INTRODUCTIONBranchiogenic cyst represents a trace of the branchial system (responsible for the development of the osteocartilaginous, muscular, neural and vascular structures of the neck). It occurs when the cervical sinus of His, a space formed due to the first branchial slits growth, does not obliterate completely. The most common branchiogenic cyst is that originated from the 2nd branchial slit and is located at the high cervical region, in front of the sternocleidomastoideus muscle, jugular-carotid region. It appears as a cervical mass, of plain and fibroelastic consistence, with side mobility, generally after upper respiratory passages infection episode (1,2).
There is a great controversy in the literature regarding the existence of the cancerized branchiogenic cyst. Most authors believe this entity does not exist, and that it is, actually an unknown primary tumor metastasis (3,4,7,8).
CASE REPORTThe patient M.I.M.L.P., 50 years old, leucodermic, married, from Belo Horizonte, sought for the otorhinolaryngology service in January 2005 complaining of cervical node to the right, of slow and progressive growth, slightly painful. This clinical picture had started about 45 days from then, when she presented tonsillitis. The patient denied other symptoms, such as dysphagia, dysphonia or emaciation. Otorhinolaryngologic exam without changes. At cervical palpation, we identified a cervical node at jugular chain to the right, with approximately 2 to 3 cm of diameter, movable and of fibroelastic consistence. We prescribed cervical ultrasonography, needle biopsy and fibronasolaryngoscopy. She returned with exams in April 2005: the US showed hypoechoic image, slightly heterogeneous, with well defined contours, measuring 40.7 x 28 x 16mm, along with the right parotid inferoposterior part. PAAF: superficial and intermediate epithelial cells with horny scales, penetrated by typical fusiform cells and rare lymphocytes, suggesting a dermic epithelial cyst. The nasal fibroscopy did not evidence any lesion. Before the case exposed, we suspected of branchiogenic cyst and indicated a surgery, which was carried out only in August of this year. In the per-operative, we identified a lesion of cystic aspect in the upper right jugular chain, which broke down and drained a yellow and thick secretion. A material was sent for anatomopathologic exam and suggested it was a squamous cell carcinoma slightly different from the metastatic carcinoma. A new physical exam was then carried out without changes. We requested cervical and abdomen ultrasonography, high digestive endoscopy, chest X-ray, and then chest computed tomography and Pet Scan without changes. The patient was forwarded to the oncologist, who indicated radiotherapy. Now, she's in the second follow-up year without signs of disease and also without the location of the probable primary tumor.
Figure 1. Cancerized Branchiogenic Cyst - Cervical ultrasonography showing cyst in right parotid inferoposterior portion.
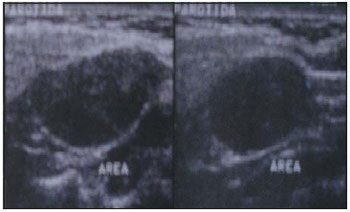
Figure 2. Cancerized Branchiogenic Cyst - Cuts of the part colored by HE.
The branchial system is composed by five arches of mesodermic origin, separated externally by furrows of ectodermal origin and internally by endodermic purses that will form the osteocartilaginous, muscular, neural and vascular structures of the neck (1,2).
There are four types of branchiogenic cysts, according to the origin arch: the most common is that of the 2nd branchial slit, followed by the 1st and then the 3rd and 4th. They appear generally as a plain movable lesion, of fibroelastic consistence, in the upper jugular-carotid region after infection in the upper respiratory passage (1,2).
For many years we have been trying to prove the existence of cancerized branchiogenic cyst (3). However, most authors believe that it does not exist or, in the other hand, that it is extremely rare, about 0.3% of all the supraclavicular cancers. They state that, actually, they are unknown primary tumor metastasis cystic degenerations (3,4,5,6,7,8).
The reason for such a controversy occurs due to several factors: histological difficulty to tell a branchiogenic cyst cancerization from a metastatic lymphonode; the lymphonode metastases generally occur at the same location of the branchiogenic cysts; the metastases are much more frequent than branchiogenic cysts and because the cervical metastases may be the first manifestation of a tumor of the upper aerodigestive tract (3,5,6,7). In addition to this, the metastasis, in most cases, may not be discarded as there is no proper period for patient follow-up (3).
Martin et al have proposed four criteria to characterize a cervical mass as a cancerized branchiogenic cyst, however these also apply to cystic metastases. The criteria are: 1) It must be located right in front of the anterior border of the sternocleidomastoideus muscle; 2) Histological appearance that the growth occurs in tissue with branchial traces; 3) The patient must be alive and have a follow-up, with periodic exams for at least 5 years without developing a primary tumor and 4) Present histological evidences that the tumor has developed in the epithelial wall of a lateral cyst of the neck (3,4).
The possibility for occurrence of cervical cystic metastasis is largely known. Its incidence reaches from 33 to 50% when it comes to Waldeyer's ring tumors (3,4). For this reason, some authors suggest amygdalectomy to help in the differential diagnosis (3,9).
The treatment for cancerized branchiogenic cyst must be aggressive and similar to that of the unknown primary tumor. We should proceed with the lesion exeresis, in case it is identified, and cervical excavation in multiple nodes or nodes bigger than 3cm (6). The use of postoperative radiotherapy is also recommended (3,5,7).
CONCLUSIONMost cases of cancerized branchiogenic cyst cases described were actually primary tumors metastases. However, in case the primary is not found, we shall never know if it is really a branchigenic cyst that was cancerized or a cervical metastasis correctly treated and eradicated, since the diagnosis superpose.
BIBLIOGRAPHICAL REFERENCES1. Cummings CW. Otolaryngology - Head and Neck Surgery 2a ed. Missouri: Copyright; 1993, Vol 2, pp. 1554-1559.
2. Campos CAH, Costa HOO, editores. Tratado de Otorrinolaringologia 1a ed. São Paulo: Roca; 2002, Vol 4, pp. 227-234.
3. Briggs RD, Pou AM, Schnadig VJ. Cystic Metastasis Versus Branchial Cleft Carcinoma: A Diagnostic Challenge. Laringoscope. 2002, 112(8):1010-1014.
4. Micheau C, Klijanienko J, Luboinski B, Richard J. So-Called Branchiogenic Carcinoma is Actually Cystic Metastases in the Neck from a Tonsillar Primary. Laringoscope. 1990, 100(8):878-883.
5. El-Sharkawi A, Williams GT. Malignant Branchioma - A Further Insight. Eur J Surg Oncol. 1993, 19(6):567-8.
6. Thompson LDR, Heffner DK. The Clinical Importance of Cystic Squamous Cell Carcinomas in the Neck. Cancer. 1998, 82(5):944-56.
7. Jereczek-Fossa BA,Casadio C, Jassem J, Luzzatto F, Viale G, Bruschini R, Chiesa F, Orecchia R. Branchiogenic Carcinoma - Conceptual or True Clinico-Pathological Entity? Cancer Treat Rev. 2005, 31(2):106-14
8. Devaney KO, Rinaldo A, Ferlito A, Silver CE, Fagan JJ, Bradley PJ, Suárez C. Squamous Carcinoma Arising in a Branchial Cleft Cyst: Have You Ever Treated One? Will You? J Laryngol Otol. 2008, 122(6):547-50.
9. Delank KW, Feytag G, Stoll W. Clinical relevance of Lateral Branchial Cyst. Laryngorhinootologie. 1992, 71(12):611-7.
1. Resident Doctor. 3rd year of specialization in ORL.
2. Specialist Medical Doctor in Otorhinolaryngology.
3. Resident Doctor. 2nd year of specialization in ORL.
4. Specialist in Cervical-Facial Surgery and Otorhinolaryngology. Preceptor of the Specialization in Otorhinolaryngology of Hospital Socor de Belo Horizonte.
5. Master's Degree in Pathology by UFMG. Assistant Professor of the Department of Pathologic Anatomy of UFMG Pathologist of the Institute Roberto Alvarenga.
Institution: Hospital Socor. Belo Horizonte / MG - Brazil.
Mail address:
Carolina Pimenta Carvalho
Rua Augusto Moreira, 237 - Apto. 202 - Santa Amélia
Belo Horizonte / MG - Brazil - Zipcode: 31555-100
Fax: (+55 31) 3330-3294
E-mail: cpcarvalho8@yahoo.com.br
Article received on September 18, 2007.
Article approved July 3, 2008.