INTRODUCTIONThe human nose's function is highly dependent on the dynamics of the air flow, since the geometry variation of the nasal cavity suggests an impact on the flow and the standard of this flow and, accordingly, the nasal function. However, ambiguous data about the mechanics of the air flow in the nasal cavities is still found in literature (1).
Nasal obstruction is a frequent symptom in otorhinolaryngological clinics, affecting individuals at all ages, from the newly-born to the elderly, and in working environments as well. In addition to the anamnesis and anterior and posterior rhinoscopies, nasal fiberoptic scope and computed tomography can be useful for the diagnosis. However, despite all these resources, quantifying the complaint of nasal obstruction in an objective way for a better analysis is not possible yet (2).
Objective evaluation tests of the nasal permeability should be comfortable to the patient, accurate, standardizable, easily performed, clinically applicable and they should not interfere with the nasal anatomophysiology. Besides, its reproducibility is essential, which is the test resource to produce reliable and consistent results when they are independently repeated (3). They are used to evaluate the functional and morphological alterations in the nasal cavity, in the turbinate hypertrophy-related obstructive cases, nasal septum deviation, nasal polyps, and also in the inflammatory and infectious causes, such as viral rhinitis, infectious rhinosinusitis, among others.
The most currently used objective methods to study the nasal flow are computer-assisted rhinomanometry, acoustic rhinometry and peak nasal inspiratory flow (PNIF) (4). The first one gauges the air flow throughout its extension in the nasal cavity, the second one measures the areas of transverse incision in predetermined points of the nasal fossa (5), and PNIF, as revealed by the name, measures the peal nasal inspiratory flow (6). Accordingly, they are useful to help diagnose and monitor the pharmacologic and immunologic treatment of the abovementioned pathologies with a special utilization in work-related rhinitis (7, 8).
Recently, the nasal obstruction-related Visual Analogue Scale (VAS) has been proposed as an important and reliable parameter to subjectively evaluate the nasal obstruction, mentioned by the patient him/herself (9). Some authors found a strong correlation of this method with rhinomanometry to measure the nasal obstruction in individuals with persistent allergic rhinitis (10, 11).
As one of the objective evaluation methods, PNIF is deemed to be a measurement that indicates the peak nasal flow of air achieved during forced inspiration. Not only is this method reproducible but it has also been used simultaneously with other objective tests (12-15). To measure PNIF, a device simply measuring the air flow penetrating in the nasal cavity during a quick inspiration and forced by the nose is used. To enter the nasal cavity, the air passes through the tube and the maximum peak flow is registered in liters/minute (16). Inspiration must be made with patient in orthostatic position and the result will be registered in the stop point of the device diaphragm after inspiration. Measurement is easily observed by a scale in l/min at the lateral of the apparatus. Its utilization requires a minimum instruction of the patient and it is easily executed and used, thus showing a similar sensibility and accuracy to the aforementioned methods. Both rhinomanometry and peak nasal inspiratory flow have a good accuracy to detect nasal obstructive alterations, with a sensibility of 0.77 vs. 0.66 and the specificity of them both is 0.8, with a diagnostic accuracy around 0.75 (16, 17). The cutting value is the average value used by some authors to classify to what extent the indexes are in the normality range for a certain parameter. In this case, for normal individuals regarding the nasal obstruction, PNIF value is at least 120 l/min, with a difference of nearly 35% before and after using a decongestant (1, 16, 17, and 18). Using a topic decongestant reduces the resistance for air passage through the nasal fossas by causing a reduction in the volume of mucosa and, as a result, in the size of turbinates. This is a situation of a harsh change in the nasal patency (19). In many works and studies, this is the method used to induce nasal alterations when intending to evaluate the degree of nasal obstruction.
In Brazil, among the methods to objectively gauge the existent nasal patency, acoustic rhinometry and rhinomanometry are by far the most noteworthy ones (20). Even so, such methods are still hardly spread nationwide, especially because of its high costs and complexity of utilization, what, for instance, turns them unfeasible for an extensive occupational utilization. Hence, a huge difficulty in evaluating the nasal obstruction efficiently and simply is observed in our routine, with objective data when such methods are not available. A practical, swift, portable, reliable and low-cost method is, therefore, wanted.
The objective of this work is to evaluate the correlation between PNIF and VAS for nasal obstruction before and after a change occurred in the nasal patency caused by the topic vasoconstriction.
METHODThis study was approved by the Research Ethics Committee of the institution under protocol Nº 824/2009. All volunteers received and signed the free and clarified term of agreement beforehand.
The present work is a quasi-experimental study in which the studies variants are PNIF and VAS in two consecutive moments (before and after nasal vasoconstriction) in a 50-adult group with no nasal respiratory complaints. To join this cohort, participants had to be between 18 and 65 years old, volunteers to the study, they could neither present nasal respiratory diseases nor have counter-indications to use a nasal decongestant. 50 (fifty) volunteers were selected with these characteristics, being 29 female and 31 male. The adopted exclusion criteria were: individuals with alterations or deformities of nasal anatomies (obstructive septum deviation, nasal polyps or mass, alterations in the nasal pyramid and craniofacial malformations); infections of the upper airways in the last 14 days; history of previous nasal or palate surgery; chronic use of nasal decongestant or corticosteroid and eventually have any counter-indication to use a nasal decongestant. To ensure these criteria have been met, participants were submitted to an anamnesis, physical examination and nasal fiberoptic scope, and they also filled out a questionnaire.
The examinations were preformed in an otorhinolaryngological office, comprised of a room with an examination chair, table, air-conditioning system keeping environmental temperature between 22-24oC, materials to disinfect PNIF, chlorhexidine, alcohol at 70%, oxygenated water and neutral liquid soap. PNIF-measuring device used belongs to Clement Clark International Limited trademark, model IN-CHECK ORAL ATM (Figure 1). Firstly, there was a period of acclimation with the volunteer sitting for 20 minutes in the test environment. In this period, an anamnesis and physical examinations were performed. Secondly, PNIF was applied for three successive times to register the highest measurement and fill VAS (Figure 2). Thirdly, a nasal decongestant was applied to both nostrils and 10 minutes were waited before repeating measurements.
PNIF-measuring equipment is comprised of a mask-inducing sealing when it is positioned on the patient's face. This mask is turned onto a plastic cylinder through which the air passes during inspiration. Inside this cylinder, there is a diaphragm that moves to the air flow, and the maximum peak flow is registered in a scale range from 30-370 l/min.
All the individuals were examined by the same otorhinolaryngologist doctor by way of an anamnesis, physical examination and they were requested to fill out a standardized questionnaire of signs and symptoms prior to test performance. Next, all the individuals informed their degree of nasal obstruction during normal breathing, with both nostrils being freed, and they signaled VAS for nasal obstruction. They were subsequently submitted to peak nasal inspiratory flow measurements. Ten minutes after applying 5 drops of decongestant solution (oxymetazoline chloride 0.05% - Afrin) in both nostril nasal fossas of all volunteers, PNIF and VAS were again measured to evaluate the variations in the measurements before and after using the nasal decongestant.
To perform PNIF test, the individual was placed in an orthostatic position and he was asked to expire completely. Immediately afterwards, the examiner strongly put PNIF mask on the volunteer's face and asked him/her to inspire nasally as strongly as he/she could, and the measurement was recorded in the apparatus. All the measurements were obtained by the same examiner. Three measurements were obtained for each individual. The highest PNIF measurement was regarded as the test result.
Some considerations were important to perform PNIF. The participant must stay in supine position; inspiration must be swift and short; special care must be taken when placing the mask on the individual's face to seal it perfectly and avoid an excessive pressure on the nasal dorsal area. This could cause a bonding of the nasal valve, causing a measurement sloping. Three successive takes must always be formed so that the participant can fully understand the method. Failing to observe these conditions can lead to a wrong interpretation of results.
Special care must be taken when using the nasal decongestant. Since it is an agonist, this drug directly functions in the capillaries of the nasal mucosa and causes a reduction in the blood volume of the mucosa. Its utilization, however, is not exempt from side effects, even though they are rare, especially in the cardiovascular system. Hence, it was explained to the participants the likelihood of cardiac arrhythmias and/or crises of arterial hypertension, and the Researcher Doctor remained entirely responsible for providing any support whichsoever, whenever required, in the hospital environment.
RESULTSAt Tables 1A and 1B, equilibrium was observed between the sexes, with an average age of 33.
At Table 2, it can be observed that the average value found for pre-vasoconstriction VAS was 4.1 and, for post-vasoconstriction, it was 2. This represented a 44% range between the measurements.
With regard to PNIF values, the average found when measuring the vasoconstriction was 151 l/min and 178 l/min after vasoconstriction, showing a 20% increase.
In Graphics 1 and 2, it was noted an inversely proportional linear correlation between the values achieved for PNIF and VAS before and after nasal vasoconstriction, i.e., the higher the values achieved in PNIF measurement the lower the values related to VAS (Table 3).
This relation was evaluated at moments before and after nasal vasoconstriction, from the model of simple linear regression. Dependant variant was log (PNIF). Independent variant was VAS.
At the pre-vasoconstrictor moment, the range of a point in average VAS value corresponds to a 3.8% decrease in average PNIF value. In the post-vasoconstriction, each increase of a point in average VAS value corresponds to a 4.5% decrease in average PNIF value.

Figure 1. PNIF.
Figure 2. EVA - Visual analogue scale for the degree of nasal obstruction.
For clinical purposes, PNIF is frequently used in the air flow evaluation, especially because of its simplicity and non-invasive nature (3).
Visual Analogue Scale (EVA), in turn, which also presents these characteristics, was used in the present study to quantify the subjective sensation of nasal obstruction.
The nasal congestion is a very common symptom observed in otorhinolaryngological practice. It can be associated with chronic diseases such as rhinitis and rhinosinusitis or only related to the nasal cycle and the changes of posture and decubitus (21). Septum deviations can impact the nasal patency for directly obstructing the air flow, commonly seen in caudal nasal septum, or in cases where the deviated septum touches the anterior area of the inferior nasal conchae when it is congested due to the nasal cycle (22).
Many works showed different results when searching a positive association between the objective measurement of the nasal patency and the subjective complaints of congestion (19). JONES et al. (1989) performed a rhinomanometric study with 250 patients coming from a reference hospital and no correlation was found (23). PANAGOU et al. (1998) performed a similar study with 254 individuals, and through the technique of partial correlation coefficient between the samples, a weak association was found (24). FAIRLEY et al. (1993) achieved a good correlation by using PNIF and subjective scales of nasal symptoms in 169 individuals (11). CLARKE et al. (1995) surveyed 20 individuals with PNIF and rhinomanometry before and after a nasal decongestant was used. A positive association was observed between the methods, having rhinomanometry attained slightly better results to capture the changes in the nasal patency (25).
The present study provides evidences that there is a strong correlation between PNIF and VAS findings with respect to nasal obstruction, even when nasal decongestant is used as a comparative parameter. It could be observed that the average value found for pre-vasoconstriction VAS was 4.1 and the average VAS value found after nasal vasoconstriction was 2. As to PNIF value, the average found in pre-vasoconstriction measurement was 151 l/min, while in post-vasoconstriction it was 178 l/min, showing an average increase in 20%. PNIF was considered an important supplementary examination to support the diagnosis of nasal obstruction. TEIXEIRA et al. found, in individuals with rhinitis, an average PNIF value of 114 l/min and 154.3 l/min in healthy individuals. This was a statistically significant difference, what corroborates to enable PNIF to help diagnose obstruction. In another study, it was adopted a cutting level for symptomatic individuals of 120 l/min, with a sensibility and specificity above 75% (7).
In a study carried out with 303 healthy volunteers, a subjective graduation of the nasal obstruction was completed in three levels: Group 1 - nose entirely permeable by air; group 2 - partially permeable; and group 3 - entirely blocked. By using a confidence interval of 95%, it was observed that PNIF measurement for group 1 was 82-227 l/min, for group 2 was 91-180 l/min, and group 3, 86.105 l/min. This data shows a strongly positive association between measurement and subjective criteria (19). A major study performed by KJÆRGAARD et al in 2008 with 2523 people analyzed both methods of objective measurement of the nasal patency (acoustic rhinometry and PNIF) in opposition with a qualititative method (questionnaire of signs and symptoms). The study indicated a significant association between the subjective sensation of nasal obstruction and the corresponding measurement of area, space and flow (6).
There is no proper popularization of the methods of objective gauging of the nasal patency, thus prevailing acoustic rhinometry and rhinomanometry. In Brazil, they are restricted to just a few health care centers, since they need a computer for analysis and they are expensive. As a result of the high cost and its implementation complexity, these methods become unfeasible to be used in the occupational environment, as, for instance, in recruitment tests. A scarcity of devices objectively measuring the nasal obstruction is observed. Consider, for example, a man complaining about nasal congestion and the physical examination appears to be normal. In another hypothetical situation, in an occupational environment like a galvanic metallurgic industry, where a group of workers of a same department complains about nasal obstruction and rhinitis symptoms more than workers in other departments. Notice how the objective evaluation would contribute to guide a therapeutic test in the first case, or even function as a mass recruitment test for the workers in the second example to adopt measurement of joint protection.
Thinking about popularizing some method that would be more accessible, CIPRANDI et al in 2009 correlated the findings of rhinomanometry and VAS in 50 patients with allergic rhinitis. In this study, it was verified a strong association between the methods, enabling Visual Analogue Scale for nasal obstruction to function as a good method to evaluate nasal congestion (10). Similar values were achieved in a study, n which it was observed a strong association between VAS and acoustic rhinometry for nasal obstruction, making it a good analyst for nasal obstruction. Still according to the authors, VAS can be used in clinical practice to quantify the nasal obstruction (20). TEIXEIRA et al showed in a study that there is a significantly linear correlation between PNIF value and Visual Analogue Scale, i.e., the bigger the nasal obstruction mentioned by the participant the lower the value expected for PNIF.
Therefore, these preliminary results indicate PNIF utilization as an efficient method to measure the change of nasal obstruction.
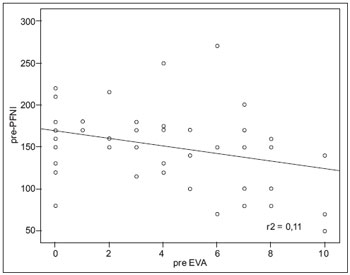
Graphic 1. Pre-PFNI and EVA values (n=60).
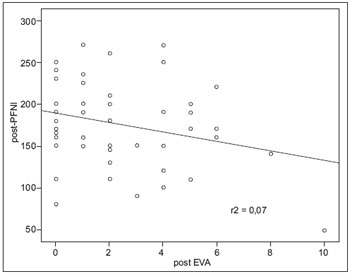
Graphic 2. Post-PFNI and EVA values (n=60).
The present study proved that there is an important correlation between the objective measurement of the nasal obstruction through PNIF and the subjective measurement provided by VAS before nasal vasoconstriction. A similar correlation between such methods can also be observed after a harsh change in the nasal patency after the nasal decongestant was used. However, such results must be carefully evaluated, since other studies with more significant samples are required to thoroughly understand and utilize PNIF.
BIBLIOGRAPHICAL REFERENCES1. Kjærgaard T, Cvancarova M, Steinsvag SK. Relation of Nasal Air Flow to Nasal Cavity Dimensions. Arch Otolaryngol Head Neck Surg. 2009, 135(6):565-570.
2. Nigro JFA, Nigro CEN, Mion O, Júnior JFM, Voegels RL. Avaliação Objetiva da Permeabilidade Nasal por meio da Rinometria Acústica. 2003, 7(4):310-5.
3. Pallanch JF, Mccaffrey TV, Kern EB. Evaluation of Nasal Breathing Function. In: Cummings CW, Fredrickson JM, Harher LA, Krause CJ, Shuller DE, (eds.). Otolaryngology - Head and Neck Surgery. St Louis: Mosby-Year Book; 1993. 2nd Ed:p.1-59.
4. Roithmann R. Avaliação da Função Respiratória Nasal. In: Lopes FO, Campos CAH. Tratado de Otorrinolaringologia. São Paulo: Editora Roca; 2003.(I):p.640-654.
5. Roithmann R, Cole P, Chapnik J, Shpirer 1, Hoffstein V, Zamel N. Acoustic rhinometry in the evaluation of nasal obstruction. Laryngoscope. 1995, 105:275-81.
6. Kjærgaard, T, Cvancarova M, Steinsvåg SK. Relation of Nasal Air Flow to Nasal Cavity Dimensions. Laryngoscope. 2008, 118:1476-1481.
7. Costa GGO, Ctenas BB, Takahashi DY, Mion O, Júnior JFM, Butugan O. Comparação entre a Rinometria Acústica, "Peak Flow" Nasal Inspiratório e sua Correlação com Sintomas e Sinais Clínicos de Rinite. Arq Otorrinolaringol. 2005, 9(3):203-211.
8. Pignatari S, et al. Obsrução nasal. Revista Brasileira de Medicina. 2010, 67:3-13.
9. Bousquet PJ, Combescure C, Neukirch F, et al. Visual analog scales can assess the severity of rhinitis graded according to ARIA guidelines.Allergy. 2007, 62:367-72.
10. Ciprandi et al. Visual analog scale (VAS) and nasal obstruction in persistent allergic rhinitis. Otolaryngology-Head and Neck Surgery. 2009, 141(4):527-529.
11. Fairley JW, Durham LH, Ell SR. Correlation of subjetive sensation of nasal patency with nasal peak flow rate. Clin Otolaringol. 1993, 18:19-22.
12. Jones AS, Viani L, Phillips D, Charters P. The objective assessment of nasal patency. Clin Otolaryngol Allied Sci. 1991, 16(2):206-211.
13. Holmström M, Scadding GK, Lund VJ, Darby YC. Assessment of nasal obstruction: a comparison between rhinomanometry and nasal inspiratory peak flow. Rhinology. 1990, 28(3):191-196.
14. Starling-Schwanz R, Peake HL, Salome CM, et al. Repeatability of peak nasal inspiratory flow measurements and utility for assessing the severity of rhinitis. Allergy. 2005, 60(6):795-800.
15. Ganslmayer M, Spertini F, Rahm F, Terrien MH, Mosimann B, Leimgruber A. Evaluation of acoustic rhinometry in a nasal provocation test with allergen. Allergy. 1999, 54(9):974-979.
16. Jose J, Ell SR.The association of subjective nasal patency with peak inspiratory nasal flow in a large healthy population. Clinical Otolaryngology. 2003, 28(4):352-354.
17. Moscato, G., et al. EAACI position paper on occupational rhinitis. Respir. Res. 2009, 10:09-16.
18. Pallanch JF, MacCaffrey TV, Kern EB. Normal nasal resistance. Otolaringol Head Neck Surg. 1995, 93:778-85.
19. Hofmam BB. Drogas ativadoras dos receptors adrenérgicos & outras drogas simpaticomiméticas. In: Katzung BG; Farmacologia Básica & Clínica. São Paulo: Guanabara- Koogan; 1998. 6º Ed: p. 92-104.
20. Zancanella E, Lima WTA. Uso da rinometria acústica como método diagnóstico. Rev Bras Otorrinolaringol. 2004, 70(4):500-3.
21. Davis SS, Eccles R. Nasal congestion: mechanisms, measurement and medications. Clin. Otolaryngol. 2004, 29:659-666.
22. Meirelles RC. Exame da Cavidade Nasal e Tratamento Cirúrgico da Obstrução Nasal. Revista do Hospital Universitário Pedro Ernesto, UERJ. 2008, 7 (jul/dez):24-32.
23. Jones AS, Willatt DJ, Durham LM. Nasal airflow: resistance and sensation. J. Laryngol. Otol. 1989, 103:909-911.
24. Panagou P, Loukides S, Tsipra S, et al. Evaluation of nasal patency: comparison of patient and clinician acessements with rhinomanometry. Acta Otolaryngol. 1998, 118:847-851.
25. Clarke RW, Jones AS, Richardson H. Peak nasal inspiratory flow - the plateau effect. J. Laryngol. Otol. 1995, 109:399-402.
1 Otorhinolaryngologist Doctor. Taking Master Degree in Public Health at FCMN/UNICAMP.
2 Resident Doctor of the Otorhinolgaryngology Department of Santa Casa de Misericórdia de Campinas.
3 Doctor in Public Health. Cooperating Professor of the Post-Degree Program in Public Health and at FCM/UNICAMP's Otorhinolaryngology, Head and Neck Department.
Institution: Santa Ca sa de Misericórdia de Campinas. Campinas / SP - Brazil. Mailing address: Santa Casa de Misericórdia de Campinas / Hospital Irmãos Penteado - Dr. Rodrigo Ubiratan Franco Teixeira - Rua Saldanha Marinho, 713 - Centro - Campinas / SP - Brazil - ZIP Code: 13013-081 - Telephone: (+55 19) 3231-3518 - Email: residenciaimc@yahoo.com.br
Article received on October 19, 2010. Article approved on December 30, 2010.