INTRODUCTIONThe macroglossia is a condition that has plagued man for thousands of years. Today, the treatment of choice is surgical excision of the tongue, but before 1900, surgery was often temida (1). Only in 1673 Niels Stenssen indisputably proved that language is composed primarily of muscle (2).
The size and shape of the teeth are directly influenced by the size of tongue (3). The shape of the teeth is determined by forces employed on the teeth, especially the muscles of the tongue, lips and cheek. Due to the effects caused by the aesthetic and functional macroglossia, it is evident the need for an accurate diagnosis and treatment.
The macroglossia is classified as true when there is excessive enlargement of the language and a relative when there is an imbalance between the size of the tongue and oral cavity, resulting in insufficient space for organ (4).
The goal is to establish technical bases associated with partial glossectomy orthodontic treatment of dentofacial deformity in patients with macroglossia.
CASE REPORTThree patients underwent orthognathic surgery associated with partial glossectomy from 1995 to 1999, a multidisciplinary team - doctor and dentist. All patients had macroglossia relative and underwent clinical assessment taking into account the respiratory function, swallowing and speech deficit, as well as changes in dental occlusion and was also performed radiological evaluation.
The first patient was Edentulous upper and carries only the anterior-inferior. The main problem was manifested by the presence of steep lower dent alveolar, destabilizing the use of dentures causing joint dysfunction with severe pain. She underwent a single surgical intervention in the partial glossectomy and orthognathic surgery for targeting sub apical segment dent alveolar anterior inferior. New dentures were made.
The main problem of the second patient was the anterior open bite accompanied by difficulty in breathing and articulation of words. After treatment for orthodontic tooth alignment leveling, underwent surgery for a single suspension by corticotomy posterior maxillary Le Fort I type, reduction of mandibullary prognathism by sagittal technical branches, targeting sub apical posterior-inferior right and partial glossectomy. The orthodontic treatment was completed six months after surgery.
The third patient had mandibullary prognathism and, during orthodontic treatment in preparation for orthognathic surgery, the surgery was anticipated, since the interposition of the tongue between the back teeth did not allow the evolution of orthodontic treatment. He underwent a partial glossectomy to reduce the transverse diameter of the tongue and mandibullary prognathism by sagittal technical branches.
All patients underwent surgery under general anesthesia. We used rigid skeletal fixation with titanium plates and screws so that patients could stay without intermaxillary block in the immediate postoperative period. To control tongue edema, dexamethasone was used. The hospital stay was 48 hours. It was followed over five years. The technique used consist of segmental resection along the median raphe of the tongue and suture by planes - Figure 1. As a routine, the resected specimens were sent to histopathology, without evidence of pathologic findings. The symptoms regressed completely and all skeletal segments remained stable.
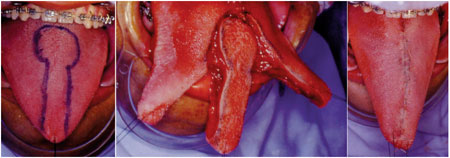
Figure 1. Demarcation and resection of the lingual and final appearance.
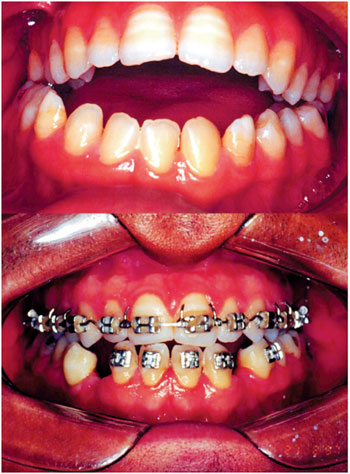
Figure 2. Aspect of pre-and postoperatively with emphasis on dental occlusion.

Figure 3. Angle of the neck in pre-and postoperatively.
The classification of macroglossia is not yet consensus in the literature. According to SHAFER (1968) (5), or primary congenital macroglossia is due to the excessive development of the musculature, which may or may not be associated with generalized muscular hypertrophy or unilateral hypertrophy. Since the secondary macroglossia may occur as a result of a tumor in the tongue, as a diffuse hemangioma or lymphangioma, neurofibromatosis, and occasionally blocking efferent vessels in cases of malignant neoplasm of the tongue. WOLFORD et al. (1996) (6) refer to as macroglossia on pseudomacroglossia, separating it from the true macroglossia. BELL et al. (1980) (7) macroglossia consider the functional as a third classification, occurring when the language does not fit into the oral cavity after a surgical procedure. VOGEL et al. (1986) (8) ranked 8th in real and relative. The true when there are histological abnormalities associated with the increase of the tongue, such as vascular malformation, stretching and tumors. Relative macroglossia includes cases of apparent increase in volume without an explanation of the language exam, as in Down syndrome.
The decision to refer the patient to partial glossectomy should be based on the volume of the language, mobility, position, function, symptoms, speech intelligibility, skeletal anterior open bite, interference in orthodontic treatment, drooling, swallowing and tongue recurrent trauma (9). The language has increased in volume expansive effect on the lower dental arch, being blamed as the cause and maintenance of open bite, bimaxillary protrusion or diastemas (10). A language has too wide an expansive force in the dental arches. Being interposed between the arches, is an important etiologic factor for malocclusion listed (Figures 2 and 3).
A partial glossectomy performed simultaneously with mandibullary osteotomy for treatment of patients with mandibullary prognathism and anterior open bite is advantageous to prevent recidivas (11). The tongue can cause deformity increased dental-muscle-skeletal, instability in orthodontic treatment and orthognathic surgery, masticatory disability, communication problems and respiratory (6). There are several clinical and radiographic findings, but not all features are always present and their existence is not necessarily path gnomonic for the diagnosis of macroglossia. Should be included the clinical, radiographic and functional for the interference with speech, mastication, airway and stability of orthodontic treatment and orthognathic surgery. There are basically three choices in the surgical sequence: (I) Stage 1: partial glossectomy, stage 2: orthognathic surgery (II) stage 1: orthognathic surgery, stage 2: partial glossectomy and (III) partial glossectomy and orthognathic surgery in a single stage surgery.
REFERENCES1. Ring ME. The treatment of macroglossia before the 20th century. Am J Otolaryngol, 1999; 20:28-36.
2. Gysel C. Renaissance considerations on the nature of the tongue. Bull Hist Dent, 1994; 42:57-60.
3. Brodie AG. Muscular factors in the diagnosis and treatment of malocclusions. Angle Orthod, 1953; 23:71-7.
4. Gasparini G. Surgical management of macroglossia: discussion of 7 cases. Oral Surg Oral Med Oral Pathol Radiol Endod, 2002; 94:566-71.
5. Shafer AD. Primary macroglossia. Clin Pediatr, 1968; 7:357-63.
6. Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop, 1996; 110(2):170-7.
7. Bell WH, Proffit W, White. Surgical correction of dentofacial deformities. Philadelphia: WB Sauders; 1980.
8. Vogel JE, Mulliken JB, Kaban LB, Macroglossia: a review of the condition and a new classification. Plast Reconstr Surg, 1986; 78(6):715-23.
9. Siddiqui A, Pensler JM. The efficacy of tongue resection in treatment of symptomatic macroglossia in the child. Ann Plast Surg, 1990; 25(1):14-7.
10. Tamari K, Shimizu K, Ichinose M, Nakata S, Takahama Y. Relationship between tongue volume and lower dental arch sizes. Am. J. Orthod. Dentofac Orthop, 1991; 100:453-8.
11. Petdachai S, Inoue Y, Inoue H, Sakuda MJO. Orthognathic surgical approach and partial glossectomy to a skeletal 3 adult open bite. Univ Dent Sch, 1993; 33:14-20.
1) Master Course for Postgraduate in Health Sciences HOSPHEL Heliopolis Hospital, Sao Paulo / SP, Brazil. Chief of Surgery Maxillo-Facial Ana Costa Hospital, Santos / SP.
2) Professor at UNILUS Lusiada Foundation, Santos. Professor of Otolaryngology and Head and Neck Surgery, Metropolitan University de Santos.
Institution: Department of Surgery Maxillo-Facial Hospital Ana Costa. Santos / SP, Brazil. Mailing address: Fued Samir Salmen - Pedro Américo Street, 60 - 7º. floor - Santos /SP - Brazil - Zip code: 11075-905 - E-mail: dedivitis.hns@uol.com.br
Article received in August 4, 2010. Article approved in November 20, 2010.