INTRODUCTIONThe septum nasal perforation is a nosological entity of easy diagnosis; it may be due to the ample variety of etiologies, since extremely benign until local manifestation of severe systemic diseases. In addition, the septum nasal perforation vary broadly in relation to the localization, amplitude and symptomatology; thereupon the therapeutic options are multiple, including the conservative treatment and several surgical techniques, musting to be individualized for each patient. In particular regarding the surgical correction, there is not technique that be universally recommended. The option by determined strategy should be based in the etiology, in anatomical characteristics as location and amplitude of the perforation, in the availability of tissues or special materials for the correction of the defect and in the experience of the surgeon.
In the present article, we analyze the main aspects of the septum nasal perforation, with special emphasis in the revision of the development of the techniques of surgical correction. We have for objective to confront and remember peculiarities of the distinct surgical techniques for help in the surgical planning of the cases of the septum nasal perforation.
LITERATURE' REVIEWEtiology
The main cause of the septum nasal perforation is the iatrogenic, as a surgery nasal complication (1, 2), however others iatrogenic causes can occur as the use of nasal corticosteroid (3,4 and, 5), mucous membrane' cauterization for the treatment of epistaxis, nasotracheal intubation and nasal turbinates cryosurgery. In addition, there are descriptions of perforation by diverse kinds of traumas. The perforation rarely occurs in children (6).
Between the illnesses related to the septal perforation we are able to cite: Nasal abscess, syphilis, tuberculosis, typhoid fever, diphtheria, granulomatosis of Wegener, lupus erythematosus and sarcoidosis. The neoplasias and carcinomas also can cause to the perforation of the septum nasal (7, 8 and, 9). In tropical areas in development, the Leprosy and the Leishmaniose are still causes not uncommon of septal perforation (10). When the perforation of embroiders are covered by mucous membrane, hardly the perforation is related to the gravest illnesses, as tuberculosis or neoplasias (3, 1).
Inhale irritants also can cause the septum nasal perforation, as in the cases of aspiration nasal of cocaine, that determines ischemia by vasoconstriction (1), formation of granuloma by adulterants (2) beyond perforation related after inhalation of smoke of chromic acid, smoke of sulphuric acid, dust of slime and cement, pitch, tar, salt, dust of glass, sodium carbonate, nitrate of can, cyanide of calcium, arsenic, mercury and phosphorous.
For times the perforation precedes others symptoms of systemic illnesses being, therefore necessary clinical inquiry of the symptomatic cases that do not have clear etiological diagnosis (11).
Clinical Picture and Diagnosis
The symptoms are normally soft. The smaller perforations are in general more symptomatic, for it cause respiratory noise similar to whistle (12). The patient also can present sensation of nasal obstruction, explained by the turbulence caused by the passage of the air in the perforation (13,14). Anosmia is another one complains referred (15), as well as formation of crusts, nasal bleeding, of intermittent to epistaxis more severe, nose in saddle, shrinkage columellar (1, 16), fetid smell and headache (16).
The ambulatory exam with speculum and nasal endoscope permits the diagnosis of a clear way. The computed tomography has shown helpful for classify and study the perforation and his relation with other elements of the nasal anatomy (14, 17).
Conservative Treatment
The conservative treatment can be:·
o Expectant in the asymptomatic cases.
o Washings and application of ointments in the cases where the complaint restrains to the formation of crusts. Some patients relate more significant relief of the symptoms after washings with diluted syrup of glucose (Karo Honey®)(8).
o Placement of manufactured orthese for filling of the perforation (manufactured button) (18). The one of Silastic® are made in a bobbin format with distance between the disks of 3mm, thickness of each disk of 1mm, central axis with 5 mm of diameter and diameter of the disks of until 3 cm (15).
Surgical Treatment
The medical literature presents countless surgical proposals for the correction of the septal perforation and sometimes it considers some cases inoperable, as FAIRBANKS in 1980 (8).
To facilitate the study and the understanding of the techniques described we can to group them according to its surgical philosophy. So, in the beginning, we are able to divide them between that one that propose the locking of the perforation and the one that propose its enlargement.
In 1935 (19), IMPERATORI and cols. proposed the surgical increase of the perforation, in order to diminish the discomfort caused by the constant whistles caused by the smaller perforation, located in the previous part of the septum nasal (12). The enlargement produced partial relief or total of the symptoms, beyond be technically a lot simpler than the attempts of correction of the perforation.
The locking of the septal perforation requires surgical technique more refined and complex, the which are able to group according to the bases of each technique: those that rely of the own septum nasal for the filling of the ´perforation, with or without the use associated grafts, and the techniques that include neighborhood shred.
Among the techniques that utilize scraps of mucous membrane of the own one septo nasal, we find the suggestion of GOLLOM (20), that in 1968 reviewed the irrigation of the septum and proposed that the shreds include in his pedicles branches of the previous ethmoid arteries and sphenopalatines. He described a technique that consists of a hemitransfixant incision, bilateral rectangular displacement of the mucous membrane, its forward displacement, filling with cartilage and bone, followed by achievement of sutures, leaving it at side of the last shred, this technique is described as difficult for perforations bigger than 1,5 cm. In the same year GOLLOM (21) described a new technique, carrying out approach of rhinoplasty with shorting of the septum. Of analogous way, JOHNSON (22), in 1968, described a technique that combines repair and rhinoplasty, for that the septum shortened to have redundant mucous membrane enough for cover the perforation. JUDSON and BELMONT (1) described in 1985 the need of broad shreds when associated the deformities of saddle of the nasal spine and the achievement of two or three surgeries. The plastic surgeries were carried out six months after the locking of the perforation septal, taking the care of do not carry out sutures in the bloody area of the graft givers regions.
Another one surgical philosophy for the locking of the perforation included the use of shreds, that can be rolled of structures of the own nasal cavity or of more distant regions. A shred of medium seashell, rolled and sutured about the area perforated, was proposed in 1964 by Ismail and cols. (23). Already DENECKE and cols., in 1967, related the lower seashell shred use, but established that the previous perforations normally are not aligned with the head of the lower seashell, arising an important restraint to the technical one (24). This technique was later resumed by FRIEDMAN and cols. (25), in 2003, utilizing also shred of lower seashell.
TIPTON (26), in 1970, related three cases in that the perforation, with dimensions of 1.5 to 2 cm, had total locking through the utilization of shred gengivolabial; the results were maintained in periodic re-evaluations carried out to six months after surgery. TARDY in 1973 (27) and afterwards in 1977 (28) attracted attention for the good elasticity of the mucous membrane gengival when turned for the nose, in comparison to the little elasticity of the nasal mucous membrane. KRATZ (29), in 1973, utilized nasal shred since the floor, initiating lower and of opposite interest to the placement of composed graft. During the post-operative he alleged twelve days of tamponage; in the same article presents horizontal shred rotation case of mucous membrane gengival by the furrow nasolabial. SCHULTZ-COULON (30), in 1994, utilized what named shred in bridge, referring to the maintenance of vascularizated pedicle preserved in the rotation of the shred. MEYER (16), in 1994, refers to utilize previous shred for perforations until 2 cm. In bigger cases of perforation carries out the correction in three steps: first accommodating seashell of ear in subgengival pocket, in a second moment passes the mucous membrane gengival with cartilaginous graft for septal correction and finally carries out a third surgical approach for pedicle' excision. ROMO and cols. (31), in 1995, they described the use of submucosal expanders implanted in nasal floor, inflated of 0.5 to 1ml weekly to the maximum one of 3,5ml before of the surgery. With that they obtained nasal floor mucous membrane shred with dimension for the locking of the perforation. Additionally, they combined the shred of this redundant mucous membrane with graft of temporal fascia, having obtained success in all the five cases operated. The articles that suggest neighborhood shred rotation are unanimous as regards the need of a second surgical time for the excision of the vascular pedicle.
Among the techniques that utilize grafts between the shreds of mucous membrane septal, we find already in 1963 the description of the use of graft of fascia and perichondrium between the leaflets of mucous membrane septal, by WRIGHT and cols. (19). This publication had big value, so much by the as much as promising results by justify the utilization of grafts in the locking of the perforation, instead of the simple suture of embroidered. The authors relate that, beyond decrease metabolic requisition, grafts of fascia and perichondrium serve like framework for the growth of fibroblasts, maintaining the growth of the margins of the mucous membranes, an in direction to the another one. MCCOLLOUGH (32) in 1976 related the locking of septal perforation through composed graft of ear, successfully. In 1980, FAIRBANKS (9) described the utilization of temporal fascia with diameter 2 bigger cm than the perforation to be cover, having obtained success in nineteen among twenty cases operated. In this same publication he defends that small perforations occurred during surgery, have better chance of locking been corrected during the same act operative, since the diameter of the perforation tends to increase with the scarring. In the same year (8) he also did contrary considerations to the surgical techniques that propose the suture of embroidered of the perforation, with or without the eversion of the against-lateral mucous membrane due to the atrophic and friable character of the tissue of the embroidered of the perforation. He also criticizes the techniques that utilize oral mucous membrane, by the not transformation of this in ciliated tissue having as consequence the desiccation. KRIDEL and cols. (33), in 1986, they utilized successfully the periosteum of the mastoid as graft and obtained the locking of seventeen between twenty-two cases operated, utilizing technique of open rhinoplasty with grafts of temporal fascia or ethmoid bone or advance of high and low shreds. TEICHGRAEBER e cols. (2), in 1993, they described technique that consists of open rhinoplasty associated to the haul incision for better exposition, applied sick bearers of perforation caused in their big majority by septoplasties, being all in the subsequent embroidery of the quadrangular cartilage, in the juncture of the vomer with the ethmoid. They obtained success in nineteen among twenty-two patients operated. In the big perforation they utilized periosteum or temporal fascia for give force and durability to the locking, beyond permit to not requirement of the bilateral cover by shreds of mucous membrane. The authors argue that the locking of a side bears the graft of connective tissue and permits that the graft behaves like a scaffold; for the migration of the against-lateral mucous membrane. HUSSAIN and MURTHY (34), in 1997, described the utilization of a graft sandwich; composed by deep temporal fascia, tragal cartilage and temporoparietal fascia.
Artificial material use suggestions, or implants, as association to the techniques of locking, include the proposal by GYENEY and KERENYI (35), in 1977, that related the correction of septal perforations through implants of fibrin (Bioplast®). KRIDEL and cols. (36), in 1998, they suggested the utilization of an acting one biosynthetical (Acellular Human Dermal Allograft®), having related success in the locking of eleven among twelve treated perforations. In case of failure had reduction of the diameter of 3 cm for 5 mm. The authors did criticisms to the utilization of fascias, mainly by the need of utilize material for dry them, what leads to its early softening, causing difficulty of manipulation. In 2006, LEE and cols. (37) they showed the glue use utility of fibrin and autologous graft of cartilage for the prevention of perforation of the septum during septoplasty.
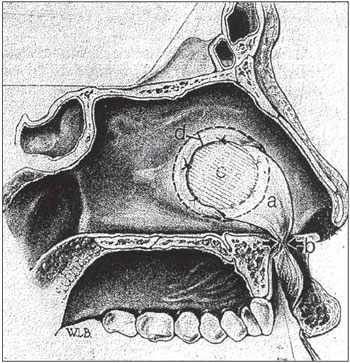
Figure 1. Gengivolabial Schred (Tipton, 1970).
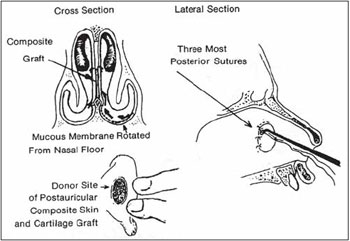
Figure 2. Compound Graft (Kratz, 1973).
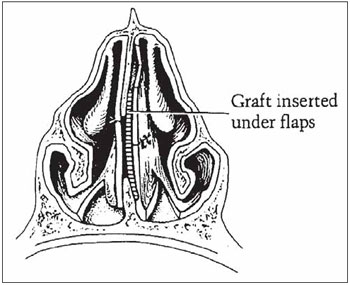
Figure 3. Temporal Fascia Graft (Fairbanks, 1980).
We observed that the literature is unanimous in recommend that in each case proceed a prudent etiologic research, since the perforation of the septum nasal is able to in some cases be manifestation of severe nosological entities. We judge useful the information that when embroiders of the perforation are covered by mucous membrane, hardly the perforation is related to the gravest illnesses, as tuberculosis or neoplasias. In the cases of iatrogenic perforations occurred during septoplasties, is preferably its immediate correction, since the perforation tend to increase with the scarring.
The surgical options vary since the enlargement of small perforation of the previous part of the septum, for relief of the discomfort represented by resulting whistles of the air stream through the defect, until to those that rely shred, both of the septum nasal to the filling of the perforation, with or without the associated grafts, as that one which include neighborhood shreds.
The rhinoplasty with shortening of the septum in special cases can be sufficient for the correction of the defect being able to supply sufficient redundant mucous membrane for cover the perforation.
We observed that among the multiple options suggested for the correction of the septal perforation, the most frequent utilize shreds of the own one septum nasal, rolled over the area of the perforation, maintained in position by means of sutures or biological glues, and interpolated with grafts of cartilage or fascia. Those grafts sounds to have a prominent function in the surgical success, serving like structural screen for the scarring of the shreds, beyond isolation between the septal leaflets, in the attempt of stop the recurrence of the perforation. Its presence would stop the contact between the embroidered cicatricials of the leaflet of opposite side of the septum, what would result in recurrence of the perforation.
It is fundamental that it preserve the irrigation of the shreds, recommending the enclosure in its pedícles of branches of the previous ethmoid arteries and sphenopalatines, when originating from mucous membrane of the own one septum nasal. The simple suture of embroider of the perforation have like an impediment the atrophic and friable character of the mucous membrane of this region.
Final Comments
All the perforations should have its etiology investigated. The iatrogenic perforations of the septum nasal in the septoplasties should be ready corrected. In the cases of option by surgical correction must be taken into account a good exposition, adequate blood supply, when necessary grafts support and attention for that the suture of the embroidered be free of tension exaggerated.
BIBLIOGRAPHICAL REFERENCES1. Judson MAJ, Belmont R. An approach to large nasoseptal perforations and attendent deformity. Arch Otolaryngol. 1985, 111(7):450-455
2. Teichgraeber JF, Russo RC. The management of septal perforations. Plast Reconstr Surg. 1993, 91(2):229-235.
3. Miller FF. Ocurrence of nasal septal perforation with use of intranasal dexamethasone aerosol. Ann Allergy. 1975, 34(2):107-9.
4. Ferguson BJ. Nasal steroid sprays and septal perforations. ENT J. 1997, 76(2):75-6.
5. Soderberg-Warner ML. nasal septal perforation associated with topical corticosteroid therapy. J Pediatr. 1984, 105(5):840-1.
6. Bridger GP. Surgical closure of septal perforations. Arch Otolaryngol Head Neck Surg. 1986, 112(12):1283-5.
7. Fairbanks DNE, Chen SCA. Closure of large nasal septum perforations. Arch Otolaryngol. 1970, 91:403-406.
8. Fairbanks DNE, Fairbanks GR. Nasal septal perforation: Prevention and management. Ann Plast Surg. 1980, 5(6):452-459.
9. Fairbanks DNF. Closure of nasal septum perforation. Arch Otolaryngol. 1980, 106(8):509-513.
10. Goulart IMB, Patrocínio LG, Nishioka SA, Patrocínio JA, Ferreira MS, Fleury RN. Concurrent leprosy and leishmaniasis with mucosal involvement. Lepr Rev. 2002, 73(2):283-284.
11. Diamantopoulos II, Jones NS. The investigation of nasal septal perforations and ulcers. Laryngol Otol. 2001, 115(7):541-4.
12. Imperatori CJ, Burman HJ. diseases of the nose and throat. Hagerstown, Md, Harper & Row Publishers Inc, 1935, pp 122-124.
13. Grutzenmacher S, Mlynski R, Lang C, Scholz S, Saadi R, Mlynski G. The nasal airflow in noses with septal perforation: A model study. ORL J Otorhinolaryngol Relat Spec. 2005, 67(3):142-7.
14. Imperatori CJ, Burman HJ. Diseases of the nose and throat. Hagerstown,Md, Harper & Row Publishers Inc, 1945, pp 96-975.
15. Facer GW, Kern EB. Nonsurgical closure of nasal septal perforations. Arch Otolaryngol. 1979, 105(1):6-8.
16. Meyer R. Nasal septal perforations must and can be closed. Aesthetic Plast Surg. 1994, 18(4):345-55.
17. Rettinger G, Hosemann W. Measuring the size of nasal septal perforations. A simple radiological method. Rhinology. 1988, 26(3):157-9.
18. Price DL, Sherris DA, Kern EB. Computed tomography for constructing custom septal buttons. Arch Otolaryngol Head Neck Surg. 2003, 129(11):1236-1239.
19. Wright WK. Tissues for tympanic grafting. Arch Otolaryngol. 1963, 78(3):291-296.
20. Gollom J. Perforation of the nasal septum: The reverse flap technique. Arch Otolaryngol. 1968, 88:84-88
21. Gollom J. Perforation of the nasal septum. Arch Otolaryngol. 1968, 88:518-522.
22. Johnson NE. Septal perforations and secondary septal surgery. Laryngoscope. 1968, 78:586.
23. Ismail HK. Closure of septal perforations: A new technique. J Laryngol Otol. 1967, 78:620-623.
24. Denecke HJ, Meyer R. Plastic surgery of head and neck: Corrective rhinoplasty. New York, Springer-Verlag, Vol. 1, 1967.
25. Friedman M, Ibrahim H, Ramakrishnan V. Inferior turbinate flap for repair of nasal septal perforation. Laryngoscope. 2003, 113(8):1425-8.
26. Tipton JB. Closure of large septal perforations with labial-buccal flap. Plast Reconstr Surg. 1970, 46(5):514-515.
27. Tardy ME. Septal perforations. Otolaryngol Clin North Am. 1973, 6:711-713.
28. Tardy ME. Practical suggestions on facial plastic surgery - how i do it. Sublabial mucosal fiap: Repaír of septal perforations. Laryngoscope. 1977, 87:275-278.
29. Kratz RC. Repair of septal perforations with composite grafts. Arch Otolaryngol. 1973, 98(6):380-82.
30. Schultz-Coulon HJ. Experiences wíth the bridge-fiap technique for the repair of large nasal septal perforations. Rhinology. 1994, 32:25-33.
31. Romo T, Jablonski R, Shapiro A, McCormick S. Long-term nasal mucosal tissue expansion use in repair of large nasoseptal perforations. Arch Otolaryngol Head Neck Surg. 1995, 121(3):327-331.
32. Mc Collough EG. An approach to repair of septal perforations. ORL Digest. 1976, 38:13.
33. Kridel RW, Appling WD, Wright WK. Septal perforation closure utilizing the external septorhinoplasty approach. Arch Otolaryngol Head Neck Surg. 1986, 112(2):168-72.
34. Hussain A, Murthy P. Modified tragal cartilage: Temporoparietal and deep temporal fascía sandwich graft technique for repair of nasal septal perforations. Laryngol Otol. 1997, 111:435-437.
35. Gyeney L, Kerenyi G. Bioplast fibrin implants in nasoseptal perforation. Arch Otorhinolaryngol. 1977, 218(1-2):143-5.
36. Kridel RW, Foda H, Lunde KC. Septal perforation repair with acellular human dermal allograft. Arch Otolaryngol Head Neck Surg. 1998, 124(1):73-8.
37. Lee JY, Lee SH, Kim SC, Koh YW, Lee SW. Usefulness of autologous cartilage and fibrin glue for the prevention of septal perforation during septal surgery: A preliminary report. Laryngoscope. 2006, 116(6):934-7.
1. Doctor Otorhinolaringologist. Specialist. Master in Othorinolaringology by the Medicine School of the Holy House of São Paulo Cashier CNPq.
2. Doctor in Medicine with Area of Concentration in Otorhinolaringology by the Medicine School of the Holy House of São Paulo. Professor and Adviser of Master and Doctorate in the Medicine School of the Holy House of São Paulo.
3. Doctor in Medicine with Area of Concentration in Othorinolaringology by the Medicine School of the Holy House of São Paulo. Member Titrate of the Brazilian Society of Plastic Surgery. Professor of Othorinolaringology and Plastic Surgery in the Institute Felippu.
4. Doctor Otorhinolaringologist. Specialist. Master in Otorhinolaringology by the Medicine School of the Holy House of São Paulo Scholarcashier CAPES.
Institution: Medicine School of the Holy House of São Paulo. São Paulo / SP - Brazil. Mail Address: Eulógio Martinez - 444, Antonio José Thomaz da Costa, St - Novo Campeche - Florianópolis / SC - Brazil - ZIP CODE: 88063-610 - Telephone: (+55 48) 9911-5575 - E-mail: eulogioneto@terra.com.br. Article received on January 23, 2009. Article approved on October 06, 2009.