INTRODUCTIONHead and neck cancers are defined as malignant neoplasms which, if not diagnosed early, evolve with metastases and may spread throughout the body, commonly reaching the lips, oral cavity, oropharynx, nasopharynx, hypopharynx, and larynx (1-2).
The symptoms associated with laryngeal cancer depend on its location. The most common features are a feeling that something is stuck in the throat or a "scraping" in the throat, odynophagia, dysphagia, otalgia reflex upon swallowing, voice changes, and dyspnea (3). However, the growth of a malignant tumor is often totally asymptomatic and undetectable by current diagnostic methods (4).
This type of cancer occurs more frequently in men (1-8) aged over 40 years (5-8). These men tend to be manual laborers (9) and are illiterate or with little schooling (10).
Head and neck cancers have multiple causes. The most common causes are derived from endogenous (genetic) and exogenous (lifestyle and environmental) factors that, alone or in combination, cause cancer (11).
Smoking plays a prominent role among the causes related to the etiology of these cancers. The incidence of this cancer is significantly higher among smokers than among nonsmokers. Alcohol consumption is another habit that influences the initiation of these neoplasms (1-12).
We analyzed the clinical and epidemiological aspects of 43 cases of squamous cell carcinoma (SCC) of the mouth and 25 of the oropharynx, between the years 1997 to 2000 at the Department of Head and Neck Surgery, Santa Casa de Misericordia of Santos, and Hospital Ana Costa. The information collected included data relating to the profession of these patients and their tobacco and alcohol habits. Regarding occupation, most of the patients were retired or were housewives. Regarding the consumption of tobacco and alcohol among the cases of OSCC, 76.8% of the subjects were smokers and 74% consumed alcohol; 35% of the OSCC group smoked up to 40 cigarettes a day, whereas 23.2% did not smoke. In the group with SCC of the oropharynx, 48% smoked up to 40 cigarettes per day and 16% had no history of smoking (13).
Approximately 74% of patients affected by head and neck cancer were tobacco and alcohol consumers, with predominant use of commercial cigarettes and sugar cane rum (cachaça) (7).
Speech therapy in the head and neck clinic has been gaining clear relevance in recent years, especially in the rehabilitation of patients with partial and total laryngectomy because this procedure causes changes that involve the voice, speech, chewing, and swallowing. The speech therapist talks to the patient and his/her family in order to educate them about the treatment to achieve greater success of the objectives proposed by a multidisciplinary team (14).
Multidisciplinary treatment involves physicians, dentists, speech therapists, nutritionists, and psychologists, which is the ideal set of professionals to minimize or even prevent the changes resulting from the treatment of head and neck cancer. This team must be familiar with this disease so that they can take its complexity into account (15).
Phonoaudiological intervention occurs during pre-operative orientation and in the immediate post-operative period; this intervention also involves speech rehabilitation itself, which may occur at the bedside and later in the clinic or outpatient clinic (16).
Pre-operative guidance is of paramount importance to the patient because this period is the most suitable for handling the relevant information and for initiating contact with the person who will assist the patients in their rehabilitation process (4).
Therefore, the aim of this study was to determine and describe the impact of preoperative phonoaudiological orientation aimed at smokers and/or alcohol consumers diagnosed with a malignant tumor in the head and neck and who renounced tobacco and/or alcohol dependence.
METHOD This was an exploratory, descriptive, and bibliographical study. Intentional non-probability sampling was used in this study.
Inclusion criteria were patients who attended the Head and Neck Clinic of a public hospital from March 2006 to June 2007. We selected patients with a confirmed diagnosis of malignant tumor in the head and neck, upper aerodigestive tract regions [(UADT) mouth, pharynx, larynx, and esophagus] aged between 40 and 90 years who presently, or had at some point in life, the habit of consuming tobacco and/or alcohol. After consultation at the hospital, these patients received speech therapy guidelines prior to head and neck surgery in which the importance of eliminating smoking and drinking habits for a successful treatment was emphasized. Guidance regarding smoking and alcohol consumption in the study sample was provided by a professional speech therapist. The patients did not receive psychological treatment during the research. Subsequently, the patient underwent surgery at the Surgical Center of the same hospital under the care of a head and neck surgeon.
Exclusion criteria were patients diagnosed with benign tumors; patients with oral tract disorders that made them unable to consume food; patients with tumors in regions other than the UADT (mouth, pharynx, larynx, and esophagus); patients with ages outside of the 40 to 90 year bracket; and patients who had never smoked and/or consumed alcohol.
To carry out this research, it was necessary to conduct a retrospective study consisting of a survey of secondary data, such as name, sex, age, occupation, telephone, and diagnosis through medical records found in the Patient Medical Record Service (SSP) of the hospital during April 2008.
The surveyed patients received and answered a structured interview developed by researchers. Patients were contacted by telephone, were informed about the type and purpose of this study, and were ensured of the confidentiality of their identities. After the patients' questions were addressed, the patients were asked to respond to the questions contained in the interview guide. The interview took place after the patient signed a written consent form (free and informed consent).
The interview consisted of 8 simple and easy-to-understand questions related to education and life habits. Data regarding tobacco and alcohol dependence, the consumption period, and the frequency and quantity consumed were collected. Subsequently, the patients were asked if they received preoperative speech therapy guidance about the importance of abandoning tobacco and alcohol dependence and, if after such guidance (1 to 12 months), they quit smoking and/or consuming alcohol.
For this study, any patient who consumed any type or amount of tobacco daily for up to 6 months was considered a smoker; any patient who had previously smoked, but had not smoked any type or amount of tobacco in the last 6 months, was considered an ex-smoker; and any patient who never smoked any type or amount of tobacco in any period of life was considered a nonsmoker.
In this context, any patient who consumed at least 30 ml or more of alcohol daily, with a 200-ml cup as a reference, was considered an alcohol drinker. All patients who were drinkers but had not ingested any type or amount of alcohol in the past 6 months were considered ex-drinkers, and patients who had never consumed alcohol frequently were considered non-drinkers.
Initially, a total of 204 records were surveyed. We then selected patients aged between 40 and 90 years with confirmed diagnoses of malignant tumors in the regions of the UADT, thereby reducing the sample size to 118 (57.84%) patients. Of these 118 patients, we were able to contact 49 (41.52%) by telephone.
After the interview, we observed that among the 49 patients interviewed, 40 (81.63%) presently, or had at some point in life, the habit of consuming tobacco and/or alcohol. The other 9 (18.37%) who never had such habits were excluded from this study. Therefore, this study sample was composed of 40 individuals.
The collected data were compiled in a database using the software Stata 10.0, were stored on DVD in the Speech Therapy Clinic of the Estacio de Sa University of Santa Catarina, and were kept confidential. Descriptive statistics were used to analyze the variables by using graphics.
This project was approved by the Research Ethics Committee (protocol 003/2008).
RESULTSThe present study evaluated 40 patients, including 31 (77.5%) men and 9 (22.5%) women.
Of the 40 subjects aged between 40 and 90 years, 10 (25%) were aged from 40 to 50 years, 12 (30%) were aged from 51 to 60 years, 11 (27.5%) were aged from 61 to 70 years, 7 (17.5%) were aged between 71 and 80 years, and no individual was older than 81 years old (Figure 1).
Regarding education, 7 (17.5%) did they not attend school at all [illiterate], 15 (37.5%) studied for 1-4 years, 8 (20%) attended school for 5-8 years, 3 (7.5%) had attended school for 9-11 years, and 7 (17.5%) had studied for more than 11 years (Figure 2).
A feature also collected through medical records was the profession of the subjects. This variable was quite diversified. Most women (12.5%) were linked to household activity, whether caring for one's own home, working as domestic servants. To a lesser extent, the women consisted of hairdressers (5%) and retirees (5%). Among men, we found a preponderance of retirees without previous professional specification and/or medical expertise (25%) and those with professions related to manual activity, including farmers (7.5%), construction workers (5%), fishermen (12.5%), and painters (5%), among others.
Among the 40 individuals surveyed, 26 (65%) were smokers before receiving preoperative speech therapy guidelines, 13 (32.5%) were former smokers, and 1 (2.5%) was a nonsmoker (Figure 3).
Of these 26 smokers before the preoperative speech therapy guidelines, 25 (96.15%) were men and only 1 (3.85%) was a woman. In the 10 individuals who were considered former smokers, 8 (80%) were men and only 2 (20%) were women. Of the 26 smokers, 6 (23.07%) had consumed tobacco for 15-25 years, 5 (19.23%) for 26-35 years, 9 (34.62%) for 36-45 years, 5 (19.23%) for 45-55 years, and 1 (3.85%) for 56 years or more (Figure 4).
Among the 36 subjects that comprised smokers and ex-smokers, 29 (80.55%) used commercial cigarettes, 4 (11.11%) used straw cigarettes, and 3 (8.34%) reported consuming both types of cigarettes (commercial cigarettes and straw). Of these, 7 (19.44%) smoked an average of 10 cigarettes a day, 14 (38.89%) smoked an average 20 cigarettes per day, and 15 (41.67%) reported smoking more than 30 cigarettes daily.
Regarding the 40 individuals surveyed, 35 (87.5%) had been alcohol drinkers at some point in their lives, 30 (85.7%) of which were men and 5 (14.3%) of which were women. Of these, 31 (77.5%) drank alcohol assiduously before receiving preoperative speech therapy guidelines, 4 (10%) claimed that they had stopped alcohol consumption before receiving guidance, and 5 (12.5%) reported that they had never consumed alcohol (Figure 5).
Among the 35 alcohol drinkers, 5 (14.29%) consumed alcohol for 10 to 15 years, 8 (22.85%) for 16-25 years, 10 (28.57%) for 26-35 years, 10 (28.57%) for 36-45 years, 1 (2.86%) for 46-55 years, and 1 (2.86%) for 56 years or more (Illustration 9). Of these, 23 (65.71%) reported a preference for sugar cane rum (cachaça), 8 (22.86%) reported consuming more beer, 3 (8.57%) consumed wine, and only 1 (2.86%) reported a preference for another type of alcoholic beverage. However, 11 (27.5%) subjects reported consuming other types of alcoholic beverages in addition to their preferred beverages (Figure 6).
In the 35 subjects who had consumed alcohol during some period of their lives, 7 (20%) reported consuming at least 200 ml daily, 13 (37.14%) reported up to 1 liter per day, 7 (20%) consumed more than 1 liter daily, and 8 (22.86%) reported drinking alcohol only on weekends, with amounts ranging from 200 ml to more than 1 liter.
Regarding the 40 individuals surveyed, 31 (77.5%) had been both smokers and drinkers at some point in their lives, 5 (12.5%) were exclusively smokers, and 4 (10%) were exclusively drinkers (Figure 7).
Of the 26 subjects who had been smokers before the orientation, 18 (69.24%) stopped using tobacco after orientation, 4 (15.38%) did not quit smoking, and 4 (15.38 %) stopped smoking for a while. However, of these latter 4 subjects, 2 (50%) returned to smoking after 1 month, 1 (25%) resumed the habit after 4 months, and 1 (25%) started smoking again after 2 years (Figure 8).
Regarding the 31 subjects who had consumed alcohol before receiving preoperative speech therapy orientation, 17 (54.84%) stopped consuming alcohol after receiving guidance, 8 (25.81%) continued consuming alcoholic beverages, and 6 (19.35%) stopped drinking alcohol for a period of time. Of these latter 6 subjects, 4 (66.66%) resumed drinking within a period of 1 month, 1 (16.67%) resumed after 4 months, and 1 (16.67%) resumed after 1 year (Figure 9).
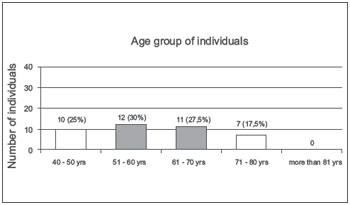
Figure 1. Age group of individuals. - Graphic distribution according to age.
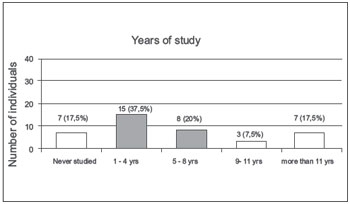
Figure 2. Years of study. - Graphic of distribution according to schooling.
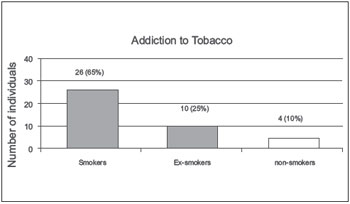
Figure 3. Addiction to tobacco. - Graphic distribution regarding tobacco dependence.
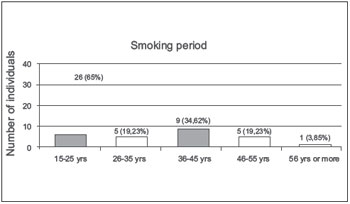
Figure 4. Smoking period. - Graphic distribution of length of smoking.
A review of the included subjects revealed that the sample was composed mostly of men. This is supported by the fact that head and neck cancers more often involve men than women (1-8).
Individuals over 40 years of age are most likely to be affected by head and neck cancers (5-8). According to the National Cancer Institute (17), mouth cancer mostly affects men over 40 years of age. The major established risk factors for this type of cancer are tobacco use (about 90% of patients diagnosed with oral cancer are smokers) and alcohol consumption (regular consumption of alcohol increases the risk of developing mouth cancer). The concomitant use of these 2 predisposing factors (tobacco and alcohol) significantly increases the risk of mouth cancer.
The incidence of head and neck cancer increases with age, and 98% of these patients are over 40 years of age in Europe (1-8). Epidemiological studies show that 13,470 new cases of oral cavity cancer occur per 100 000 inhabitants, with rates of 10,060 for men and 3,410 for women, in Brazil. Data from the National Cancer Institute (INCA) in 2005 indicated that oral cancer is the eighth most common type of malignant tumor in Brazil (12-17). Head and neck cancer represents 2% of all cancer cases in Brazilian patients, and is extremely significant in Latin America (7-10).
Most belong to the social strata associated with little schooling, studying (primary school) for 4 years on average. Similar findings were observed in studies of patients with head and neck cancer, which revealed that 21% of the patients were illiterate and 36% had little schooling (10).
Regarding the subjects' professions, we observed a predominance of blue-collar workers, retirees and housewives. Studies have shown that most of the women are housewives and the men are involved in professions such as electricians, drivers, farmers, and mechanics, among others (9-13).
Practical measures are needed to prevent cancers of the head and neck successfully. These measures include the avoidance of continuous intake of foods that are smoked and high in fat, the continuous consumption of alcohol, smoking, exposure to chemicals and ultraviolet rays, and the use of badly adjusted dentures and poor oral hygiene. Among the negative habits of the surveyed patients, we noted that commercial cigarettes were consumed more regularly than straw cigarettes (7).
The phonoaudiology team participates effectively in the multidisciplinary treatment of head and neck cancers in the pre-operative and post-operative periods by providing explanations to patients and their families in order to educate them with the aim of successful treatment. In phonoaudiology, pre-operative guidance is of great importance and includes the goals of establishing ties with and providing support and security to the patient, performing a detailed history evaluation and assessing communication skills and swallowing, and, ultimately, preparing for surgery. Post-operative complaints related to chewing and swallowing after certain head and neck surgeries require great attention, and speech therapy offers good functional results and assists in the patient's social reintegration.
The main objectives of phonoaudiological work involving patients with head and neck cancer are to ensure a better quality of life and a greater adaptation of these individuals to the functions previously performed with difficulty (i.e., chewing, swallowing, and communication). The rehabilitation of these functions usually occurs after hospital discharge.
On the basis of effective elimination of smoking and drinking habits after preoperative speech therapy orientation, as demonstrated in this study, it is evident that this guidance is important for the awareness and elimination of these habits regarding the treatment of head and neck cancers.
In this context, we emphasize the importance of preoperative phonoaudiological guidance with regard to head and neck surgery. It should be noted that phonoaudiological therapy in conjunction with assistance by other professionals is necessary because of the effects of these surgeries. The work involves multidisciplinary professionals from diverse areas, such as head and neck surgeons, nurses, oral and maxillofacial dentists, psychologists, social workers, nutritionists, phonoaudiologists, radiation oncologists, and otolaryngologists (18).
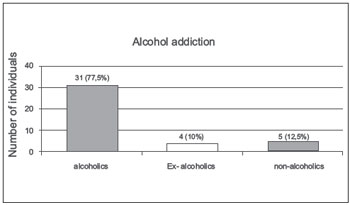
Figure 5. Alcohol addiction. - Graphic distribution regarding alcohol dependence.
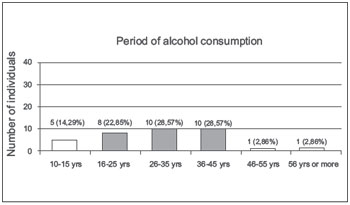
Figure 6. Period of alcohol consumption. - Graphic distribution regarding the time of alcohol consumption.
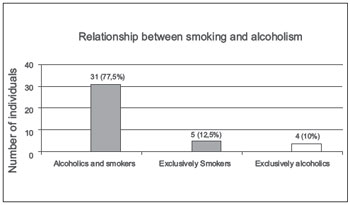
Figure 7. Relationship between smoking and alcoholism. - Graphic distribution of the relationship between smokers and drinkers.
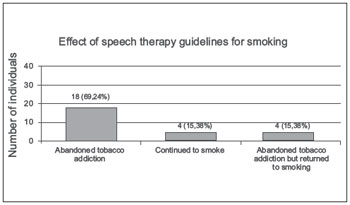
Figure 8. Effect of speech therapy guidelines for smoking. - Graphic distribution regarding the effect of speech therapy guidelines regarding smoking.
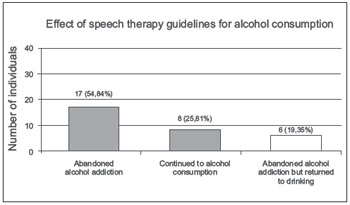
Figure 9. Effect of speech therapy guidelines for alcohol consumption. - Graphic distribution of the effect of speech therapy guidelines in relation to alcohol consumption.
The results of this study are in agreement with published data showing that cancers of the head and neck are more common in men, smokers and/or drinkers, and persons over 40 years of age. Most people are aware of the harm that tobacco and/or alcohol cause to health, and therefore renounce these habits. This proves the impact of preoperative phonoaudiological guidance on patients with head and neck tumors (on the studied site).
These results are another tool in the fight against tobacco and alcohol consumption, which includes the prevention and treatment of cancers of the head and neck. Given the size and severity of the effects produced by the consumption of tobacco and alcohol, it is of great importance that further studies be conducted and that their results be disseminated to the scientific community as well as to the general population.
We note that the integrated work of psychologists and phonoaudiologists prepares patients for the pre-surgical period, rehabilitation, and the return to their social life and family. Data from the World Health Organization (WHO) confirm the importance of quality of life in the rehabilitation of cancer patients.
Phonoaudiology, especially when incorporated in the hospital environment, can contribute quite effectively to the improvement of the quality of life of patients with head and neck cancers. Scientific production regarding phonoaudiology and its dissemination has been progressively increasing, ensuring the recognition of the importance of phonoaudiology in cases of head and neck cancers.
REFERENCES 1. Russo A, Ruiz MT, Galbiatti ALS, Cury NM, Raposo LS, Maniglia JV, Pavarino-Bertelli EC, Goloni-Bertollo EM. Câncer de cabeça e pescoço: avaliação do polimorfismo CYP2E1 [Internet]. 55º Congresso Brasileiro de Genética; 2009 30 Aug - 02 Sep; São Paulo. [cited 2009 Sep 19]. Available from: http://web2.sbg.org.br/congress/sbg2008/pdfs2009/GH223-28775.pdf
2. Angelis EC, Fúria CLB, Mourão LF, Kowalski LP. A atuação da Fonoaudiologia no câncer de cabeça e pescoço. São Paulo: Lovise; 2000.
3. Crespo A. Propedêutica da laringe. In: Angelis EC, et al., editors. A atuação da fonoaudiologia no câncer de cabeça e pescoço. São Paulo: Lovise; 2000. p. 53-60.
4. Angelis EC, Martins NMS. Orientação pré e pós-operatória em câncer cabeça e pescoço. In: Angelis EC, et al., editors. A atuação da fonoaudiologia no câncer de cabeça e pescoço. São Paulo: Lovise; 2000. p. 149-54.
5. Zender CA, Petruzzelli GJ. Why do patients with head and neck squamous cell carcinoma experience distant metastases: can they be prevented? Curr Opin Otolaryngol Head Neck Surg. 2005;13:101-4.
6. Fardin M, Rapaport M, Magalhães MR, Latorre MRDO. Fatores de risco no prognóstico do câncer de boca. Estudo de 1440 casos. Rev Bras Cir Cabeça e Pescoço. 2004; 33(1):27-33.
7. Favero E, Bittencourt M, Andrade Júnior A, Cyrillo CG, Ferraz LGC, Franzi SA. Perfil epidemiológico de pacientes da grande São Paulo com carcinoma espinocelular avançado da boca e da orofaringe. Rev Bras Cir Cabeça e Pescoço. 2007;36(3):155-8.
8. Vicente LCC, et al. Tumores de cavidade oral e orofaringe-Atuação fonoaudiológica. In: Campiotto AR, et al., editors. Tratado de fonoaudiologia. São Paulo: Tecmedd; 2005. p. 949-69.
9. Castro MG, Oliveira MSO, Moraes JFD, Miguel AC, Araujo RB. Qualidade de vida e gravidade da dependência de tabaco. Rev Psiquiat Clínica. 2007;34(2):61-7.
10. Borggreven PA, Verdonck-De Leeuw IM, Muller MJ, Heiligers MLCH, De Bree R, Aaronson NK, et al. Quality of life and functional status in patients with cancer of the oral cavity and oropharynx : pretreatment values of a prospective study. Eur Arch Otorhinolaryngol. 2007;264(6):651-7.
11. Moraes ED, et al. Tumores de cabeça e pescoço. In: Guimarães JRQ, editors. Manual de oncologia. São Paulo: BBS; 2004. p. 429-52.
12. Instituto Brasileiro de Controle ao Câncer [Internet]. [cited 2007 May 30]. Available form: http://www.ibcc.org.br/
13. Dedivitis RA, França CM, Mafra ACB, Guimarães FT, Guimarães AV. Características clínico-epidemiológicas no carcinoma espinocelular de boca e orofaringe. Rev Bras Otorrinolaringol. 2004;70(1):35-40.
14. Seif CS. Fonoaudiologia em cabeça e pescoço. In: Barbosa MM, SÁ GM, Lima RA, editors. Diagnóstico e tratamento dos tumores de cabeça e pescoço. São Paulo: Atheneu; 2001. p. 209-18.
15. Jham BC, Freire ARS. Complicações bucais da radioterapia em cabeça e pescoço. Rev Bras Otorrinolaringol. 2006;72(5):704-8.
16. Defina AP, Massih DA, Mamede RCM. Relato de experiência da atuação da Fonoaudiologia e da Psicologia a pacientes com Câncer de Cabeça e Pescoço. Rev Bras Cir Cabeça e Pescoço. 2004;33(1):45-8.
17. Ministério da Saúde, Instituto Nacional do Câncer [Internet]. [cited 2009 Mar 25]. Available from: http://www.inca.gov/
18. Nemr, Kátia. Câncer de Cabeça e Pescoço. In: Marchesan, Irene Q. Fundamentos em Fonoaudiologia: aspectos Clínicos da Motricidade Oral. Rio de Janeiro: Guanabara Koogan;2005. p. 103-15.
1) Phonoaudiologist.
2) MSc in Production Engineering (UFSC); Specialist in Educational Psychology (UNISUL) and Teaching in Distance Education (ESAB); Degree in Pedagogy (UNIGRAN) and Speech Therapy (UFSM). Professor, Universidade do Estado de Santa Catarina (UDESC).
3) MSc in Production Engineering (UFSC); Degree in Physiotherapy (UNICRUZ) and Specialist in Teaching in Distance Education (ESAB); Professor, Universidade do Estado de Santa Catarina (UDESC).
Institution: Estácio de Sá Faculty. Florianópolis/SC - Brazil. Mailing address: Raquel Fleig - Rua Júlio Dias, 605/501 - Coqueiros - Florianópolis / SC - Brazil - Zip code: 88080-060 - E-mail: fonofleig@gmail.com
Article received on September 18, 2009 - Article accepted on December 3, 2012.