INTRODUCTIONTonsillectomy associated or not to adenoidectomy is one of the oldest and mostly practiced surgical procedures by the medicine. Approximately 250.000 adenotonsillectomy operations are carried out in the USA per year (1). Since its first description, it has been undergoing several modifications, aiming at diminishing its complications and bleeding is the most common and feared of them (2).
Among the adenoidectomy indications hyperplasia is found in this lymphoid tissue with consequent oral breathing and serous otitis media that don't improve with clinical treatment, recurrent acute otitis media and nasosinusal infections difficult to control (3). For tonsillectomy indications the recurrent and hard to control acute infections, intense hyperplasia and peritonsillar abscess are mentioned (3). In addition to these we may associate the upper airways obstruction, snore and apnea. There are also relative indications, such as the presence of the halitosis symptom like in the caseous tonsillitis (2, 3).
The tonsillectomy is one of oldest surgical procedures, described for about 2000 years, by Celso Cornélio (4). The surgical techniques have been undergoing several modifications, first with the tonsillar dissection, described by Worthington (1907), followed by the use of Guillotine-Cutter (Whillis Y and Pybus in 1910), besides the Sluder-Ballenger's technique, introduced by Sluder in 1911 (5 and 6), then by Waugh, who improved the Worthington's technique (7, 8, 9), described the modern technique of tonsillectomy by dissection at the end of the twentieth century, and the suture of vessels (bleeding or not), was assumed by Cohen (1909) (10).
As hemorrhage remains as the most common and feared of the complications, other measures were introduced to hemostasis, such as the use of electrocauteries (4), bismuth subgallate isolated (11) or combined with adrenaline (10).
We may classify the postoperative hemorrhage into primary (<24 hours) or secondary (>24 hours) (12). Most studies confirm the primary hemorrhage is much more frequent than the secondary (13, 14) and this type of event occurs mostly between 6 and 8 ours from the postoperative (15). The primary bleeding is said to be more dangerous due to the possibility of risk of aspiration, laryngospasm, low amount continuous bleeding with a consequent collapse of the blood-circulation (13, 15). The secondary bleeding occurs rarely and is predominantly observed after the eleventh day as of the postoperative (13, 15). Some of these complications may reach a large magnitude and there is need for volemic and hematic replacing.
The objective of this study is to contribute for the awareness of the frequency of bleeding in the immediate intraoperative and postoperative period, by analyzing the frequency of hemorrhage cases, the need for hemostatic procedures, surgical reintervention and hemotransfusion.
METHODAll patients submitted to adenoidectomy and/or tonsillectomy were prospectively analyzed at the Hospital Paulista de Otorrinolaryngology - São Paulo, in the period from February 2005 to February 2007. In all cases, we requested blood count and coagulogram in the preoperative, as well as the cardiologic evaluation for surgical risk and preanesthetic evaluation with the Hospital Paulista's anesthesia group.
All surgeries were carried out under general anesthesia with orotracheal intubation, the Rose's standard position was used in all cases and was the technique employed upon mechanical dissection of the tonsillar tissue and curettage of the adenoid tissue with Beckman's curette, the hemostasis for adenoidectomy made with the use of anchored gauze wet in a mixture of about 10 grams of bismuth subgallate and 10 ml of physiologic solution, 0.9% placed in the rhinopharynx region for about 10 minutes and the tonsillectomy hemostasis was carried out with simple points separated of catgut 2.0.
After the surgery, the patients move to the post-anesthesia care unit (PACU), where they are monitored, we keep the bleeding control and they are discharged after at least 40 minutes if they feel good and have no bleeding.
The basic surgical indications were:
1 - Upper airways obstruction (with snoring and apnea)
2 - Recurrence infections
3 - Chronic tonsillitis (halitosis, caseum and related symptoms)
4 - Peritonsillar abscess
The patients who didn't present with complication after 8 hours of surgery were discharged from hospital for service follow-up. The follow-up was carried out one week and one month after the postoperative. New returns were scheduled in cases of complications that need a more frequent follow-up.
RESULTSWe studied 832 patients submitted to adenoidectomy and/or tonsillectomy, 431 (52.3%) of the male sex and 401 (47.7%) of the fe male sex (Graphic 1). The mean age was of 15.4 years that ranged from 1 year and 3 months to 45 years old. Out of the 832 procedures, 195 (23.4%) were of adenoidectomy, 254 (30.5%) tonsillectomy and 383 (46.1%) of adenotonsillectomy (Graphic 2).
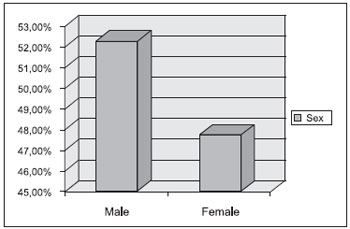
Graphic 1. Distribution by sex of patients submitted to surgery.
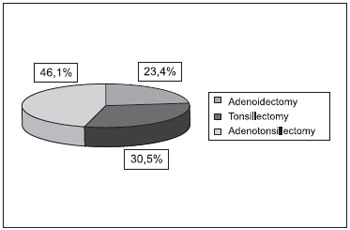
Graphic 2. Distribution of the patients by type of surgery carried out.
The obstructive symptoms formed a more frequent indication of the procedures, with 598 (71.8%) surgical indications, then the recurrent infections totalized 204 (24.5%) cases, chronic tonsillitis with 18 (2.16%) indications and peritonsillar abscess included only 12 (1.44%) patients (Graphic 3).
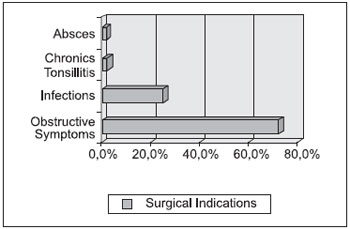
Graphic 3. Distribution of the main surgery indications.
We noted that in the patients submitted to tonsillectomy there was a higher incidence of dysphagia to liquids in the first postoperative, pain and dysphagia to solids during the first week and pain during the first month, compared to the groups submitted to adenotonsillectomy and adenoidectomy. This difference may be ascribed to the fact that the patients submitted only to tonsillectomy were in a higher age range, when compared to the other groups.
We observed hemorrhage in the first 24 hours after the procedure in only 11 (1.32%) patients, and 5 of whom had it after the adenoidectomy, in which the use of bipolar electrocautery was necessary with the help of 2 fine probes for aspiration and retraction of the soft palate with control of hemorrhage, and only 1 case needed the placing of a posterior splint with the suitable control of the hemorrhage and it was removed 24 hours without intercurrences.
The other 6 patients had it after tonsillectomy, in which we needed a surgical review for hemostasis under general anesthesia. Only 1 case needed a unit of red blood cells concentrate for the suitable hemodynamic balance. There was no death in our study.
DISCUSSIONBecause these kinds of surgery are of high frequency, it's indispensable that any surgeon who intends to practice them must have the due knowledge of the possible complications and intercurrences he may find.
Among the complication of the intra and postoperative, hemorrhage proves to be the most frequent according to several authors (9, 10, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22) and it brings more risks to the patient's life, so that its control is indispensable. Such bleeding may be reduced by research of personal and family-related precedence of bleeding, advanced suspension of certain medications that alter the blood coagulability or platelet aggregation and the request for blood count and coagulogram (23).
In all procedures we used as an ancillary substance called bismuth subgallate, which is a relatively insoluble heavy metal of poor absorption and a strong astringent power (10), which is also used by several authors in the literature (10, 11, 17, 24, 25). Studies by Thokisdottir and cols (17) showed that this heavy metal acts in the cascade of coagulation by means of the extrinsic coagulation pathway, specifically in factor XII, and causes an acceleration on the hemostatic activity. No collateral or toxic effect has been described in the literature as a hemostatic agent (24).
The literature reports an incidence of hemorrhage in the immediate postoperative of 0.28% to 7.48% (Table 1), which confirms our study assuming that 11 cases represent an incidence of 1.32% of hemorrhage in the first 24 hours as from the surgery.
In this study, out of 11 cases of postoperative hemorrhage, 5 occurred after adenoidectomy and in the remaining 6 patients after tonsillectomy, in all cases a surgical review was needed for hemostasis under general anesthesia. Only 1 (0.12%) case required a unit of red blood cells concentrate for the adequate hemodynamic balance, which is within the average in the literature studies, which states the quantity of the cases that needed blood transfusion ranged from 0% to 2.3% (26, 27).
Some authors correlated the male sex to higher chances of bleeding (10, 18, 19), which is also confirmed in our study, in which 7 out of the 11 patients were male, but other authors (20, 21) don't believe this relation and/or difference between sexes.
All patients, except for those who needed surgical review due to immediate postoperative hemorrhage, remained interned for about 8 hours, with routine prescription of analgesic and antibiotics and if necessary, antiemetic agents, aiming at the reduction of pain, fever and vomits and promoting a quicker return to the usual diet although in a recent study by Burton and col. (28) (2008), after a large literature review, concluded that there is no evidence that the use of antibiotics reduces pain or hemorrhages after tonsillectomy operations. In those who evolved with bleeding, the patients remained 24 hours in hospital under suitable observation and reposition of fluids and electrolytes.
There are several works in the literature about the importance of complications in the procedure, and there were even fatal cases (16). Therefore, the awareness of indications, technique and possible intercurrences of the surgery is crucial for a major confidence of the otorhinolaryngologist and mainly of the patient.
CONCLUSIONThe adenoidectomy and/or tonsillectomy is a safe procedure with precise indications, but it's not exempted from complications, and postoperative hemorrhage is the most frequent one. In our case report, the incidence of this event was of 1.32% and only one case required transfusion of blood cells concentrate and had no statistically significant difference.
BIBLIOGRAPHICAL REFERENCES1. Shinhar S, Scotch BM, Belenky W, Madgy D, Haupert M. Harmonic scapel tonsillectomy versus hot eletrocautery and cold dissection: an objective comparison. Ear Nose Throat J. 2004, 83(10):712-715.
2. Antunes ML, Frazatto R, Macoto EK, Vieira FM, Yonamine FK. Mutirão de cirurgias de adenotonsilectomias: uma solução viável? Rev Bras Otorrinol. 2007, 73(4):446-451.
3. Otacílio e Campos. Tratado de Otorrinolaringologia. Editora ROCA; 1994.
4. Sanchez Del Hoyo, A et al. Microcirurgia Amigdalar com Disseccion Bipolar e Analis Otorringologicos e Ibero-Americanos. 1995, 4: 379-391.
5. Feldmann H. 200 year history of tonsillectomy. Images from the history of otorhinolaryngology, highlighted by instruments from the collection of the German Medical History Museum in Ingolstadt. Laryngorhinootology. 1997, 76(12):751-760.
6. Wiikmann V, Prado FAP, Caniello M, Di Francesco RC, Miziara ID. Complicação pós-operatórias em tonsilectomias. Rev Bras Otorrinol. 2004, 70(4):464-468.
7. Worthington TC. A simple method of excision of the faucial tonsil. JAMA. 1907, 48:1761-1762.
8. Waugh GE. A simple operation for the removal of tonsil with notes on 900 cases. Lancet. 1909, 1:1314-1315.
9. Waugh GE. An operation for the excision of tonsils [letter] Lancet. 1909, 2:572.
10. Maniglia AJ, et al. Adenotonsillectomy - A safe outpatient procedure. Arch Otolaryngol Head Neck Surg. 1989, 115:92-94.
11. Mofina FD, Maniglia JV, Magalhães FP, Dafico SR, Rezende RS. A Eficácia do Subgalato de Bismuto em tonsilectomias como agente hemostático. Rev Bras Otorrinolaringol. 2000, 66(3):194-197.
12. Windfuhr JP, Ulbrich T. Post-tonsillectomy hemorrhage: Results of a 3 months follow-up. Ear, Nose and Throat J. 2001, 80(11):790-802.
13. Windfuhr JP, Chen YS. Post-tonsillectomy and adenoidectomy hemorrhage in nonselected patients. Ann Otol Rhinol Laryngol. 2003, 112(1):63-70.
14. Johnson LB, Elluru RG, Myer CM. Complications of adenotonsillectomy. Laryngoscope. 2002, 112(8pt2):35-36.
15. Randall DA, Hoffer ME. Complications of Tonsillectomy and adenoidectomy. Arch Otolaryngol. Head Neck Surg. 1998, 118(1):61-68.
16. Peeters A, Soldien V. Lethal complications of the tonsillectomy. Acta Otorhinolaryng. 2001, Belg 55.
17. Thokisdottir H, Ratnoff OD, Maniglia AJ. Activation of Hageman factor (Factor XII) by bismuth subgallate, a hemostatic agent. J Lab Clin Med. 1988, 112:481-486.
18. Kristensen S, Tveteras K. Post-tonsillectomy haemorrage. A retrospective study of 1150 operation. Clin Otolaryngol. 1984, 9:347-350.
19. Colclasure JB, Graham SS. Complications of outpatient tonsillectomy and adenoidectomy: A review of 3.340 cases. Ear Nose Throat J. 1990, 69:155-160.
20. Myssiorek D, Alvi A. Post-tonsillectomy hemorrhage: An assessment of risk factors. Int J Pediatr Otorhinolaryngol. 1996, 37:35-43.
21. Tami TA, Parker GS, Taylor RE. Post-tonsillectomy bleeding: An evoluation of risk factors. Laryngoscope. 1987, 97:1307-1311.
22. Walker MBBSP, Fracs DGBN. Post-tonsillectomy hemorrhage rates: Are they technique dependent? Arch Otolaryngol Head and Neck Surgery. 2007, 136(4):S27-S31.
23. Vieira FMJ, Diniz FL, Figueiredo CR, Weckx LLM. Hemorragia na adenoidectomia e/ou amigdalectomia: revisão de 359 casos. Rev Bras Otorrinolaringol. 2003, 69(3):338-341.
24. Lowe DL. Adverse effects of bismuth subgallate: A further report from the Australian Drug Evaluation Committee. Med J Aust. 1974, 2:664-666.
25. Conley SF. MD, Ellision MD. MD. Avoidance of Primary Post-tonsillectomy Hemorrhage in a teaching Program. Arch Otolaryngol Head Neck Surg. 1999, 125(3):330-333.
26. Gabalki EC, Mattucci KF, Setzen M. Ambulatory tonsillectomy and adenoidectomy. Larynoscope. 1996, 106:77-80.
27. Mutz I, Simon H. Hemorrhage complications of the tonsillectomy and adenoidectomy. Experiences with 7.743 operation in 14 years. Wien Klin Wochenschr. 1993, 105:520-522.
28. Burton MJ, Archer SM. MD, Rosenfeld RM. MD. Extracts from the Cochrane Library: Antibiotics to reduce post-tonsillectomy morbity? Arch Ololaryngol Head and Neck Surgery. 2008, 139(1),7-9.
29. Paredes P, Paul P. Evaluacion de amigdalectomias y adenoidectomies relizadas em el Hospital Regional Honorio Delgado de Arequipa entre 1975 a 1995. Arequipa UNSA, 60 - set 1995
30. Zwack GC, Derkay CS. The utility of preoperative hemostatic assessment in adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 1997, 39(1):67-76.
31. Liu JH. MD, Anderson KE. MD, Willging JP. MD, Myer CM. MD, Shott SR. MD, Bratcher GO. MD; Cotton RT. MD. Posttosnsillectomy Hemorrhage: What is it and What shout be recorded? Otolaryngology Head and Neck Surgery. 2001, 127(10):1271-1275.
32. Bottino MA, Souza JCR, Martinelli RB. As vantagens do sluder na amigdalectomia. Arch. Otorrinolaringol. 2002, 6(1):51-3.
33. Krishna P. MD, Lee D. MD. Post-tonsillectomy Bleeding: A Meta-Analysis. Laryngoscope. 2001, 111(8):1358-1361.
34. Lee MSW, Montague ML, Hussain SSM. Post-tonsillectomy hemorrhage: cold versus hot dissection. Arch Otolaryngol Head and Neck Surgery. 2004, 131(6):833-836.
35. O'Leary S. PhD, Vorrath J. FRACS. Postoperative Bleeding after Diathermy and Dissecion Tonsillecomy. Laryngoscope. 2005, 115(4):591-594.
1. Otorhinolaryngologist - Fellow at the University of Graz - Austria.
2. Third Year Resident at the Hospital Paulista de Otorrinolaringologia.
3. Second Year Resident at the Hospital Paulista de Otorrinolaringologia.
Institution: Hospital Paulista de Otorrinolaringologia. São Paulo / SP - Brazil.
Mail address:
Breno Simões Ribeiro da Silva
Rua Dr. Diogo de Farias 780 - Bairro Vila Clementino
São Paulo / SP - Brazil - Telephone: (+55 11) 5087-8700
E-mail: brenosimoes21@yahoo.com.br
Article received on February 17 2009.
Accepted on May 10 2009.