INTRODUCTIONThe growth in the aging population and increased longevity associated with lifestyle changes affected the patterns of morbidity and mortality. Advancing age increases the risk for a number of chronic diseases, and dizziness and hypertension (systemic arterial hypertension; SAH) have become highly prevalent among the elderly.
Dizziness is the illusion of movement of the individual or his or her surrounding environment. This symptom can be caused by dysfunction of any segment of the systems related to body balance. Dizziness with a rotational character is called vertigo (1). These symptoms are highly prevalent worldwide, affecting approximately 2% of young adults, 30% of seniors at age 65, and up to 50% of individuals over 85 years of age. Dizziness originates in the vestibular system in 85% of cases, with the remainder stemming from ocular, neurological, psychiatric, metabolic, and cardiovascular problems (2).
The dizzy patient usually reports difficulty in mental concentration, memory loss, fatigue, and falling. The physical insecurity generated by dizziness and imbalance can lead to irritability, loss of confidence, fear of going out alone, anxiety, depression, or panic and can change the routine of life and affect family, social, and professional relationships, in turn causing loss of confidence, concentration, and income (1). Dizziness interferes with the individual's quality of life (QOL) and can restrict certain movements of the head and body, thus impeding his or her professional, domestic, social and/or leisure activities (3).
Dizziness is a major cause of falls in the elderly. The Unified Health System (SUS) in Brazil has increased spending on treatment of fractures in older people each year, and as of October 2009 R$57.61 million had been spent on hospitalizations (4).
Tinetti (5) reports that falls are the cause of approximately 10% of emergency hospital admissions and 6% of urgent care visits and are associated with restricted mobility, a decline in the ability to perform daily activities, and an increase in the risk for institutionalization.
Hypertension is a chronic disease of multifactorial origin that is highly prevalent in Brazil and constitutes a serious risk factor for the development of cerebrovascular and heart diseases (6). High blood pressure and dizziness are often associated because a person with uncontrolled hypertension may present with dizziness; indeed, dizziness may be the only symptom of hypertension.
High blood pressure affects approximately 50% of the population over 60 years of age, accounting for 80% of cases of stroke, 60% of cases of acute myocardial infarction, and 40% of early retirements and a mean cost of R$475 million for the 1.1 million admissions per year (7, 8).
The objective of this study was to assess the association between dizziness and hypertension in elderly residents, including men and women, of the 5 different regions of the city of Londrina.
METHODS We conducted a historical cross-sectional cohort study in a community of non-institutionalized elderly people in the city of Londrina, Paraná, who were participants in the Study of Aging and Longevity. The inclusion criteria were age over 60, either sex, independent living, a Functional Status level as proposed by Spirduso (9) of 3 or 4, and voluntary informed consent to participate in the study (indicated by freely signing the consent form). We excluded elderly subjects with cognitive problems who did not reach the minimum score on the Mini Mental State Examination (MMSE) (the cutoff score was 19 for the illiterate and 25 for the literate, after the study of Lourenço and Veras (10)), older adults with uncorrected hearing problems, and anyone who did not wish to participate in the research.
The study population consisted of 43,610 seniors enrolled in 38 Basic Health Units (BHUs) of the urban area of Londrina. The required sample size was calculated to be 343 individuals. The sample was increased to 493 individuals over 60 years of age to allow for the degree of sample loss typical of studies of the elderly. The sample was chosen randomly but with consideration for the socioeconomic differences among the 5 regions of the city (north, south, central, east and west). A sampling error of 5% was assumed for the sample size calculations.
The data collection questionnaire was devised by the authors themselves to address socio-demographic factors (such as age, gender, etc.) and self-reported diagnosis of hypertension by a doctor and episodes of dizziness in the past 3 years. No participant's blood pressure was measured, and no other precision instrument was used; only oral reports were considered. This study was approved by the Ethics Committee in Research of Universidade Norte do Paraná (UNOPAR), protocol number 0070/09.
The statistical analysis included descriptive analysis of categorical variables and chi-square analysis with a significance level of p < 0.05 to examine the possible associations between dizziness and hypertension and between both dizziness and hypertension and gender. The statistical program SPSS15.0 was used.
RESULTS The study included 493 individuals aged 60 to 97 years (median, 69 years; first quartile, 64 years; third quartile, 74 years), of whom 330 (66.9%) were women (Figure 1).
Among all of the elderly subjects, 257 (52.1%) complained of dizziness, of whom 76.3% were women, and 308 (62.5%) subjects reported a diagnosis of hypertension, of whom 66.9% were women and 33.1% men.
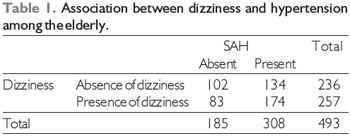
The chi-square analysis of the relationship between hypertension and dizziness resulted in a
X2 value of 6.26 with an associated probability (p value) of 0.01 for 1 degree of freedom, showing that such a relationship is unlikely to appear only as a result of sampling error (random) (Table 1).
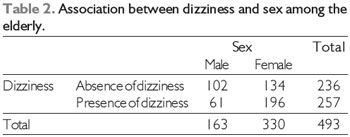
Analysis of the relationship between dizziness and gender showed an association between female sex and dizziness (
X2 = 21.10, p < 0.001; Table 2). There was also an association between female sex and a diagnosis of hypertension (
X2 = 5.47, p = 0.02, 1 degree of freedom; Table 3).
Chi-square test (
X2 = 6.26; p = 0.01).
SAH: systemic arterial hypertension
Chi-square test (
X2 = 21.10; p < 0.001).
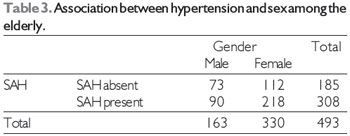
Chi-square test (
X2 = 5.47; p = 0.02).
Sensory changes, decreases in visual acuity, and impairment of proprioception and the vestibular system reduce environmental stimuli and leave individuals more susceptible to falling, requiring a multifaceted approach to reducing the risk of such falls. Integrated actions and specialized care are used to monitor the population at greatest risk and encourage them to take preventive measures to minimize the risk for future falls (11, 12).
Of the 257 subjects with dizziness, 76.3% were women. This gender distribution agrees with studies that have shown that women are susceptible to dizziness, possibly due to hormonal changes, and also with the fact that women more often seek out health services (13,14).
The present study examined only people over 60 years of age and found a prevalence of dizziness of 52.1%. Dizziness has been considered a geriatric syndrome, a multifactorial health condition resulting from the cumulative effects of deficits in multiple systems that make the elderly more vulnerable to situational challenges. Aging causes loss of balance and changes in muscle and bone mass (15).
Falls and their consequences for the elderly have assumed epidemic dimensions in Brazil. The costs for the elderly person who falls and sustains a fracture are incalculable; worse, the entire family is affected when the elderly person with a fracture requires hospitalization and/or surgical treatment. The costs to the health system are also high (4).
In summary, dizziness can cause physical, functional, and emotional changes in older people and may result in other health problems such as falls and fractures. Therefore, both prevention and treatment are suggested for improving the quality of life of these individuals.
Pharmacological treatment for dizziness should be used with caution and only for a short period of time due to its interference with the natural compensation of the central nervous system (CNS). When such treatment is appropriate, as for cases of vertigo lasting more than a few days, it must be withdrawn gradually over the course of a few days (16). It is important to remember that the elderly more often have comorbidities and hence use multiple medications, the interactions among which can cause undesirable effects such as dizziness. Therefore, a detailed history including all medications used is an important part of the diagnostic work-up of elderly patients with dizziness.
Hypertension in the elderly requires constant use of medication and can also cause dizziness. A study of therapeutic intervention in patients with hypertension conducted in 49 individuals by the Reference Center for Social Work in Fortaleza found that although over 50% of the participants employed only non-pharmacological treatment modalities such as diet and exercise, 49% reported adverse reactions Of these, the most frequently cited were polyuria and dizziness (29% each) (17).
Dizziness can sometimes be a symptom of hypertensive crisis. According to FEITOSA-FILHO (18), the hypertensive crisis is a clinical condition characterized by a sudden increase in blood pressure (to >180/120 mmHg) accompanied by symptoms that may be mild (headache, dizziness, and tinnitus) or severe (dyspnea, chest pain, coma, and even death) with or without acute lesion of a target organ. Therefore, dizziness may be the first warning sign to direct the patient or clinician to investigate the possibility of hypertension.
Benign paroxysmal positional vertigo (BPPV) was reported to affect 36.7% of an elderly population with peripheral vestibular disorders and account for 33% of the complaints of dizziness in primary care (19). SCZEPANEK et al. (20) confirmed BPPV to be the most frequently underdiagnosed cause of dizziness in the elderly in primary care. Therefore, primary care providers should give more attention to common vestibular disorders.
Dizziness may affect the QOL of the elderly. The "Dizziness Handicap Inventory" (DHI) was developed to measure the self-perceived levels of physical, functional, and emotional handicap associated with dizziness. These symptoms can generate frustration, fear of going out alone or staying home alone, worry about self-image, disturbed concentration, feelings of failure, changes in family or social relationships, and depression (21, 22).
The prevalence of hypertension in the elderly is higher than 60% and is becoming the determining factor in morbidity and mortality in this population, thus requiring proper identification of the problem and appropriate therapeutic approaches (23).
A study carried out using the data from the Health, Welfare, and Aging in Latin America and the Caribbean Project (SABE) from 1769 elderly individuals in São Paulo found that this population was predominantly female (58.8%) and that hypertension was the most common chronic condition (53.4%) (24).
In our survey, 62.5% of participants reported hypertension; of these, 66.9% were women and 33.1% men. In a cross-sectional study with a randomized sample of 892 people representing the adult population of the city of Campo Grande, MS, Souza et al. (25) found that the prevalence of hypertension was 41.4% overall, 51.8% in men and 33.1% in women. Of the 370 subjects with hypertension, only 69.18% were aware of their disease (p < 0.001). It should be kept in mind that hypertension was self-reported in our study, so it is highly probable that the number of hypertensive individuals was greater than reported.
A study of the 110,489 inhabitants of the city of Catanduva in São Paulo using a random sample of 688 adults (>18 years old), 286 men and 402 women, found a 31.5% prevalence of hypertension. The prevalence in men was 33.9%, ranging from 9% in the 18-29-year-old group to 44% among those aged 70-99 years (26).
Alves et al. (24) demonstrated in their study that chronic diseases strongly influence the functional capacity of the elderly. The presence of hypertension increased the probability that an elderly person would be dependent in instrumental activities of daily living by 39%.
Hypertension (HBP) is a major circulatory disease that can affect the peripheral and/or central auditory and vestibular systems. Many studies in the elderly have addressed the association between hypertension and dizziness and/or vertigo. One study comparing the frequency of vertigo in elderly patients with and without hypertension in 238 subjects found that 23.8% of hypertensive patients reported vertigo whereas 16% of non-hypertensive subjects reported dizziness, but there was no significant association (27).
The use of only self-reported information about the presence of hypertension is a limitation of our study. According to Zaitune et al. (28), morbidity information helps to identify individuals who have been diagnosed at least once in their lifetimes but omits those unaware of their hypertension and can thus underestimate prevalence. However, other studies have found that the prevalence of hypertension self-reported during an interview proved to be a valid estimate of the prevalence of hypertension in the population.
Hypertension is one of the most common diseases in the elderly and places enormous demands on the health system. Dizziness is the most frequent cause of falls in the elderly, which affects the quality of life in this population as well as imposing exorbitant costs arising from fractures. It is important to pay more attention to these conditions and to implement preventive measures and develop health promotion programs for the primary care setting.
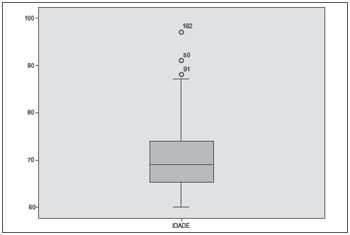
Figure 1. Age distribution of the sample.
Our data show a significant association between dizziness and hypertension as well as high prevalence rates of both hypertension and dizziness in this elderly population.
In addition to avoiding the overuse of medications and maintaining adequate control of blood pressure, special care should be taken in the differential diagnosis of dizziness associated with benign paroxysmal positional vertigo and other disorders in order to avoid dizziness and other symptoms that can lead to falls and other harm to seniors.
REFERENCES1. Cabral GTR, Correia LB, Silveira SR, Lopes RP. Interferência da queixa de tontura na qualidade de vida dos idosos cadastrados na UBS do bairro Araçás, Vila Velha/ES. ACTA ORL. 2009;27(2):58-63.
2. MaarsinghOR, Dros J, Schellevis FG, van Weert HC, Bindels PJ, van der Horst HE. Dizziness reported by elderly patients in family practice: prevalence, incidence, and clinical characteristics. BMC Fam Pract. 2010;1(11):11-2.
3. Takano NA, Cavalli SS, Ganança MM, Caovilla HH, Santos MAO, Peluso ETP, et al. Qualidade de vida de idosos com tontura. Braz J Otorhinolaryngol. 2010;76(6):769-75.
4. Brasil. Ministério da Saúde Brasil. Quedas de idosos: SUS gasta quase R$ 81 milhões com fraturas em idosos em 2009 [Internet]. [cited 2011 jul 2]. Available from: http://portal.saude.gov.br/portal/sau de/visualizar_texto.cfm?idtxt=33674&janela=1
5. Tinetti ME. Preventing falls in enderly persons. N. Engl. J. Med. 2003;3(348):42-9.
6. Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Nefrologia. 5ª Diretrizes Brasileiras de Hipertensão Arterial. São Paulo; 2006.
7. Brasil. Ministério da Saúde. Relatório técnico da campanha nacional de detecção de suspeitos de diabetes mellitus. Brasília: Secretaria de Políticas da Saúde, Ministério da Saúde; 2001.
8. Oliveira TC, Araujo TL, Melo EM, Almeida DT. Avaliação do processo adaptativo de um idoso portador de hipertensão arterial. Rev. Lat Am. Enfermagem. 2002;10(4):530-6.
9. Spirduso WW. Dimensões físicas do envelhecimento. 1st ed. Barueri-SP: Manole; 2005. p. 168-199.
10. Lourenço RA, Veras RP. Mini-Exame do Estado Mental: características psicométricas em idosos ambulatoriais. Ver Saúde Pública. 2006;4(4):712-9.
11. Paixão JR, Heckmann MF. Distúrbios da postura, marcha e quedas. In: Freitas EV, et al. Tratado de Geriatria e Gerontologia. 2nd ed. Rio de Janeiro: Guanabara Koogan; 2006. p. 950-60.
12. Aguiar CF, Assis M. Perfil de mulheres idosas segundo a ocorrência de quedas: estudo de demanda no Núcleo de Atenção ao Idoso da UnATI/UERJ. Rev Bras Geriatr Gerontol. 2009;12(3):391-404.
13. Tanaka OU, Ribeiro EL. Ações de saúde mental na atenção básica: caminho para ampliação da integralidade da atenção. Cien Saude Colet. 2009;14(2):477-86.
14. Koga KA, Resende BDA, Mor R. Estudo da prevalência de tonturas/vertigens e das alterações vestibulares relacionadas à mudança de posição de cabeça por meio da vectoeletronistagmografia computadorizada. Rev CEFAC. 2004;6(2):197-202.
15. Siqueira FV, Facchini LA, Piccini RX, Tomasi E, Thumé E, Silveira DS, et al. Prevalência de quedas em idosos e fatores associados. Rev Saude Publica. 2007:41(5):749-56.
16. Bertol E, Rodriguez CA. Da tontura a vertigem: uma proposta para o manejo do paciente vertiginoso na atenção primária. Rev APS. 2008;11(1):62-73.
17. Vitor AF, et al. Perfil das condições de seguimento terapêutico em portadores de hipertensão arterial. Esc. Anna Nery. 2011;15(2):251-60.
18. Feitosa-Filho GS, Lopes RD, Poppi NT, Guimarães HP. Emergências hipertensivas. Rev. bras. ter. intensiva. 2008;20(3):305-12.
19. Neuhauser HK, Radtke A, von Brevern M, Lezius F, Feldmann M, Lempert T. Burden of Dizziness and vertigo in the community. Arch Intern Med. 2008;168(19):2118-24.
20. Sczepanek J, Wiese B, HummersPradier E, Kruschinski C. Newly diagnosed incident dizziness of older patients: a followup study in primary care. BMC Fam Pract. 2011;12(58):1-8.
21. Pereira AB, Santos JN, Volpe FM. Effect of Epley's maneuver on the quality of life of paroxismal positional benign vertigo patients. Braz J Otorhinolaryngol. 2010;76(6):704-8.
22. Santos EM, Gazzola JM, Ganança CF, Caovilla HH, Ganança FF. Impacto da tontura na qualidade de vida de idosos com vestibulopatia crônica. Pro Fono. 2010;22(4):427-32.
23. Brandão AP, Brandão AA, Freitas EV, Magalhães MEC, Pozzan R. Hipertensão arterial no idoso. In: Freitas EV, et al. Tratado de geriatria e gerontologia. Rio de Janeiro: Guanabara Koogan; 2006. p. 459-73.
24. Alves LC, Leimann BCQ, Vasconcelos MEL, Carvalho MS, Vasconcelos AGG, Fonseca TCO, et al. A influência das doenças crônicas na capacidade funcional dos idosos do Município de São Paulo, Brasil. Cad Saude Publica. 2007;23(8):1924-30.
25. Souza ARA, Costa A, Nakamura D, Mocheti LN, Stevanato Filho PR, Ovando LA. Um Estudo sobre Hipertensão Arterial Sistêmica na Cidade de Campo Grande, MS. Arq Bras Cardiol. 2007;88(4):441-6.
26. Instituto Brasileiro de Geografia e Estatística [Internet]. Rio de Janeiro: IGBE; 2004. [cited 2011 Aug 10]. Available from: http://www.ibge.gov.br.
27. Marchiori LLM, Melo JJ, Possette FLF, Correa AL. Comparação da Frequência de Queixa de Vertigem no Idoso Com e Sem Hipertensão Arterial. Arq. Int. Otorrinolaringol. 2010;14(4):456-60.
28. Zaitune MPA, Barros MBA, César CLG, Carandina L, Goldbaum M. Hipertensão arterial em idosos: prevalência, fatores associados e práticas de controle no Município de Campinas, São Paulo, Brasil. Cad Saude Publica. 2006;22(2):285-94.
1) Student in the Master's Program in Rehabilitation Sciences associated with Universidade Estadual Londrina (UEL)/Universidade Norte do Paraná (UNOPAR), Londrina, Parana. Union of America Faculty Professor, Foz do Iguacu, Parana.
2) Student in the Master's Program in Rehabilitation Sciences associated with UEL/UNOPAR, Londrina, Parana. Physiotherapist admitted after a public examination by the Family Health Program.
3) Doctor of Medicine and Health Sciences, University of Londrina. Professor in the Master's Program in Rehabilitation Sciences associated with UEL/UNOPAR, Londrina, Paraná.
4) Doctor of Medicine and Health Sciences, University of Londrina. Professor in the Master's Program in Rehabilitation Sciences associated with UEL/UNOPAR, Londrina, Paraná.
Institution: Universidade Estadual de Londrina. Londrina / PR - Brazil. Mailing address: Anália Rosário Lopes - Rua da Cosmoética, 1847 - Bairro: Tamanduazinho / Foz do Iguaçu / PR - Brazil - Zip code: 85853-755 - E-mail: analialopes80@gmail.com
Article received on April 9, 2012. Article accepted on November 8, 2012.