INTRODUCTION The adenotonsillar hyperplasia is the most common cause of respiratory obstruction in children and unchains obstructive sleep disorders that include a variable group of abnormalities such as snoring and sleep obstructive apnea syndrome. Moreover, these children may present with a high incidence of recurrent infections of the upper airways with the frequent use of antibiotics (1). Such patients present variegated clinical symptoms and there may occur alterations of the normal breathing standard, dental arch, increase of the curvature of the palate, diction, chewing and deglutition (1,2). It is also possible to find behavior alterations, such as, low school development, irritability, somnolence and morning headache or headache relating to growth, such as low weight gain and low body length (2,3). In the more severe cases the children may have cardiovascular manifestations such as systemic hypertension, cor pulmonale and left ventricle hypertrophy. In many situations the adenotonsillectomy is the choice treatment (4).
The tonsils and adenoids are located at the entry of the respiratory and gastrointestinal tract and are the largest components of the Waldeyer's lymphatic ring, fundamental structures for induction of immune response and formation of antibodies. It may be the region of a series of pathological processes, specially infectious ones and results in a number of important signs and symptoms, mainly in children with a decreased immune response, that generate recurrent pictures of tonsillitis (1,4,5). This is one of the main reasons for prescription and indiscriminate use of antibiotic with a consequent increase of the bacterial resistance and selection (6). Although the allergic rhinitis is not the essential factor in the genesis of the adenoid hyperplasia, there are traces of its major incidence in children with rhinitis and it is one more factor that contributes for the installation of a chronic inflammatory reaction of the nasal mucosa, which stimulates the lymphatic tissue (7).
The administration of antibiotics and the intranasal topical use of corticosteroids for temporary relief of the obstructive and/or allergic symptoms are applied mainly in cases where one desires to postpone the surgery or in case the surgical risk is very high (8). Then the adenotonsillectomy indications and contraindications must be strict and we must take into account the physical, psychic and socioeconomical damages of the patients who many times spend time and money to obtain medical assistance (1,4,9).
Several studies have been showing the role of the adenotonsillectomy in different aspects, such as improvement of behavior, cognition and life quality of children with adenotonsillar hyperplasia (2,3,10,11). However, most of them evaluate the improvement immediately or some months after the surgery. A few studies analyze such results at a long term, with periods of about one year. In our area, JUNIOR et al (2008) (12) reported that the positive impact on the life quality remained for about 15 months after surgery. Through a questionnaire developed by DE SERRES et al (2.3) DI FRANCESCO et al (2004) (13) reported an increase of the life quality of the children submitted to adenotonsillectomy and evaluated domains such as physical suffering and sleep disorders. Despite some authors confirm that in some children the allergy may be a risk factor for adenoid hyperplasia (7) and that the children with adenotonsillar hyperplasia have an increased risk of UAI and continuous use of antibiotic therapy (1,6), the works in the literature approaching these aspects are uncommon.
This work analyzed the effect of adenotonsillectomy on the life quality of children with adenotonsillar hyperplasia in a broader manner, by comprising aspects such as prevalence of nasal obstruction, rhinitis, UAI and the use of antibiotics before and after a long term after surgery.
METHOD Through a prospective clinical study we interviewed 51 parents of patients coming from the unified health system (SUS) who had been submitted to adenotonsillectomy at the Hospital Universitário "Leonar-do Domingos Cerávolo", Presidente Prudente, SP, aged between 3 to 14 years. The surgeries were performed between August 2006 and August 2007 and the interviews were carried out at least 12 months after and at most 18 months after the surgery. The inclusion criteria were hyperplasia of the palatine tonsils level III or more and the increase of the pharyngeal tonsil of at least 50% (in the Cavum X-Ray), and/or presence of recurrent tonsillitis. We excluded maxillofacial malformations, neurologic diseases or concomitant otological and/or nasal surgeries. The project was approved by the Ethics Committee in Research of UNOESTE and HU.
For evaluation of the patients we used a questionnaire proposed by DE SERRES et al. (2000; 2002) (2.3) (Picture 1) and previously used in Brazil by DI FRANCISCO et al. (2004) (13). Other domains were researched by using a questionnaire with a scale from 1 to 4 or more than 4, as the number of tonsillitis before the surgery; use of antibiotics before and after the surgery; number of UAI after the surgery and the appearing of episodes of pharyngitis 7 duly diagnosed after the surgery.
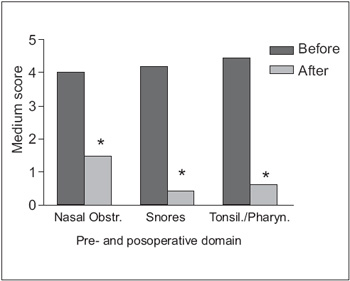
Picture 2. Average values±DP of the domains of nasal obstruction, presence of snores and episodes of tonsillitis and pharyngitis of children with adenotonsillar hyperplasia before and after the adenotonsillectomy. *p< 0.05 comparing the nasal obstruction; *p< 0.001 comparing the presence of snore and *p< 0.001 comparing the presence of tonsillitis and pharyngitis.
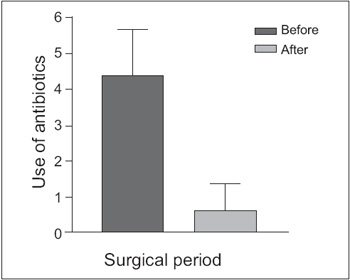
Picture 3. Average values±DP of the reduction in the frequency of use of antibiotics reported by 51 children with adenotonsillar hyperplasia before and 12 to 18 months after the adenotonsillectomy; *p< 0.01.
In a scale ranging from 1 to 10 we asked whether the parents were worried about the child's snoring even after surgery and the level of satisfaction of the parents regarding the surgery. In order to evaluate the role of rhinitis in the life quality of the children submitted to adenotonsillectomy, we asked about the medical diagnosis and the presence of the main symptoms of rhinitis.
The statistical analysis was carried out by using a test t of Student, through the statistical software R v. 2.5.1 (R Development Core Team 2009, Vienna, Austria. ISBN 3-900051-07-0) and GraphPad software (V4.0) (San Diego, CA). The correlation coefficients were computed by using the statistical software MINITAB v.13. The level of statistical significance was defined as 5%.
RESULTS 51 children were analyzed comprising 31 of the male sex (60.78%) and 20 of the female sex (39.22%) (*p<0.05), aged between 3 to 14 year at the time of surgery and the higher prevalence was between children aged 36 years old (29 of 51; 56.86%). The number of children who lived in Presidente Prudente (28 of 51; 54.90%) was similar to those who lived in other cities of the region (23 of 51; 45.10%) (p>0.05).
We verified a decrease in the degree of nasal obstruction and 39 children (76.47%) had a high degree of nasal obstruction before (4.00±1.48) and 9 (17.65%) reported seldom event after the surgery (0.74±0.85; *p< 0.05). In the domain about sleep disorder, there was a strong diminishment of snore of the children after surgery (4.16±1.47 vs 0.43±0.96; *p< 0.001). Upon evaluation of the surgery effect on the number of tonsillitis, we verified that 39 (76.47%) of the children had 5 or more episodes per year before the surgery (4.43±1.14) and only 1 (1.96%) had the same episode for a period of up to 1 year after the surgery (0.61±0.94; *p< 0.001) (Picture 2).
There was a significant diminishment of the use of antibiotics when we compared the periods before (4,331,26) and after surgery (0.59±0.90; *p< 0.001) (Picture 3) with decrease in the number of upper airways infections (UAI) and 30 (58.82%) children had only two episodes in up to 18 months after the surgery. There was no significant alterations in the domains about problems of speech and deglutition, emotional discomfort and activity limitations and these complaints had a lower prevalence out of the parameters evaluated.
When we asked about the level of satisfaction of the parents regarding the surgery, we verified a high level of satisfaction, once in a scale from 1 to 10, 8 (15.7%) parents ascribed mark 8, 4 (7,8%); mark 9 and 37 (72.5%) reported the maximum mark of satisfaction (Picture 4). And it was more predominant in the female sex (9.85±0.49 vs 9.13±1.48; p=0.020) than in the male sex (Table1).
Rhinitis is generally frequent in patients with upper airways pathologies and it is present in 17 (33.33%) of the individuals in our study. These children had a lower level of satisfaction with the surgery (8.82±1.81) when compared to the children without rhinitis (9.71±0.68; *p= 0.007) (Table 1). All interviewees who did not present a maximum level of satisfaction (27.5%) had rhinitis.
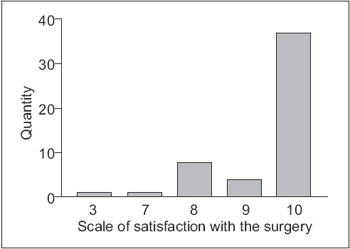
Picture 4. General level of satisfaction as for the surgery ascribed by the parents of children with adenotonsillar hyperplasia and submitted to adenotonsillectomy.
In the last decades, the number of adenotonsillectomy has been decreasing, but it is still one of the most frequent pediatric surgeries. The severe respiratory obstructive processes and the high prevalence of recurrent infections, with the continuous use of antibiotics and selection of a significant number of resistant bacteria may represent criteria for the performance of the surgery (1,4). In our area, we must take into account not only the physical suffering, but also politic and economic matters, such as the large search for medical consultations, long periods of delay for assistance and use of antibiotics which very often have high prices for most part of the population. In our study, an important factor to be emphasized is the fact that all patients assisted were users of SUS, predominantly with low household income. Among the children analyzed, there was a number significantly higher of boys submitted to the surgery than girls, similar to that found by MITCHELL et al (2004) (14), and the number of children living in other cities was similar to those living in Presidente Prudente. Although the adenotonsillectomy is a surgical action of low complexity, this fact reveals the difficult access found by the parents to the specialized assistance in their original cities.
The age range with a higher prevalence was between 3 and 6 years, a period in which the mucosa-associated lymphoid tissue (MALT) is under formation and presents a higher susceptibility to infectious and allergic processes. As from 8-9 years old, this tissue already presents a major stage of maturation and makes the children less prone, a fact also demonstrated by MODRZYNSKI & ZAWISZA (2007) (7) in allergic children with adenoid hyperplasia.
When we evaluated the physical suffering of the children before the surgery, the nasal obstruction had a higher average score with a large reduction after surgery. In the sleep disorders, the presence of snore presented a higher average score with a large reduction after surgery. According to MITCHELL & KELLY (2007) (14) the adenotonsillectomy improved from 79 to 92% the life quality of children who had sleep obstructive disorder. BENNINGER & WALNER (2007) (15), state that when such disorders are not corrected, they may lead to problems such as lack of attention, learning deficit, behavioral problems, or may cause more severe morbidity such as growth diminishment and pumonary hypertension.
The surgeries reduced the number of postoperative infectious episodes from 76.47% to 1.96%. CONLON et al (1999) (16) confirmed that the reduction of tonsillitis after surgery was the main reason of satisfaction of the parents (100%). FUJIMORI et al (2002) (17) suggested that the surgical treatment is an effective approach to improve the oral bacterial flora in children with tonsillitis. As mentioned above, under the conditions of the developing countries, the difficult access to specialized professionals and the high cost of antibiotics, not often available in the public network, are important factors to be taken into account upon indication of the surgery in children who have recurrence of UAI.
The domain with the lowest preoperative and postoperative basal score found was emotional discomfort and activities limitations, which differ from works presented specially in developing countries (9,11,18). In results similar to ours, DA SILVA et al. (2006) (19) attempted to justify such findings in the cultural and climatic matters, since the Brazilians are considered to be more prospective and with hotter climates, in which there is a low prevalence of this kind of complaint.
When the interviewees were asked an evaluation as for the satisfaction concerning the surgery for the preoperative and postoperative life quality, we obtained a high total level of satisfaction, which suggested the importance of the surgery in children with socioeconomic profile similar to that we have researched. The improvement in the life quality of a population with social characteristics similar to ours presenting sleep obstructive disorders was confirmed after adenotonsillectomy in Fortaleza, Ceará (19).
It is important to emphasize that the group that did not ascribe the maximum satisfaction had rhinitis associated, a result also demonstrated by DI FRANCESCO et al (2004) (13). We must consider the low education and socioeconomic level of the parents and their difficult access to the specialized services of SUS as for the good adhesion to the postoperative treatment and the subjectivity of the questionnaire concerning allergic symptoms. By means of the data presented, we may conclude that the adenotonsillectomy improved the children's life quality, mainly for the improvement of the sleep disorders, the significant reduction in the number of UAI's episodes and the decrease in the use of antibiotics. However, the improvement was less significant in children with symptoms of rhinitis.
BIBLIOGRAPHIC REFERENCES 1. Garetz SL. Behavior, cognition, and quality of life after adenotonsillectomy for pediatric sleep-disordered breathing: summary of the literature. Otolaryngol Head Neck Surg. 2008, 138:19-26.
2. De Serres LM, Derkay C, Astley S, Deyo RA, Rosenfeld RM, Gates GA. Measuring quality of life in children with obstructive sleep disorders. Arch Otolaryngol Head Neck Surg, 2000, 126:423-429.
3. De Serres LM, Derkay C, Sie K, Biavati M, Jones J, Tunkel D, Manning S, Inglis AF, Haddad Jr J, Tampakopoulou D, Weinberg AD. Impact of adenotonsillectomy on quality of life in children with obstructive sleep disorders. Arch Otolaryngol Head Neck Surg. 2002, 128:489-496.
4. Burton MJ, Glasziou PP. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/ recurrent acute tonsillitis. Cochrane Database Syst Rev. 2000, (2):CD001802.
5. Avelino MAG, Pereira FC, Carlini D, Moreira GA, Fujita R, Weckx LLM. Avaliação polissonográfica da síndrome da apneia obstrutiva do sono em crianças, antes e após amigdalectomia. Rev Bras Otorrinolaringol. 2002, 68:308-311.
6. Le TM, Rovers MM, van Staaij BK, van den Akker EH, Hoes AW, Schilder AG. Alterations of the oropharyngeal microbial flora after adenotonsillectomy in children: a randomized controlled trial. Arch Otolaryngol Head Neck Surg. 2007, 133:969-972.
7. Modrzynski M, Zawisza E. An Analysis of the incidence of adenoid hypertrophy in allergic children. Int. J. Pediatr Otorhinolaringol. 2007, 71:713-719. 8. Brodsky L, Poje C. Tonsillitis, Tonsillectomy, and adenoidectomy. In: Bailey BJ, et al. Head and neck surgery - otolaryngology. 3th ed. Philadelphia: Lippincott Williams and Williams; 2001. p. 980-91.
9. Constantin E, Kermack A, Nixon GM, Tidmarsh L, Ducharme FM, Brouillette RT. Adenotonsillectomy improves sleep, breathing, and quality of life but not behavior. J Pediatr. 2007, 150:540-546.
10. Do Nascimento GMS, Salgado DC, Maia MS, Lambert EE, Pio MRB, Tiago RSL. Impacto do Tratamento cirúrgico na qualidade de vida de crianças com hiperplasia de tonsilas. Acta ORL. 2007, 25:119-123.
11. Van den Akker EH, Rovers MM, Hordijk GJ, Hoes AW, Schilder AG. Effectiveness of adenotonsillectomy in children with mild symptoms of throat infections or adenotonsillar hypertrophy: open, randomised controlled trial. Clin. Otolaryngol. 2005, 30:60-63.
12. Lima Júnior JM, Silva VC, Freitas MR. Long term results in the life quality of children with obstructive sleep disorders submitted to adenoidectomy/adenotonsillectomy. Braz J Otorhinolaryngol. 2008, 74:718-724.
13. Di Francesco RC, Komatsu CL. Melhora da qualidade de vida em crianças após adenoamigdalectomia. Rev Bras Otorrinolaringol. 2004, 70:748-751.
14. Mitchell RB, Kelly J, Call E, Yao N. Quality of life after adenotonsillectomy for obstructive sleep apnea in children. Arch Otolaryngol Head Neck Surg. 2004, 130:190-194.
15. Benninger M, Walner D. Obstructive sleep-disordered breathing in children. Clin Cornerstone. 2007, 9:6-12.
16. Conlon BJ, Donnelly MJ, Mcshane DP. Improvements in health and behavior following childhood tonsillectomy:a parental perspective at 1 year. Int J Pediatr Otorhinolaringol. 1997, 41:155-161.
17. Fujimori I, Goto R, Kikushima K, Hisamatsu Ken-ichi, Murakami Y, Yamada T. Investigation of oral a -Streptococcus showing inhibitory activity against pathogens in children with tonsillitis. Int J Pediatr Otorhinolaryngol. 1995, 33:249-255.
18. Flanary, VA. Long-term effect of adenotonsillectomy on quality of life in pediatric patients. Laryngoscope. 2003, 113:1639-1644.
19. Da Silva VC, Leite AM. Qualidade de vida em crianças com distúrbios obstrutivos do sono: avaliação pelo OSA-18. Rev Bras Otorrinolaringol. 2006, 72:747-756.
1. Doctor. Professor Doctor, Post-Graduation Supervisor. Professor Doctor of the Immunology Department, Supervisor of the Department of Post-Graduation of the Universidade do Oeste Paulista
2. Specialist. Doctor of the Otorhinolaryngology Discipline of the Hospital Universitário Domingos Leonardo Cerávolo.
3. Doctor of the Universidade do Oeste Paulista.
Institution: Universidade do Oeste Paulista. Department of Post-Graduation Unoeste. Presidente Prudente - SP - Brazil. Mail Address: Luiz Euribel Prestes Carneiro - Departamento de Imunologia, Universidade do Oeste Paulista - Rua José Bongiovani 700 - Cidade Universitária - Presidente Prudente / SP - Brazil - Zip code: 19050-680 - Telephone/Fax: (+55 18) 229-1013.
Article received on November 25, 2008. Article accepted on July 24, 2009.