INTRODUCTIONWhile unilateral peripheral facial palsy (PFP) is a common disorder with an incidence between 12 to 25 cases per year for each 100.000 habitants, simultaneous bilateral facial palsy is a rare disease, which correspond less than 2% of the facial palsy cases (1). Its incidence is of one case in five millions of people a year (2). Its occurrence is from 7 to 12% of the cases of unilateral PFP, being more common in the opposite side, while the occurrence of bilateral PFP is very rare (1, 2).
Opposite unilateral facial palsy, in which the majority of the cases do not present definite etiology, with Bell´s idiopathic palsy diagnosis in even 80% of the cases, bilateral palsy usually presents definite etiology. Only 25% of the cases are assigned to Bell´s palsy. In this way, it is fundamental the investigation of bilateral PFP by larger risk of association with other diseases (3, 4).
Patients with HIV positive often presents otologic and neurotological manifestations, what means that facial palsy can occur in any stage of the disease, inclusively as first manifestations (5). Bell´s palsy is responsible for the majority of the cases, usually occurring in non-symptomatic patients (5,6).
The target of this study is to describe the case of a patient with HIV that developed severe bilateral peripheral facial palsy associated to a herpetic lesion condition in oral cavity; and also to revise the literature on the topic, discussing the aspects related to etiology and investigation of bilateral PFP.
CASE REPORTA 35-year-old patient, male, with HIV diagnosis and having a follow-up at the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), reports appearance of vesiculosus lesions in upper lips and aphthous lesions jugal mucosa for 8 days, followed by clinical condition of viral prodrome. He was taking Aciclovir topical. Before that he had already presented labial herpes in the past. Three days after the appearance of labial lesion, he developed bilateral peripheral facial palsy, in a sudden way, symmetric and apparently without developing factors. The patient did not report any current and previous otologic complaint and also previous facial palsy.
As important personal antecedent, the patient presents HIV diagnosis since 1990. It is probably by sexual transmission, being regularly medical assisted and with no antiretroviral therapy (CD4/CD8 stable, with low rate of viral reapplication). He reports history of pulmonary tuberculosis treated 4 years ago. He denies history of diabetes mellitus, contact with tick, parotideo bulging and trauma.
At physical exam he presented symmetric bilateral peripheral facial palsy, grade V, according to classification of House-Brackman (7) (Picture 1). In oroscopy, crustous lesion presence on upper lips and aphthous lesion in jugal mucosa in bilateral way could be noticed. He did not presented ear lesion, with external acoustic meatus and tympanic membrane without alterations. Cervical palpation was normal, and did not present alterations in neurological exam from other cranial pair.
The patient was admitted with diagnosis of Bilateral PFP, and went to hospital for diagnosis investigation and clinical treatment, taking Aciclovir 600mg EV every 8 hours and dexametason 8mg/day.
Hemogram exams, hepatic function tests and electrolytes showed normal results. Serologies for syphilis, Lyme disease and hematological tests presented negative results.
Audiometry presented moderate symmetric sensorineural hearing loss in acute frequencies, similar to previous audiometry from the year 2000. Tympanogram showed normal results and presented reflex absence in a bilateral way.
It was requested a cranial magnetic resonance imaging which showed facial nerve with normal course, calibration and distinction, with internal ear structures preserved (Pictures 2 and 3).
After 4 weeks of development, the patient showed important improvement in palsy on both lips, degree 3 (7). After 6 months, he presented complete improvement of palsy, preserving only with synkinesis.
DISCUSSIONBilateral PFP is a rare disease and usually associated with systemic quadro, and should be carefully investigated before establishing diagnosis of Bell idiopathic palsy (4).
Different diagnosis is extensive, varying from idiopathic causes as Bell´s palsy, Melkersson-Rosenthal, syndrome of Guillain-Barret, multiple cranial neuropathy; infectious as Lyme disease, herpes zoster, neuropathy by HIV, syphilis, mononucleosis, cyomegalovirus, bilateral medium otitis, bacteria meningitis; neoplasic such as leukosis, lymphoma and cerebellum-point angle tumors. Other possible causes are metabolic diseases as diabetes, cranial traumatism, malformations as Möbius syndrome and uncertain etiology diseases as sarcoidosis, vasculitis, and so forth (1-3).
Lyme disease is reported to be the main infectious cause of bilateral PFP, reaching up to 39% of the cases, though its incidence can vary (1,4). In Brazil, its real incidence is unknown, though there are some reported cases of the disease in the Great São Paulo and at the seaside of São Paulo State and Florianópolis and in Morro Branco (RN) (8). Curiously, it occurs especially in tourists and always around vegetation area. It was reported the case of a patient, in Cotia (SP), with bilateral PFP associated to sudden deafness, treated with erythomycin, developing with comprehensive regression of PFP, but with no improvement of hypoacusis (9).
Disease is caused by spirochete, Borealis burgdorferi, whose carrier is a common tick (9). Lyme disease is a polymorphic infection, with clinical development and manifestations which can vary. Its incubation period ranges from 3 to 32 days. The first manifestation is usually cutaneous rash (erythema chronic migrans), associated to viral prodrome symptoms (stage 1). After some weeks or months, patients can present neurological and cardiac quadro; and migration myalgia is common in this stage (stage 2). Patients can also present meningoencephalitis, multiple cranial neuropathy, and radiculoneuritis. Tipically they present symptoms uncertain of meningitis, followed by PFP and peripheral radiculoneuritis. Third stage can occur either after some weeks or years from initial quadro, developing with monoarthritis (60% of patients), cutaneous (acrodermatitis chronic atroficans), or neurological (8, 9).
PFP occurs in 10% of patients with Lyme disease, bilateral one in 30% of the cases. Prognosis of palsy is good, with comprehensive recovering in most of cases. Patients with associated neurological quadro and bilateral PFP present worse prognosis. On the contrary of Bell´s palsy, which is more common in adults, Lyme disease is more common in children. Diagnosis is serologic, and antibodies of IgM category increase in the second week and tend to decrease with treatment, while antibodies of IgG category appear late with reaching its top in the second or third month, and it can indefinitely remain positive (9). The recommended treatment is antibiotic therapy, and tetracycline can be an option. Penicillin and erythromycin can also be used (8). As in the reported case the patient presents negative serology but does not present history of contact with tick or previous air trip to endemic areas, the diagnosis was rejected.
Guillain Barret syndrome (GBS) is an inflammatory post-infectious polyrradiculoneuritis of uncertain etiology. IX, X and VII are cranial pairs with more occurrences in the order of frequency. Bilateral PFP can occur in even 50% of the cases, associated to the worst prognosis. O quadro típico is dysphagia with dysarthria, followed by areflexia and ascending motor palsy. Diagnosis is done through lumbar puncture, what shows liquoric dissociation: normal cell number and high protein (1, 3). In the reported case, GBS was rejected by the absence of other neurological signs.
Patients with HIV can present PFP in any developing period of the disease, though it is more frequent in non-symptomatic patients (10). PFP can even precede the appearing of the disease. In non-symptomatic patients, it occurs as Bell´s palsy or as region manifestation of Guillain Barret syndrome. In immune depressed patients, in more advanced stage of the disease, PFP can also occur by infection of herpes zoster. In these cases, PFP can be unilateral, associated cutaneous eruption, or bilateral, as a consequence of herpetic meningoencephalitis. Besides, immune depressed patients present PFP as consequence of HIV, by chronic neuropathy associated to virus, or even associated to lymphoma not Hodgkin, it is usually secondary to meningea dissemination. In these cases, diagnosis is done through liquor exam (5, 6).
As in the reported case, patient presented high level of CD4/CD8 without antecedent of infection by zoster. Liquor exam was not done. However, palsy could be associated to neuropathy by HIV.
Neoplasy is caused by bilateral PFP, usually secondary to meningea dissemination. Although pontine tumor can develop with bilateral PFP, leucosis and lymphoma are more frequent neuplasies (1, 5, 11). Thus, it is fundamental the accomplishment of a hemogram when investigating cases of facial palsy, especially in patients with HIV and in children. The hemogram in reported case is normal and the RNM exam did not show any expansive or infiltrative lesions of cranial base.
Bell's palsy is responsible for about 25% of the cases de Bilateral PFP (1). Its etiology is still uncertain and discussed. Some authors suggest the association with Herpes simplex. In this way, PFP could occur as possible reactivation of latent virus on geniculate ganglion (12). Bell diagnosis is one of exclusion, which should be done after careful investigation, especially in Bilateral PFP. Bilateral Bell's palsy prognosis as well as the unilateral palsy, is favorable in most of the cases. Recovering of function usually occurs in one side first; the recovering of the opposite side can occur weeks or months later (4).
There a patient reports with Bilateral PFP associated with herpetic stomatitis (13) and genital herpetic infection, although most cases of idiopathic PFP is not associated to oral lesion (14). In the case reported, bilateral PFP manifestations occurred after labial herpes, reinforced its possible association with PFP.
In RNM it can be observed an increase in contrast captação by fácil nerve in patients with Bell, possibly secondary to local inflammatory process, with oedema and vascularization increase (15). Some authors also suggest that RNM could be used as prognostic exam, where contrast captação in mastoidea portion of the nerve would be the indication of the worst prognosis (15). Contras captação can also be observed in patients with Lyme and Herpes Zoster (14). It was no observed anomalous captação of contrast in the reported case.
After negative laboratory and radiologic investigation, Bell's palsy and neuropathy related to HIV cannot be rejected as possible differential diagnosis. By the chronological association of bilateral PFP appearing with labial herpes, we believe that this can be related with quadro.
FINAL COMMENTSBilateral PFP is a rare event often associated to systemic diseases. We cannot avoid mentioning the importance of laboratory and radiologic investigation in all cases, especially in HIV positive patients. Although we need more evidences, we also report a possible association between herpes simplex and bilateral facial palsy.
BIBLIOGRAPHY1. Keane JR. Bilateral seventh nerve palsy: analysis of 43 cases and review of the literature. Neurology 1994, 44: 1198-2002.
2. Teller DC, Murphy TP. Bilateral facial paralysis: a case presentation and literature review. J Otolaryngol 1992, 21: 44-47.
3. May M, Klein SR. Differential diagnosis of facial nerve palsy. Otolaryngol Clin North Am 1991, 24: 613-645.
4. Price T, Fife DG. Bilateral simultaneous facial nerve palsy, J Laryngol Otol 2002, 116: 46-8.
5. Linstron CJ, Pincus RL, Leavitt EB, Urbina MC. Otologic neurotologic manifestations of HIV-related disease. Otolaryngol Head Neck Surg 1993, 108: 680-7.
6. Casanova-Sotolongo P, Casanova-Carrillo P. Asociación de paralysis facial periférica en pacientes con infección por el virus de la inmunodeficiencia humana. Rev Neurol 2001, 32: 327-330.
7. House JW. Facial nerve grading systems. Laryngoscope 1983, 93:1056-9.
8. Yoshinari NH, Barros PJL, Bonoldi VLN, Ishikawa M, Battesti DMB, Pirana S, et al. Perfil da Borreliose de Lyme no Brasil. Rev Hosp Clin Fac Med S Paulo 1997, 52 (2):111-117.
9. Pirana S, Bento RF, Bogar P, Silveira JAM, Yoshinara NH. Paralisia facial e surdez súbita bilateral na doença de Lyme. Rev Bras Otorrinolaringol 1996, 62:500-2.
10. Belec L, Gherardi R, Georges AJ, Schuller E, Vuillecard E, Di Costanzo B, Martin PM. Peripheral facial paralysis and HIV infection: report of four African cases and review of the literature. J Neurol. 1989, 236: 411-414.
11. Buyukavci M, Tan H, Akdag R. An alarming sign for serious diseases in children: bilateral facial paralysis. Pediatr Neurol 2002, 27:312-3.
12. Adour KK, Bell DN, Hilsinger RL Jr. Herpes simplex virus in idiophatic facial paralysis (Bell palsy). JAMA 1975 233: 527-30.
13. Ghonin MR, Gavillan C, Sarriá MJ. Bilateral simultaneous Bell´s palsy: two cases following herpes simplex gingivostomatitis. ORL J Otorhinolaryngol Relat Spec 1988 50: 26-72.
14. Santos DQ, Adour KK. Bilateral facial paralysis related to sexually transmitted herpes simplex: clinical course and MRI findings. Otolaryngol Head Neck Surg 1993, 108: 298-303.
15. Schwaber MK, Larson TC 3rd, Zealear DL, Creasy J. Gadolinium enhanced magnetic resonance imaging in Bell´s palsy. Laryngoscope 1990, 100: 1264-9.
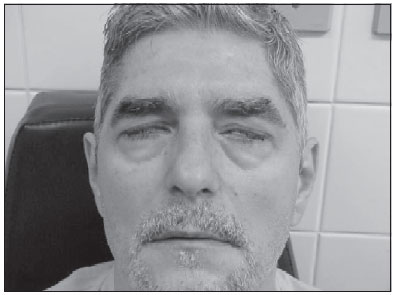
Picture 1. Incomprehensive bilateral ocular closing with maximum effort, absence of bilateral facial mimic musculature movement.
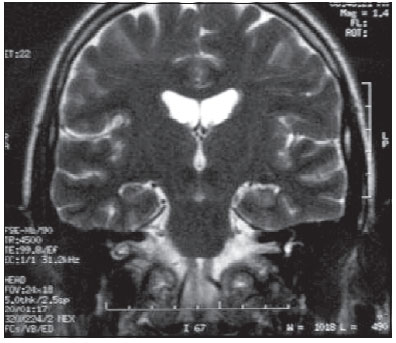
Picture 2. Coronary cut of RM em T2, showing facial nerve course without alterations
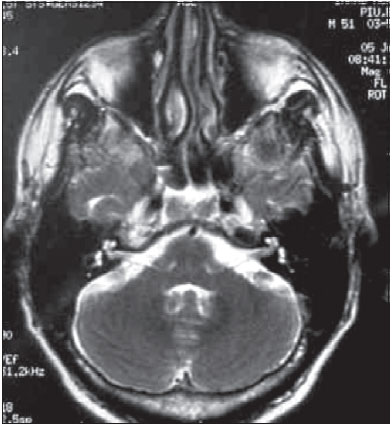
Picture 3. Axial cut of RM em T2, showing facial nerves and inner ear structure preserved.