protects it. It is continuous to anterior cornea and to optic nerve with dural covering. Human sclera can be used as a barrier material in orbit floor fractures because it is present in large number in hospitals after the removal of donated corneas.
As bovine sclera is histologically similar to human sclera, we have made this study with the purpose of evaluate the efficiency of bovine sclera as barrier material for standard-fracture programmed on orbit floor of rabbits, avoiding fat herniation, rectus muscle, ocular viscera, through behavior study of biocompatibility.
MATERIAL AND METHODSExperimental AnimalsAs rabbits offer easy control of variables as age, sex, weigh, hygiene, maintenance, and are easily handled, it was used 18 isogenous rabbits from New Zealand (Qryctolagus cuniculus), albin, males, raging from six to eight months of age, weighing about 2.8 Kilos, and were provided by Veterinary Lab of Universidade Federal de Uberlândia (UFU-MG).
Groups of Study DefinitionIn this clinical trial, animals were randomly distributed in 2 groups of 9 animals each, according to used material. After surgery experiments being made in each group, both were again subdivided into three other groups of 3 animals in each to histopathologic evaluation in different dates (30, 45 and 60 post surgery days) which might express tissues compatibility, possible immunologic reaction and, consequently, bone repairment.
GI (experiment): 9 rabbits with standard bone defect in left infraorbitary border and filled with bovine sclera (subdivided in GI-30, GI-45, GI-60).
GII (experiment): 9 rabbits with standard bone defect in right infraorbitary border and filled with block of silicon (subdivided in GI-30, GI-45, GI-60).
Surgeries and post-surgery period were made at Laboratory of Surgery Technique of Veterinary Hospital (UFU-MG).
Implant PreparationSix ocular globes were taken off and stored in a glass container previously sterilized containing alkaline solution. After some time, sclera was separated and conserved in glycerin as dura-mater, corneas and cartilage are maintained to posterior use as implant (4) (Picture 2).
Silicon as much as bovine sclera was prepared with standard measure of 1cm of length X 0.5cm of width X1mm of thickness, and then isometry between the implants was made (Picture 3).
Post-Surgery ProceduresOnce anaesthetized, animals were laid on their side on the operating table. Bone defects were made using drill (troncoconic of steel no. 703 - to flat piece). Standard bone fracture was made with 1mm of thickness (diameter of the most calibrous portion of active extremity of the drill) and 5mm of length (active extremity measure of the drill in its long axis) (Picture 4).
Using the same drill, it was made two equidistant perforations on fracture borders (2mm) in order to make attachments of bovine sclera and hard silicon, using steel wire 2-0 in the orbit floor keeping them in this form in situ (Picture 5). Skin synthesis was made with intradermic suture with Mononylon 4-0 and afterwards with some simple stitches as complementary security procedure.
Collection and Preparation of Material for Morphological ExamAfter observation period of 30, 45 and 60 days, animals were submitted to anaesthesia similar to post surgery act, followed by intravenous injection of Potassium Chloride 19.1%, in 2 ml proportion and sodic thiopental 1.0g, leading to euthanasia.
After that, it was made and surgery procedure through division of soft tissue and osteonomy to remove bone block of the orbit floor with implant.
After a period of 48 hours, obtained pieces were bathed in running water in order to remove the excess of fixation agents (10% tamponed formol) and then, a decalcification process started. Pieces were immersed in decalcification solution of EDTA (ethylenediaminetetraacetic) 5.5g, 90ml of water and 40 ml of formol at 37-40% to remove mineral part of mineralized bone matrix. Six days later, pieces were bathed in running water in order to remove EDTA and be submitted to dehydration in etilic alcohol (70%, 90% and 100% consecutively), diafanization in soap and penetration in histological paraffin (5).
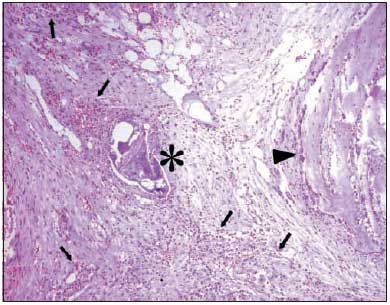
Blocks were sectioned with microtome, adjusted in 5 mm of thickness and cuts were semi-seriated in lateral direction. Laminas obtained from decalcification bone matrix were colored with hematoxylin and eosin and observed at optic microscope.
Clinical and Macroscopic Analysis Results were statistically clinically analyzed concerning presence of erythema, oedema, secretion, hematoma or bruises, in orbit region (conjunctive and sclerotic) and in skin in the infraocular area. Clinical evaluation at the end of 30, 45 and 60 days also considered the presence of erythema, necrosis, oedema, adherence and if there was incorporation of the material to the bone or conjunctive tissue in the local. These records were based on a semi-quantitative evaluation, considering (0) absent, (+) light, (++) moderate or (+++) intense.
Microscopic EvaluationImplants were evaluated histologically by hematoxylin and eosin color, through optic microscope of visible light and with more suitable amplifications for each observed item. In this analysis, it was considered:
1. Cell inflammatory infiltrates composition, classifying them as acute (composed by neutrophils) and chronic (composed by lymphocytes, plasma cells and macrophages considered in group or separately) (6).
2. Infiltrate intensity, measured from evaluation and its intensity: (0) absent; (+) light; (++) moderate; (+++) macroscope.
This evaluation was a comparative feature between the two tested groups in relation to the dynamic of process formation of bone repairment. The results were expressive according to the criteria described above and also they were represented by photomicrography of the expressive areas.
Ethics CommitteeThe current study was approved by Ethics Committee on Animal Use (CEU/UFMS), on December 15, 2003, agreeing on ethic principles followed by Colégio Brasileiro de Experimentação Animal - COBEA (Brazilian Institute of Animal Experiment).
RESULTSGeneral aspects in post-surgery period
Animal endured anaesthesia and surgery act with no record of occurrences either in pre, trans or post surgery period. During post-surgery follow-up of the two groups (Silicon and Bovine Sclera) no signs of immediate or late post-surgery were recorded. All animals presented discrete oedema (+) in post-surgery period.
Macroscopic ObservationsTable 1 displays macroscopic observations of the bone blocks of orbit floor in rabbits including implants of Silicon and Bovine Sclera with 30, 45, 60 days.
Microscopic ObservationGraph 1 displays microscopic evaluations comparing the silicon group and the bovine sclera one at 30, 45, and 60 days.
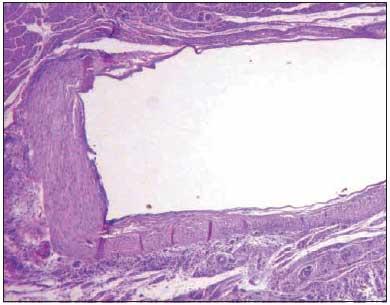
Pictures 6 to 11 give details on microscopic observation from all groups.
DISCUSSIONDifferent and multiple materials have been used in orbit fracture correction, they are: silicon, Teflon, supramid, polyethylene (Porex), bone, autogenous cartilage, hydroxyapatite, etc (3). Ideal graft would be the one which had consistence and resistance of defective structure. It should be easily obtained and molded, and of low cost. Moreover, it should cause minimum tissue reaction to extrusion and to reabsorption by the body (7).
Researching literature, we observed large quantity of works on partial or total rebuilding of human organism. When we chose sclera for our search, we analyzed its advantages on this range of biocompatible materials, such as cost to hospitals and to patient, because sclera is donated together with cornea. Besides, it is an easily acquired material for its large quantity in registered hospitals to receive or withdraw corneas from donors. Another property of sclera is the easy manipulation to be remolded, adapted and attached to receiving surface. Its conservation is done in glycerin 98%, what keeps cell integrity (4, 8, 9).
We studied human sclera to fit it in biomaterials as well. During the study, we observed that in the group of animals with bovine sclera good adaptation, attachment and accommodation on receiving surface, no displacement of sclera and easily modeled as the anatomy of receiving area.
Silicon was chosen as material for the control group for being an implant extensively studied in traumatic enophthalmos. Its disadvantage is that it can be visible over skin, even after being modeled, besides, it can occur expelling from the receiving surface (3, 7). In relation to our researched material, for being organic, they do not have such disadvantages. They are easily attached with different surgery wires.
Skin is another implant used in large scale in exenteration (surgical removal of the organs within a body cavity), though having two expressive disadvantages: a) possible hair development; b) possible secretion production (7). Such disadvantages do not exist in implant with sclera.
In the study of conjunctive subcutaneous tissue reaction to human acellular dermis implantation (Alloderm®) and membrane of polytetrafluorethylene (Teflon) in rats, was verified that in late period (90 days) Teflon presented fibrous formation and capsule, without inflammatory reaction. However material is expensive to hospital and patients (8).
In the research of development of autogenous and alogenous bone grafts placed in bone defects of critical size in calvaria of guinea-pigs, Urist et al. (9) showed that osteoinductive and endochondral factors induce bone formation going through hyaline cartilage period. Referring to the results of our studies with bovine sclera, we can also agree on the existence of an osteoinductive substance, though, besides it works as barrier, it permitted bone formation at the end of the research.
A study was done using human sclera and polytetrafluorethylene as alternative material on treatment of sclera perfuration in rabbits. Evolution of post-surgery period of animals was daily analyzed during one month, classifying intensity of ocular hyperaemia in the following categories: O (absent), + (light hyperaemia), ++ (moderate hyperaemia) and +++ intense hyperaemia), moreover the presence or absence of ocular secretion (10).
In our study we use bovine sclera on programmed fractures on orbit floor in rabbits. The presence of inflammation (+++) on the bovine sclera group in the period of 30 and 45 days - what remained (++) at the end of the research - is possibly related to the use of implant (sclera) in its natural from. Despite all that, it demonstrated similar features to homologous sclera used for correction of diverse lesions in scleras.
Implants of ferromagnetic platelets on rabbit sclera were studied with the purpose of nystagmus neutralization and achievement of normal ocular position after strabismus correction and mainly its stabilization. This research evaluated inflammatory intensity in the following way: two independent observers used the following standards for the evaluations: -: absent; + present, but discreet; ++: moderate; +++: stressed; Conjunctive Secretion: absent (a); or present (p); Presence of nerves: absent (a) or present (p). In this study inflammatory reaction remained up to 28th day (11). In our study with bovine sclera, we had the presence of inflammatory process in light condition up to the group of sacrificed animals with 60 days (last sub-group of the research).
In the research with bovine sclera in its natural form, we basically concluded that the material is easily handled, adapted and molded on the receiving area. It worked as barriers, though at the end of 60 days it became fibrous and enabled bone formation on the side of the programmed standard-fracture.
Programmed standard-fracture at 60 days in the control group (silicon), was already closed while in research group (bovine sclera) was not. Bovine sclera showed that it will be able to join the biomaterial group. Though other studies will fit it in a research line to be thoroughly tested. According to Medawar "Freezing and lyophilisation are methods apparently able to destroy particles and cell vitality, decreasing immunologic capacity of graft (implant) and preserving the matrix in an intact form for a future graft (implant)" (12). Freezing and lyophilisation of the material is a natural step of the study of this graft in orbit fractures.
CONCLUSIONSIt is concluded that, in programmed fractures on orbit floor in rabbits, both implanted materials were biocompatible, causing discreet clinical oedema in the beginning and non-specific granulomatous chronic inflammatory reaction which disappeared at 60 days (more quickly in control group with silicon implant). Besides, they enabled partial bone regeneration during studied period (60 days), not being reabsorbed and working as barrier material against herniation of orbit material for maxilla.
REFERÊNCIAS BIBLIOGRÁFICAS 1. Schenk RK. Regeneração óssea: bases biológicas. In: Buser D, Dahlin C, Schenk RK. Regeneração óssea guiada na implantodontia. 2.ed. São Paulo: Quintessence; 1996. p. 49-100.
2. Mendonça JCG. Estudo morfológico comparativo do enxerto ósseo autógeno e o polímero de mamona em rebordo infra-orbitário em coelhos. 47 f. 2004. Dissertação (Mestrado em Ciências da Saúde) - Faculdade Federal de Campo Grande - Mato Grosso do Sul. 2004.
3. Junqueira LC, Carneiro J. Histologia Básica. Rio de Janeiro; Gunabara Koogan; 1995.
4. Sousa CJA, Loyola AM, Versiani MA, Biffi JCG, Oliveira RP, Pascon EA. A comparative histological evaluation of the biocompatibility of materials used in apical surgery. Int Endodont J 2004;37(10):1-11.
5. Portelinha WM, Couto Jr. AS, Moura EM, Zenha JC, França VP, Gonçalves JOR. Fraturas orbitárias. In: Soares EJC, Moura EM, Gonçalves JOR. Cirurgia plástica ocular. São Paulo: ROCA; 1997. p. 426-46.
6. Patrocínio LG, Patrocínio JA. Atualização em enxertos na rinoplastia. Rev Bras Otorrinolaringol 2001;67(3):394-402.
7. Ramos RQ. Reações do tecido conjuntivo subcutâneo aos implantes de derme humana acelular (Alloderm®) e membrana de politetrafluoretileno não expandido (teflon). Estudo histológico em ratos. 129 f. 2001. Dissertação (Mestrado em Cirurgia e Traumatologia Buco-Maxilo-Facial) - Faculdade de Odontologia - Universidade Estadual Paulista, Araçatuba. 2001.
8. Koenig SB, Sanitato JJ, Kaufman HE. Long-term follow-up study of scleroplasty using autogenous periosteum. Cornea 1990;9(2):139-143.
9. Florian A, Cohn LH, Dammin GJ, Collins JJ Jr. Small vessel replacement with gore-tex (expanded polytetrafluoroethylene). Arch Surg 1976;111(3):267-70.
10. Utrilla JC, Martín-Lacave I, San Martín MV, Fernández-Santos JM, Galera-Davidson H. Expression of c-erbB-2 oncoprotein in human thyroid tumours. Histopathology 1999;34(1):60-65.
11. Abreu SLDR, Bicas HEA. Estudo comparativo entre técnicas cirúrgicas para fixação de placa metálica em esclera de coelhos. Arq Bras Oftalmol 2002; 65(2):177-181.
12. Medawar PB. Transplantation immunity and subcellular particles. Ann NY Acad Scienc 1957; 68(2):255-67.
Picture 1

Picture 2

Picture 3

Picture 4
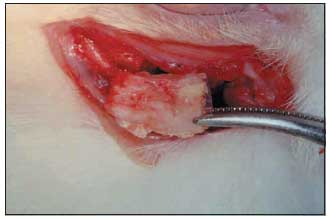
Picture 5
Picture 6
Picture 7
Picture 8
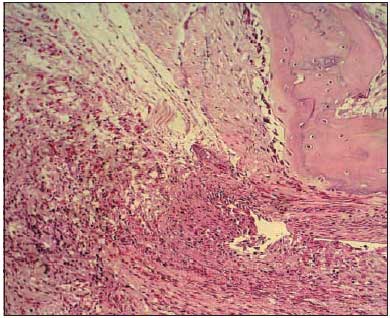
Picture 9
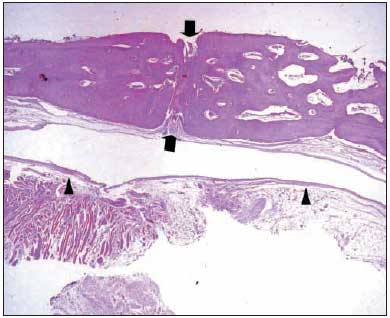
Picture 10
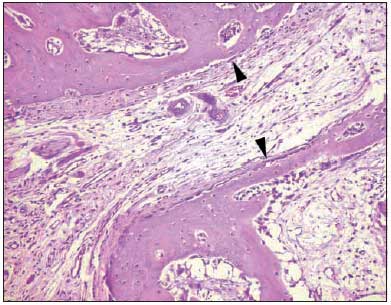
Picture 11
Table 1 - Macroscopic observation from alterations of the bone blocks removed from receptive area of implants with 30, 45 and 60 post-surgery days.
Graph 1 - Microscopic evaluation comparing silicon group and bovine sclera at 30, 45, and 60 post-surgery days.