INTRODUCTIONMalignant fibrous histiocytoma (MFH) is a tumor derived from mesenquimal tissue composed by 5 cell types (7). The term MFH was suggested to describe a tumor histiocytic-like with fibrous tissue (8). Its origin is believed to be from totipotent cells for presenting 2 different cell types (3,7,11). In histological terms, MFH is divided into 5 subtypes (1).
MFH is usually malignant when occurs on profound soft tissue (5). Around 3% of such tumors occur in the area of head and neck (11), and it is rare in larynx (14). New immunohistochemical and by electronic microscopy techniques have increased accuracy of histopathological diagnosis (13).
We described a rare case of MFH in the larynx and discussed its diagnosis and treatment.
CASE REPORT41-year-old-male patient, smoker for 20 years was assisted in June, 2004 at Ambulatório de Laringologia do Hospital de Clínicas da Universidade Federal - Uberlândia (Laryngology Laboratory of Federal University Hospital). He had had hoarseness and globus sensation for six years. He neither has symptoms of dyspnea, dysphagia nor important medical antecedent. He used to smoke 15 cigarettes a day.
Videolaryngoscopy, May, 2004, did not present polypoid lesion on medium third of left vocal fold/cords, with no paresis (Picture 1). There was no palpable cervical lymphadenopathy. In June, 2004, a direct microlaryngoscopy with polyp excision was performed. Anatomy pathological exam showed MFH (Picture 2). In August, 2004, he was submitted frontolateral laryngectomy to left. He was kept in hospital for four days after surgery and did not present intercurrence. The follow-up after 1 year did not show any recurrences.

Picture 1 - Videolaryngoscopy showing polypoid lesion in one third of the left vocal fold, with no paresis.
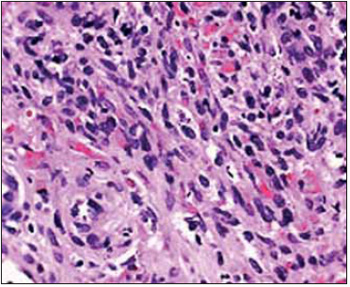
Picture 2 Separation by light microscopy showing large proliferation of fibroblasts mixed in several histiocytic, indistinguished, multinucleated and xantomatous cells (with hematoxylin-eosin. 200X)
The term MFH was suggested by Kauffman and Stout in 1961 in order to describe a histiocytic-like tumor with predominance of fibroblasts (8).
MFH on head and neck area is more common in men, in a proportion of 3:1 (7) and it affects this area only in 3% of the cases (11) on the skin and soft tissues. Nose, paranasal sinus and mandible are the most common areas (3) with malignant feature when in profound areas (5). There are 30 cases reported (14), and most of them are subglottic (1,6,7) , preferably in men on glottic area and in women in subglottic (7). Patient with glottic MFH are usually older and smoker, opposing from subglottic MFH (7).
It is histologically divided into 5 types: pelomorphic, myxoid, inflammatory, giant cells and angiomatous (1). It is derived from mesenquimal tissue composed by 5 cell types: fibroplast, histiocytic, indistinguished, giant multinucleated and xantomatous cells (7). Its origin is believed to be from totipotent cells for presenting two different cell types (3,7,11). Structural analysis through electronic microscopy, immunohistochemical techniques and culture of tissue help in order to differ this type of tumor (1,3,7,11). The immunohistochemical anti-vimentin V9 was positive in this case.
This tumor often presents only clinical symptoms, such as dyspnea, dysphagia, hemoptysis, stridor and tiredness when achieves larger sizes (7). Diagnosis for it is usually established after the removal of the organ (11).
Differential diagnosis should be performed with pleomorphic rhabdomyosarcoma, fibrosarcoma, spinocellular carcinoma, angiosarcoma, hemangiopericytoma, pleomorphic liposarcoma and lymphoma (2).
Surgery is the therapy with block resection of tumor (4,7,9,10,12). The hemilaryngectomy technique was chosen, though tumor was limited to left vocal fold. Cervical emptying was not performed because physical exam did not presented lymphonode involvement. Radiotherapy is reserved to high risky patients, recurrence of non-operated patients and cases of metastasis to distance (2). Some authors suggest chemotherapy for other types of sarcomas (3,11), therefore, few patients with MFH had it (6). Adjuvant radiotherapy and chemotherapy with surgery requires more studying.
MFH of the larynx is a rare type of tumor, but a high recurrence, fast growth, unexpected clinical behavior one and it tends to local and distance metastasis, especially to brain and lungs (1,4,6,7,9). There is a lack of prognosis when there is sign of metastasis and glottic MFH, what differs from subglottic MFH (7).
CONCLUSIONMFH is a rare type of tumor and there are few reported cases in the literature, what make is prognosis and therapy definition difficult. Surgical therapy is the one with ample resection of tumor.
BIBLIOGRAPHY1. Barnes L, Kanbour A. Malignant fibrous histiocytoma of the head and neck. Arch Otolaryngol Head Neck Surg 1988;114:1149-56.
2. Bernaldez R, Nistal M, Kaiser C, Gavilán J. Malignant histiocytoma of the larynx. J Laryngol Otol 1991;105:130-3.
3. Blitzer A, Lawson W, Biller HF. Malignant fibrous histiocytoma of the head and neck. Laryngoscope 1977, 87:1479-99.
4. Canalis R, Green M, Donard H, Hirose F, Cooper S. Malignant fibrous xanthoma of the larynx. Arch Otolaryngol 1975, 101:135-7.
5. Enzinger FM, Weiss SW. Soft Tissue Tumours. St. Louis: C.V. Mosby Company; 1983. pp. 125-35, 170-98.
6. Ferlito A, Nicolai P, Recher G, Name S. Primary laryngeal malignant fibrous histiocytoma: review of the literature. Laryngoscope 1983;93:1351-8.
7. Godoy J, Jacobs JR, Crissman J. Malignant fibrous histiocytoma of the larynx. J Surg Oncol 1986;31:62-5.
8. Kauffman SL, Stout AP. Histiocytic tumors (fibromas, xanthoma and histiocytoma) in children. Cancer 1961;14:469-82.
9. Keenan J, Snyder G, Toomey J. Malignant fibrous histiocytoma of the larynx. Otolaryngol Head Neck Surg 1979;87:599-603.
10. Majumder NK, Sharma HS, Srinivasan V. Malignant fibrous histiocytoma of larynx. J Laryngol Otol 1989;103:219-21.
11. Ogura J, Toomey J, Setzen M, Sobol S. Malignant fibrous histiocytoma of the head and neck. Laryngoscope 1980;90:1429-40.
12. Ramadass T, Balasubramaniam VC, Annamalai L. Malignant pleomorphic fibrous histiocytoma of the larynx. J Laryngol Otol 1984;98:93-6.
13. Saleem M, MacArthur PD, Hainau B, Velagapudi SB. Pathology in Focus: fibrous histiocytoma of the larynx. J Laryngol Otol 1998;112:1205-7.
14. Van Laer C, Hamans E, Neetens I, Van Marck E, Van Oosterom A, Van der Heyning P. Benign fibrous histiocytoma of the larynx: presentation of a case and review of the literature. J Laryngol Otol 1996;110:474-7.
1. Resident doctor at Serviço de Otorrinolaringologia da Faculdade de Medicina da Universidade Federal de Uberlândia.
2. Master in Othorhinolaryngology - Head of Laryngology Division at Serviço de Otorrinolaringologia da Faculdade de Medicina da Universidade Federal de Uberlândia
3. Titled Professor - Head of Serviço de Otorrinolaringologia da Faculdade de Medicina da Universidade Federal de Uberlândia
Serviço de Otorrinolaringologia da Faculdade de Medicina da Universidade Federal de Uberlândia, Uberlândia, Minas Gerais, Brasil - Otorhinolaryngology Service from Medical School of Federal University.
Lucas Gomes Patrocínio
Address: Rua XV de Novembro, 327 / aptº. 1600 - Bairro Centro Uberlândia - MG CEP: 38.400-214 Telefone/Fax: (55) 34 - 3215-1143 E-mail: lucaspatrocinio@triang.com.br
This article was submitted to SGP - Sistema de Gestão de Publicações (Publication Management System) from RAIO on December 7, 2005 and was approved on March 8, 2006 10:27:54.