INTRODUCTIONThe Mucoepidermoid Carcinomas (MEC) represent about 5% of all tumors in the salivary glands. They affect the intraoral major and minor salivary glands in more than 90% of the cases (1, 2). In the minor salivary glands it affects specifically the roof and the floor of the mouth, generally in the fifth decade of life and with a slight prevalence in the female sex. The mucoepidermoid carcinomas have been histologically classified into three degrees of malignity (low, intermediate and high degree), and such subdivision has been proved helpful for the setting up of the therapy and in the prognosis of such tumors (3, 4, 5). The early diagnosis and the correct management of this disease are key factors for the prognosis. It is an aggressive lesion and must be considered as a diagnosis hypothesis in the oral mucosa proliferative lesions, even when its clinical appearance does not suggest malignity.
CASE REPORTCT, 47 years old, white housewife from Italva/RJ, was forwarded to the ORL service of the HSJA after a critical episode of bleeding in oral cavity. She reported the appearing of a mass with fast and expansive growth in a topography of canine fossa for +/- 06 months, associated to the loss of 10 kg. The patient was lucid, examined, with regular general status, dehydrated (++/+4), pale (++/+4), with pediculated tumor of +/- 06 cm (Figure 1), firm consistency, painless with palpation, bleeding; non-palpable cervical lymph nodes. Chronic alcoholic and smoker, without family record of neoplasm. Faced with the case we opted for a surgical resection of the tumor (Figure 2) and the performance of histopathological exam that confirmed mucoepidermoid carcinoma of minor salivary glands of intermediate degree (Figure 3). The patient was sent to the radiotherapy service; but she abandoned the treatment and evolved with death 4 months after.

Figure 1. Pediculated tumor in oral cavity.

Figure 2. Surgical piece.
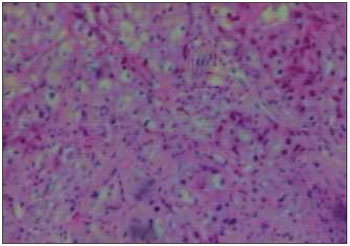
Figure 3. Optical microscopy exam of the mucoepidermoid carcinoma of minor salivary glands. Microscopy (HE 100 x).
Mucoepidermoid carcinomas (MECs) are malignant tumors from glandular structures excrectory ducts that affect the intraoral major and minor salivary glands in more than 90% of the cases (1, 2). MEC can also occur in covering glands of the maxillary sinuses, lachrymal glands, oropharynx, nasopharynx, larynx, vocal cords, trachea and lungs (2).
The etiopathogenesis of the MEC is unknown; however, as well as the other kinds of cancer, the lesion results from genetic alteration, and when altered the proto-oncogenes and the tumor suppressor genes play an important role in their pathogenesis. As procatartic factors we include exposure to ionizing radiation, previous RT, nickel refinery, chemical solvents, leather, sawing, formaldehyde, pollution (9). The MEC's histopathological characteristics are: presence of squamous cells, mucus-producing cells and intermediate cells. The predominant cellular type and its configuration vary between the tumors and inside the same tumor mass.
Clinically, MEC may manifest as a lesion of color ranging from blue to red or purple. The oral mucosa lesions, floor of the mouth, lips and retromolar region appear as asymptomatic submucous masses while tongue lesions are frequently painful. The factors relating to the MEC prognosis are: size of the primary lesion upon surgery, histological grading of the tumor and presence of metastases.
Large local resection associated or not to cervical space and eventually postoperative radiotherapy is the choice treatment for mucoepidermoid carcinomas (1, 5, 6, 7, 8). The resection of adjacent structures is indicated for cases with complications detected previously or during the surgery.
FINAL COMMENTSSuch tumors have different biological behavior according to the degree of histological differentiation, size of the lesion and presence of metastases; the early diagnosis and the correct management are key factors for prognosis.
In this case, the fast and aggressive growth of the lesion, the size of the tumor was critical for the patient's prognosis.
BIBLIOGRAPHICAL REFERENCES1. Ellis GL, Auclair PL, Gnepp DR. Surgical Pathology of the salivary glands. Major Problems in Pathology Series. Volume 25. Philadelphia: WB Saunders Company; 1991.
2. Ellis GL, Auclair PL. Tumors of the Salivary Glands. In: Armed Forces Institute of Pathology. Atlas of Tumor Pathology. 3rd Series, Fascicle 17. Washington; 1996.
3. Auclair PL, Goode RK, Ellis GL. Mucoepidermoid carcinoma of intraoral salivary glands. Cancer. 1992, 69:2021-30.
4. Cardoso WP, Denardin OV, Rapoport A, Araújo VC, Carvalho MB. Proliferating cell nuclear antigen expression in mucoepidermoid carcinoma of salivary glands. São Paulo Med J. 2000, 118:69-74.
5. Goode RK, Auclair PL, Ellis GL. Mucoepidermoid carcinoma of the major salivary glands: clinical and histopathologic analysis of 234 cases with evaluation of grading criteria. Cancer. 1998, 82:1217-24.
6. Brandwein MS, Ivanov K, Wallace DI, Hille JJ, Wang B, Fahmy A, Bodian C, Urken ML, Gnepp DR, Huvos A, Lumerman H, Mills SE. Mucoepidermoid carcinoma: a clinicopathologic study of 80 patients with special reference to histological grading. Am J Surg Pathol. 2001, 25:835-45.
7. Plambeck K, Friedrich RE, Bahlo M, Bartel-Friedrich S, Klapdor R. TNM staging, histopathological grading, and tumor-associated antigens in patients with a history of mucoepidermoid carcinoma of the salivary glands. Anticancer Res. 1999, 19:2397-404.
8. Spiro RH, Huvos AG, Berk R, Strong EW. Mucoepidermoid carcinoma of salivary gland origin: a clinicopathologic study of 367 cases. Am J Surg. 1978, 136:461-8.
9. Calderón-Garcidueñas L, Delgado R, Calderón- Garcidueñas A, Meneses A, Ruiz LM, Garza J, Acuna H, Villarreal- Calderón A, Raab-Traub N, Devlin R. Malignant neoplasms of the nasal cavity and paranasal sinuses: A series of 256 patients in México City and Monterrey. Is air pollution the missing link? Otolaryngol Head Neck Surg. Apr. 2000, 122:499-508.
1 Specialist in Otorhinolaryngology. Coordinator of the Medical Residence Service in Otorhinolaryngology from the Hospital São José do Avaí (HSJA).
2 Resident Student of Otorhinolaryngology of the HSJA (R3).
3 Resident Student of Otorhinolaryngology of the HSJA.
4 Trainee Doctor of the Otorhinolaryngology Service of the HSJA.
5 Trainee Student of the Otorhinolaryngology Service of the HSJA.
Institution: Hospital São José do Avaí. Itaperuna / RJ - Brazil. Mail address: Paulo Tinoco - Rua Coronel Luiz Ferraz, 397 - Centro - Itaperuna / RJ - Brazil - Zip code: 28300-000 - Telephone: (+55 22) 9251-5451 - E-mail: josecarlosop@hotmail.com
Article received on June 11, 2009. Approved on August 16, 2009.