INTRODUCTIONThe extramedullary plasmocytoma is a malignancy of the plasma cells, which together with the solitary plasmocytoma bone sum less than 10% of this condition located, which has multiple myeloma (MM) as the main diagnosis.
MM is the systemic form of the disease, and cancer is a B lymphocyte is characterized by proliferation of malignant plasma cells and production of monoclonal immunoglobulin. Its incidence among hematological malignancies ranges from 10 to 15%, with increased frequency in men by a ratio of 1.6:1, being more prevalent in the sixth decade of life. The extramedullary plasmocytoma (EMP), one of the localized forms, is a neoplastic proliferation of monoclonal plasma cells. In contradiction to other forms, the tumor may be confined to their place of origin in 80% to 90% are located in the head and neck, most commonly in the sub epithelial tissue of the upper aerodigestive tract. It is estimated incidence 4-5% in the nasal cavity, paranasal sinuses and nasopharynx (1.2).
The PEM of the larynx is a rare presentation of unknown etiology that accounts for 0.04 to 0.19% of malignant laryngeal neoplasias (3). The relationship between men and women is 3:1, primarily affecting patients over 50 years (4, 5, 6). and secondary symptoms are often local invasion of tumor mass (7), with only 10-20% with lymph node (2). Typically lesions are unique and independent, but may be the first evidence of multiple myeloma (6) and then progress 10-30% of the time for diagnosis (4).
The solitary bone plasmocytoma (PSO), otherwise located mainly affecting the pelvic and long bones of the extremities with solitary bone lesions and without spinal cord changes, the progression to the systemic form also occurs, but more frequently, up to 60% cases up to 10 years.
Given the rarity of this lesion we report a case of PEM of the larynx, taking into account its clinical, pathological and therapeutic.
CASE REPORTFemale patient, aged 49, teacher, referring to our service intermittent dysphonia a year ago with progressive worsening associated with vocal effort and vocal fatigue. During the physical examination Maximum phonation time of 16 seconds [s] = 18 seconds, unable to perform the [z]. It was showed slight harshness and breathiness of the voice. Endoscopy visualized lesion reddish edges smooth, polypoid in 1/3 of the left ventricular fold. It was programmed then the micro laryngeal surgery for excisional biopsy of the lesion with the primary diagnosis of ventricular fold granuloma.
Patient undergoing the procedure where the microscopic examination of the lesion damage was observed in red, well vascularized, from third average throat left ventricle, the consistency of soft tissue without significant infiltration (Figure 1). 0.5 x0 resected lesion, 7 cm with the help of CO2 laser material and sent for pathological examination.
Histological examination showed proliferation of plasma cells in nodular arrangements expanding the corium being suggestive of Plasmocytoma, later diagnosed immunophenotyping.
We then screened for Multiple myeloma with whole-body scintigraphy, urinary tests for Bence-Jones proteins, protein electrophoresis of blood and bone marrow biopsy which are all within normal limits.
The patient is outpatient treatment without signs of recurrence or progression of the disease a year ago.
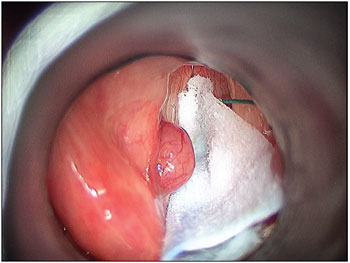
Figure 1. Microlaryngoscope - injury with an appearance of granuloma in 1/3 of the ventricular fold.
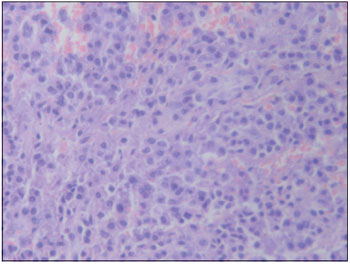
Figure 2. Histomicrograph (200X) - Proliferating plasma cells arranged in nodular expanding chorion.
The extramedullary plasmocytoma (EMP), with the solitary bone plasmocytoma is a localized presentation of plasma cell neoplasm, multiple myeloma that has as its main representative. Its incidence among these neoplasms is 4.5 to 7, with 2% to the head and neck as most common, making up 80% of cases. Laryngeal involvement is rare and the most common sites of presentation the epiglottis, vestibular fold, arytenoids, and subglotis, respectively (1.4). Most patients at diagnosis is between 50 and 70 years, but there are cases reported since the second decade of life (5). Its prevalence is higher in men by a ratio of 3:1, with no racial predilection (2).
The clinical presentation of PEM varies according to location: hoarseness, cough, dyspnea, stridor that these symptoms can last from months to years before their diagnosis (1). In our case, the patient attended a year of dysphonia due to vocal strain and fatigue before diagnosis, not presenting with cervical lymphadenopathy, which corroborates other publications (5,6,7).
In the larynx the PEM doesn't have a characteristic lesion may be polypoid or sessile. In our case, is presented as a mass in middle 1/3 of left vestibular fold, polypoid with a smooth surface and reddish like a granuloma. This presentation is the most common red, but can also be colored pink or yellow, are generally consistent with hyper vascular soft tissue and friable (3,5,8).
The microscopy shows diffuse monomorphic infiltrate in a fine reticular stroma with plasma cells with abundant cytoplasm, slightly basophilic and rich in organelles (2.9). Various forms of atypical cell can be found depending on the degree of cell differentiation, which is directly related to prognosis (2).
Diagnosis is confirmed histologically by the presence of monoclonal plasma cell proliferation. In the presence of difficulty to distinguish PEM from undifferentiated epithelial tumors should be performed immunophenotyping to differentiate monoclonal from polyclonal cells. Thus, one can show granulomas benign forms of plasma cells or other inflammatory processes have characteristics polyclonal (1,4,8).
As the PEM can be the first evidence of a neoplasm of plasma cells and progression to MM occurs in up to 30% of cases, after the initial diagnosis, we should perform thorough research on this. They are usually made: bone marrow biopsy, imaging tests to rule out lytic lesions, electrophoresis and immunoelectrophoresis of serum protein and urine test for Bence Jones proteins. The MRI is the test of choice to highlight the lytic lesions (8).
There are studies that suggest an association between laryngeal amyloidosis with extramedullary plasmocytoma. VELEZ et al in 2008 reported a case that was confirmed by histological examination of this correlation. In the literature review conducted by the author shows that the first report of correlation between these diseases happened in 2001 by Nagasaka et al. accordingly, in cases of laryngeal amyloidosis is important to research pathological process in lymphomatous laryngeal lesion (10). This association was not observed in our case.
The differential diagnosis includes plasma cell granuloma, pseudo lymphoma, undifferentiated carcinoma and metastases. The PEM has been differentiated from the benign form of plasma cell granuloma by immunophenotyping, in which this disease presents polyclonal chains and other inflammatory cells (1).
Due to the low incidence of PEM, there is still no consensus on optimal therapy. Radiation therapy is accepted as the standard treatment, even if not standardized dose and period, and no study showing the advantage over surgery alone (2.11). The non-mutilating surgery, especially in areas easily accessible to small and localized lesions, promotes the same benefit with less morbidity (3,8). In our case was chosen by the micro laryngeal surgery with CO2 laser and resection of the lesion, with subsequent "screanning" for MM. The patient keeps up with no signs of recurrence or disease progression.
Adjuvant chemotherapy may be used to prevent progression to MM, however, its role remains uncertain. Several studies suggest that chemotherapy increases the clearance of proteins M and reduces progression to MM, while others found no benefit (5).
The conversion of the PEM to MM ranges from 10 to 30%, significantly lower than the progression of the PSO. Kapadia et al (1982) and HOLLAND et al (1992) observed the progression to MM in their patients over a period of two years, suggesting this period as high risk. Most authors recommend a "follow-up" long since found cases of conversion to MM 15 years after diagnosis of localized disease (2).
The prognosis is related to the location of the tumor, cartilage and bone destruction, and regional lymph node involvement. Survival is higher in patients with localized disease than in those with MM, with a five-year survival of 18% in patients with MM and approximately 66% among those with PEM. (5). Patients who developed MM after the diagnosis of PEM have a longer survival than those who have MM as the initial diagnosis.
CONCLUSIONExtramedullary plasmocytoma should be considered in the differential diagnosis of rare tumors of the larynx. It is essential after the diagnosis of multiple myeloma research and a "follow up" appropriate given that their progression to the systemic form is well documented.
Radiotherapy is an effective therapy for PEM with high rates of local control and the surgery is an option for small and localized lesions, as described in our case.
REFERENCES1. Zbären P, Läng H, Beer K, Becker M. Plasma cell granuloma of the supraglottic larynx. J Laryngol Otol, 1995; 109(9):895-8.
2. Susnerwala SS, Shanks JH, Banerjee SS, Scarffe JH, Farrington WT, Slevin NJ. Extramedullary plasmocytoma of the head and neck region: clinicopathological correlation in 25 cases. Br J Cancer, 1997; 75(6):921-7.
3. Bjelkenkratz K, Lundgren J, Olofsson J. Extramedullary plasmocytoma of the larynx. J Otolaryngol, 1981; 10(1):28-34.
4. Pratibha CB, Sreenivas V, Babu MK, Rout P, Nayar RC. Plasmacytoma of Larynx - A Case Report. J. Voice, 2009; 23(6):735-8.
5. Gorenstein A, Bryan Neel H, Devine KD, Weiland LH. Solitary extramedullary plasmocytoma of the larynx. Arch Otolaryngol, 1977; 103(3):159-61.
6. Maniglia AJ, Xue JW. Plasmocytoma of the larynx. Laryngoscope, 1983; 93(6):741-744.
7. Nakashima T, Matsuda K, Haruta A. Extramedullary plasmocytoma of the larynx. Auris Auris Nasus Larynx, 2006; 33(2):219-22.
8. Hotz MA, Bosq J, Schwaab G, Munck J. Extramedullary solitary plasmocytoma of the head and neck. Ann Otol Rhinol Laryngol, 1999; 108(5):495-500.
9. Jyothirmayi R, Gangadharan VP, Nair MK, Rajan B. Radiotherapy in the treatment of solitary plasmocytoma. Br J Radiol, 1997; 70(833):511-6.
10. Velez D, Hinojar-Gutierrez Z, Nam-Cha S, Acevedo-Barbera 2007 A. Laryngeal Plasmacytoma presenting as amyloid tumour: a case report. Eur Arch Otorhinolaryngol, 2007; 264(8):959-61.
11. Creach KM, Foote RL, Neben-Wittich MA, Kyle RA. Radiotherapy for extramedullary plasmocytoma of the head and neck. Int J Radiat Oncol Biol Phys, 2009; 73(3):789-94.
1) President of the Brazilian Society of Laryngology and Voice (2001-2003). Director of the Center for Otolaryngology and Head and Neck Surgery of São Paulo.
2) Resident Doctor of the Center for Otolaryngology and Head and Neck Surgery of São Paulo.
3) Otolaryngologist.
Institution: Center for Otolaryngology and Head and Neck Surgery of St. Paul. Sao Paulo / SP - Brazil. Address correspondence to: José Antonio Pinto - Alameda Nhambiquaras of 159 - Sao Paulo / SP - Brazil - CEP: 04090-010 - E-mail: japorl@uol.com.br
Manuscript received June 8, 2010. Article accepted on August 1, 2010.