INTRODUCTIONAllergic Rhinosinusitis (AR) is one of the main chronic respiratory pathologies for its high level of prevalence, its association with asthma and sinusitis and for the impact in people's quality of life(1,2,3,4). It presents locally and is systemic to allergy. Around 15% of world population presents symptoms related to it(1,2,4), especially those with other allergic diseases such as asthma and atopic dermatitis. In the South and Southeast of Brazil, prevalence of symptoms was higher in May and August, while in the Northeast there was no difference regarding year months(3). Nasal symptoms presented by Brazilian students ranged from 19.3 to 47.4% during International Study of Asthma and Allergies in Childhood(3).
80%(4) people with asthma can be affected by AR. There is an association with bacterial rhinosinusitis, allergic conjunctivitis and otitis media (inflammation of the middle ear), and therapy for these depends on AR proper control(1).
AR patients present hypersensitiveness reaction type 1, with persistent inflammation of nasal mucosa. Inflammatory cells such as eosinophils and mastocytes and mediators as chemokines and cytokines make part of physiopathology. Atopic patients develop Th2 with cytokines such as IL-4, IL-5 e IL-10 (6,7,8,9,10) as standard immune response. B-Lymphocytes from patients previously sensitive to some allergens produce IgE antibodies that are linked to mastocyte and basophil surface through receptors of high connection with Fc portion of antibodies. After a new contact, allergen is linked to IgE, which is in the mastocyte surface, causing their degranulation, with the release of histamine lipid-derived substances (prostaglandin and leukotriene) and cytokines. Eosinophils are also united to this inflammatory area releasing cation protein with amplification of allergic response (11).
Nasal hyper-reactivity symptoms are: runny nose, itching and nasal obstruction, which can recede spontaneously or under therapy(7). These symptoms are related with exposure to some allergens, such as: home dust, cockroach antigens, fungus, animal skin and pollen.
Persistent rhinitis is classified when symptoms remain for more than 4 days a week or more than 4 weeks; intermittent rhinitis is when symptoms remain for less than 4 days a week and less than 4 weeks(12).
Rhinitis can be still classified as mild, moderate and severe according to symptoms, depending on how they influence on sleep and daily activities(12). Physical exam findings are not specific and comprehend mucous pallor and hypertrophy of inferior turbinates or those ones related to sinusitis and otitis.
Diagnosis is clinical but can involve test in order to detect IgE either free or cell-related. Specific skin tests to inhaling allergens are important tools to confirm allergic rhinitis and to detect allergens involved in disease pathogenesis, moreover planning specific immunotherapy treatment(12). Specific IgE can also be in vitro detected through RAST testing (radioallergosorbent).
Allergic Rhinitis therapy consists of above environmental control, medication use that prevents mastocytes degranulation and modulates immune response(12). Patients submitted to corticosteroid or immunotherapy treatment change from standard of Th2 immune response to Th1, with an increase on interferon-gama production(9).
OBJECTIVETo evaluate patients who complain of allergic rhinosinusitis according to most frequent symptoms, signs observed from videoendoscopic examination, positive skin hypersensitiveness and association to bronchospasms.
MATERIAL AND METHODSThe total sum was 45 patients for this study. 39 of them aging from 10 to 35 years were selected. They presented spontaneous complaint of allergic rhinosinusitis and inflammation of the nasal mucosa or one of the followings: nasal obstruction, hiposmia, rhinorrhea, sneezing or itching according to II Brazilian Consensus on Rhinitis(3).
A clinical questionnaire on pathology background and main symptoms was applied. Preceding bronchospasms was evaluated through a questionnaire on medical evaluation due to respiratory complaint. It was also performed clinical ENT exams and nasal videoendoscopy in all patients by the same professional (more than 5 years of experience).
Patients were submitted to skin hypersensitiveness tests. The tested antigens were: tobacco, grass, house dust, cat and dog skin, fungus, flowers and woolen fabric by making use of prick test
R. The test consisted of pouring a drop of each allergen on patient's forearm and pricking it. Positive control was performed with histamine and negative one with the diluents of the chosen allergens; in such cases, we choose the FDA allergens. Test interpretation was done 15 minutes later through measures of perpendicular diameter of emerged nodules. Result was considered positive when induration occurred on inoculation point of a tested allergen with a 3mm diameter or larger.
Patients who did not attend service to have their tests done were excluded from the study, besides the mentioned criteria. All patients signed the Free and Clear Consent Term and the study was previously approved by Research Ethics Committee in November, 2004, CAAE - 0022.0.057.000-04.
RESULTThe main symptoms reported by patients, in reply to the questionnaire were: nasal itching (96.5%), nasal obstruction (93%), sneezing (93%), runny nose (82.7%), itching in the pharynx (65.5%), itching eye (62%) and eye tearing (55%) (Chart 1).
Chart 1.
When questioned on bronchospasms background, 14% of patients reported 1 or more occurrences, and 86% did not report any (Chart 2).
Chart 2.
The main findings from external rhinoscopy evaluation and nasal videoendoscopy were: hypertrophy of inferior turbinate (69%) (Picture 1), mucous pallor (65.5%), septum deviation (41.3%) and hypertrophy of middle turbinate.
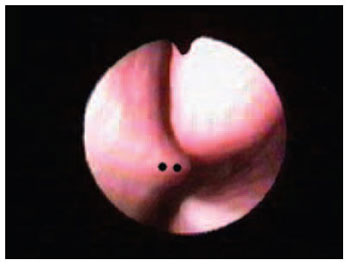
Picture 1. Septal Deviation - black dots - septal spur next to middle turbinate.
Prick test
R was performed at the last stage of the exams. Results were evaluated according to mentioned criteria. From the patients who sought ENT department with compatible complaints of allergic rhinosinusitis, according to II Brazilian Consensus on Rhinitis (Chart 3), 73% of them presented positive response on skin test, while 27% presented negative one.
Chart 3.
The main allergens that affected patients with rhinitis complaints were: house dust (54 %), cat skin (34.6%), dog skin (27%), tobacco (23%), woolen fabric (19.2%), fungus (19.2%), hay (19.2%), flowers (7%) and grass (7%). (Chart 4).
Chart 4.
Patients who complain of allergic rhinosinusitis also present signs and symptoms that vary regarding manifestation frequency, environment and time of year. In temperate climate areas, for instance, patients present more intense symptoms of nasal obstruction and coriza in severe winter and in spring (pollination season). In tropical and equatorial climates, the presence of humidity raises colonization by fungus in the environment and might expose people to more intense allergic symptoms. Symptoms can vary in idiosyncratic manner according to temperature, environment hygiene and to patient's genotype.
This study reports symptoms with more occurrences in patients from tropical areas, what is not so different from symptoms occurring in temperate climate areas. However, symptoms intensity and frequency was not the aim of this study.
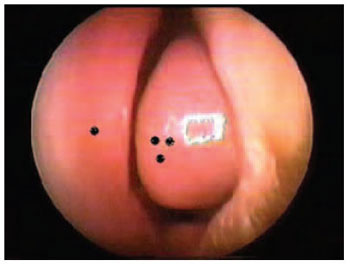
Picture 2. Hypertrophy of inferior turbinate - single black dot - nasal septum Triple black dot: Hypertrophy of inferior turbinate, covering more than 75% of respiratory area.
The correlation between skin sensitiveness and allergic rhinitis complaint was 73% of patients. This agrees with the literature that shows a 60- 70% correlation. The frequency of allergens was also similar, and house dust prevailed.
It is important to point the positive factor of tobacco on allergic tests (23%), as it does not lead to an IgE-mediated response, suggesting primary skin irritation and non- positive factor of skin test. At last, it was noticed a low frequency complaint of bronchospam symptom from patients with allegic rhinitis (14%). This information is important because the results from other studies were the opposite, between 80 and 100%(4-13). This information could be analyzed as bronchospasms represented a more advanced and systemic disease in relation to rhinitis, then patients who would develop bronchospams, would have previously presented mild symptoms such as rhinitis and dermatitis. Symptoms can vary in idiosyncratic manner according to temperature, environment hygiene and to patient's genotype(12- 15).
CONCLUSIONENT manifestations of allergic rhinitis differed from the literature and the consensus. Exam results depend on techniques, correct interpretation and quality of equipment. In the skin test findings, we had result alterations regarding antigen choice and manufacturer of the studied allergens.
REFERENCES1. Bousquet J, Van Cauwenberge P, Khaltaev N, ARIA Workshop Group World Health Organization. Allergic rhinitis and its impact on asthma initiative. A pocket guide for physicians and nurses. Merck & Co., Inc., 2001.
2. American Academy of Allergy, Asthma & Immunology. The allergy report. Milwaukee, WI: The American Academy of Allergy, Asthma & Immunology, Inc., 2000.
3. Solé D, Weckx LLM, Filho NAR, Júnior JFM, et al. II Consenso Brasileiro sobre Rinites 2006. Rev. bras. alerg. Imunopatol 2006; 29(1):29-58.
4. Wang DY, Clement P. Pathogenetic mechanisms underlying the clinical symptoms of allergic rhinitis. Am J Rhinol 2000; 14:325-33.
5. Leynaert B, Neukirch F, Demoly P, Bousquet J. Epidemiologic evidence for asthma and rhinitis comorbidity. J Allergy Clin Immunol 2000; 106:S201-5.
6. Benson M, Strannegard IL, Wennergren G, Strannegard O. Interleukin-5 and interleukin-8 in relation to eosinophils and neutrophils in nasal fluids from school children with seasonal allergic rhinitis. Pediatr Allergy Immunol 1999; 10:178-85.
7. Mygind N, ed. Allergic and nonallergic rhinitis clinical aspects. Philadelphia: Saunders, PA, 1993.
8. Naclerio RM, Proud D, Togias AG, et al. Inflammatory mediators in late antigen- induced rhinitis. N Engl J Med 1985; 313:65-70.
9. Bascom R, PipkornU, Lichtenstein LM, Naclerio RM. The infux of inflammatory cells into nasal washings during late response to antigen challenge: effect of corticosteroid pretreatment. Am Rev Respir Dis 1988; 138: 406-412.
10. Bradding P , Feather IH, Wilson S, et al. Immunolocalization of cytokines in the nasal mucosa of normal and perennial rhinitis subjects. J Immunol 1993; 151:3853-3865.
11. Durham SR, Sun Ying M, Varney VA,et al. Cytokine messenger RNA expression for IL-3, IL-4, IL-5 nad granulocyte/macrophage- cloning- stimulating factor in the nasal mucosal after local allergen provocation : relationship to tissue eosinophilia. J Immunol 1992; 148:2390-2394.
12. Bousquet J, Van Cauwenberge P, Khaltaev N, ARIA Workshop Group, World Health Organization (WHO). Allergic Rhinitis and its Impact on Asthma. J Allergy Clin Immunol 2001; 108 (Suppl):S147-S334.
13. Bousquet J, Vignola AM, Demoly P. Links between rhinitis and asthma; Allergy. 2003 Aug;58(8):691-706
14. Rosenwasser L. New insights into the pathophysiology of allergic rhinitis Allergy Asthma Proc. 2007 Jan-Feb;28(1):10-5
15. Ramsey CD, Gold DR, Litonjua AA, et al. Respiratory illnesses in early life and asthma and atopy in childhood. J Allergy Clin Immunol. 2007 Jan;119(1):150-6.
16. Yuen AP, Cheung S,Tang KC. et al. The skin prick test results of 977 patients suffering from chronic rhinitis in Hong Kong. Hong Kong Med J. 2007 Apr;13(2):131-6.
1. Expert in ENT and Legal Medicine (Assistant Teacher of Cervical-Facial Surgery at Santa Casa da Bahia, Hospital Santa Izabel; and teacher of Cervical-Facial Anatomy at UNIME- BA)
2. PhD in ENT by USP - Head of the ENT Discipline and Cervical-Facial Surgery at Santa Casa da Bahia, Hospital Santa Izabel)
3. Master degree in Pathology by Fio Cruz/UFBA - Assistant Professor of ENT and Cervical-Facial Surgery at Santa Casa da Bahia, Hospital Santa Izabel)
4. Expert in ENT by Santa Casa de Saúde da Bahia - expert in Immunology by USP - Allergy and Immunology doctor at Alergon Clinic).
Santa Casa de Misericórdia da Bahia
Adriano Santana Fonseca
Mail address: Rua das Patativas, 43, apto 1004. Imbui - Salvador/BA - CEP: 41720-100.
This article was submitted to SGP (Sistema de Gestão de Publicações - Publication Management system) of R@IO on September 26th, 2007 and approved on October 27th, 2007 at 12:56:55.