INTRODUCTIONSeveral diseases can affect the external ear canal (EAC), causing conductive hearing loss. They are usually associated with ear pain, otorrhea and tinnitus, and the main cause is the presence of cerumen, eczema, external otitis and otomycosis. The benign tumors on this area are a rare process, but its etiological diagnosis is important(1) as the otoscopic findings do not present differences between benign and malignant lesions.
Exostosis is the most found benign tumor of the EAC (6.3 in 1000 patients with ENT complaints)(2). Vascular lesions are less common and hemangioma is the main one. The differential diagnosis is important in order to determine the correct analysis and proper therapy(3).
Hemangioma is a vascular lesion usually found in the dermis. It is more common in young children and it progressively disappears before the ages of 5-6 years. They occur in two developmental stages (1): a quick growth stage (proliferative stage), followed by a decline one. In histological terms, an endothelial hyperplasia and an increase of mastocytes is noticed in the proliferative stage. Fibrosis, fatty infiltration, cell reduction and number normalization of mastocytes are noticed in the decline stage (2). Hemangioma can be either capillary type when vessels are organized in capillary structures or cavernous type when presenting large vascular spaces, which is more common in the skin and in the mucosa. In children, during the proliferative phase, it has been observed that the urine and serum levels of the basic fibroblasts growth factor (bFGF) have increased(1).
CASE REPORTA 41-year-old-male Causasian patient searched for ENT assistance complaining of progressive hearing loss to the left for the past 2 months. He did not report ear pain, otorrhea or even previous history of otological disorder. He had previously gone to another service complaining of hearing muffling to the left, being diagnosed with Eustachian tube dysfunction disorder and treated with loratadine and pseudoefedrine, but no success. Through otoscopy, pedicled mass could be seen starting from anteroposterior wall of the internal third of the left EAC (Picture 1). The lesion virtually occupied all EAC diameters, but it was possible to compress the mass and to observe the tympanic membrane (TM). When compressing the mass, transitory auditory improved, but with the increase of the lesion, hearing ability got worse. CT scan (TC) of temporal bone was carried through, what confirmed the localization of the lesion, the absence of TM involvement and the absence of spreading to other areas, and also mild impregnation by the contrast in the lesion surroundings (Picture 2 and 3).
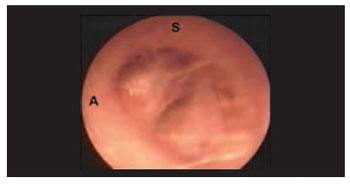
Picture 1. Pedicled mass of the left external auditory canal (A: anterior; S: superior)
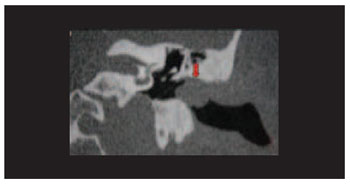
Picture 2. CT scan finds lesion (arrow), showing no involvement of the tympanic membrane and no extension to adjacent structures.

Picture 3. CT scan showing mild impregnation by contrast in the lesion surroundings (arrow).
Patient was submitted to transcanal surgery, by displacing EAC skin up to the lesion, when there was an intense bleeding, which was partially managed with cotton pieces soaked in vasoconstrictor and cauterization of pedicle of the lesion that transversed tympanic bone, but without eroding it. Dissection of the skin was carried out, but there was no success and then after that a medial incision to the mass in order to avoid displacement and unexpected lesions in the midline skin of the EAC and of the tympanic angle. At this stage, the lesion was removed with posterior drilling, by using drill diamond burs of the anterior wall of the EAC, in order to perform a better hemostasis. The area was fulfilled with skin graft from the midline surface of the left arm. The anatomopathological diagnosed microvascular hemangioma (Picture 4). Patient condition improved and he presented with no symptoms in the last examination (6 months after surgery). He had complete cicatrisation of the EAC and no recurrence of the lesion.
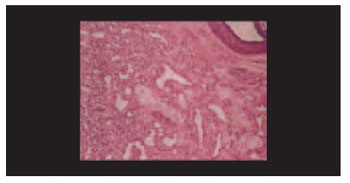
Picture 4 - Histopathological exam showing microvascular hamangioma.
Freedman (in 1972) was the first to report the presence of hemangioma in the outer ear, describing two male patients at their 60´s with lesion that started from the posterior wall of the EAC affecting TM(4). Since then, few cases have been reported. In 1987, Hawnk and van Nostrand described the first case of hemandioma of EAC with no involvement TM, and up to now there have been only 3 cases like that(1). In the current case, lesion started from the anterior wall of the ECA and when compressed, it does not seem to affect TM.
Differential diagnosis of the vascular lesions in the ear counts for: glomus jugulare and glomus tympanic tumors, high jugular bulb, aberrant internal carotid artery, arterial-venous malformations and others(1). Otoscopy revealed a non pulsatile lesion and no color alteration. Even so, temporal bone CT with contrast is important to achieve differential diagnosis, limiting the lesion extension and evaluating its vascularization(6). CT did not show TM involvement or extension to adjacent structures, besides it showed mild impreganation by contrast in the lesion surroundings.
Hemangioma treatment consists of surgery and its removal. When removing the lesion, the current authors built a skin graft in the site due to the extension of the bloody area. Definite diagnosis is done through the anatomopathological exam(8), and prognosis is favorable most of time and its recurrence is rare(7). Patient presented with good recovery and no recurrence of the lesion.
CONCLUSIONThe presence of tumor mass in the EAC can offer several diagnosis hypotheses, such as hemangioma, especially id the lesion is soft and compressible, regardless skin color, as the reported case. It is important to limit the lesion regarding localization, tympanic membrane involvement and invasion of adjacent structures, and CT scan is the best exam for that. Surgery is the best therapy for hemangiomas by providing good prognosis and few chances of complications.
REFERENCES1. Reeck JB, Yen TL, Szmit A, Cheung SW. Cavernous hemangioma of the external ear canal. Laryngoscope. 2002 Oct;112(10):1750-2.
2. Newcomer NT, Marple B. Benign Tumors of the External Ear. Emedicine, 2002: http://www.emedicine.com/ent/topic706.htm.
3. Limb CJ, Mabrie DC, Carey JP, Minor LB. Hemangioma of the external auditory canal. Otolaryngol Head Neck Surg. 2002 Jan;126(1):74-5.
4. Freedman SI, Barton S, Goodhill V. Cavernous angiomas of the tympanic membrane. Arch Otolaryngol. 1972 Aug;96(2):158-60.
5. Hawke M, van Nostrand P. Cavernous hemangioma of the external ear canal. J Otolaryngol. 1987 Feb;16(1):40-2.
6. Chakeres DW, Kapila A, LaMasters D. Soft-tissue abnormalities of the external auditory canal: subject review of CT findings. Radiology. 1985 Jul;156(1):105-9.
7. Jackson CG, Levine SC, McKennan KX. Recurrent hemangioma of the external auditory canal. Am J Otol. 1990 Mar;11(2):117-8. 8. Kemink JL, Graham MD, McClatchey KD. Hemangioma of the external auditory canal. Am J Otol. 1983 Oct;5(2):125-6.
1. PhD degree in Medical Science by Universidade Federal do Rio Grande do Sul. Adjunt Professor of the ENT and Ophthalmology department of the Fundação Federal Faculdade de Ciências Médicas de Porto Alegre. Professor of the Post Graduation program in Medical Science at Universidade Federal do Rio Grande do Sul.
2. PhD Student of the Post Graduation program in Medical Science at Universidade Federal do Rio Grande do Sul. ENT doctor at Complexo Hospitalar Santa Casa de Porto Alegre.
3. Medical Student at Fundação Federal Faculdade de Ciências Médicas de Porto Alegre.
4. Medical Student at Fundação Federal Faculdade de Ciências Médicas de Porto Alegre.
5. Medical Student at Fundação Federal Faculdade de Ciências Médicas de Porto Alegre.
Fundação Federal Faculdade de Ciências Médicas de Porto Alegre (Federal Institution - Medical Science College). Post Graduation Program in Medical Science - Universidade Federal do Rio Grande do Sul (Federal University - Rio Grande do Sul - Brazil).
José Faibes Lubianca Neto. (Clínica Otorrinos Porto Alegre - ENT Clinic)
Mail Address: Rua Dona Laura, 320, 9o andar. Porto Alegre/RS. CEP 90430-090. Phone/FAX: (51) 3029-8749
This article was submitted to SGP (Sistema de Gestão de Publicações - Publication Management system) of R@IO on January 10th, 2007 and approved on June 29th, 2007 at 18:29:35.