INTRODUCTIONThe frontal sinus are typically pair, asymmetric, separated by a central intersinusal septum and with different degrees of pneumatization. In adults the average dimensions are 24.3 mm high, 29 mm large and 20.5 deep. Around 10 to 12% of normal adults may present a rudimentar frontal sinus (FS) or even a complete lack of frontal bone pneumatization in one of two sides. Around 4% of the asymptomatic population may present bilateral frontal sinus agenesis (1). Gaafar e col.2 reported that the average diameter of the frontal sinus ostium has been 5.6 mm, varying from 4 to 7 mm.
The frontal sinus drain via is made of three different regions and usually presents a sandglass shape. The sandglass upper part is represented by the frontal sinus itself, while the narrower part is this sinus ostium. The sandglass lower part is made of the frontal recess (FR), a space which depends on the variable development of anterior pneumatized cells. (1,3,4,5).
Among the anterior ethmoid cells, two of them make the left and right frontal sinus. The remaining ethmoid cells compete for the available space and some of them may eventually expand on the frontal bone, while others remain with small dimensions. (6)
Accessory cell classification in the FS and in the RF have been a source of divergence in the literature for around one century. For this discussion, the accessory cells on the FS and in the FR regions are classified into three main categories: bulla frontalis; supra-orbitary cells and septal inter-sinus cells. In the presence of front-ethmoid cells, the surgeon may face, during the endoscopic surgery, multiple openings in the FR, which consequently makes the FS ostium recognition difficult. (7)
The objective of the present corpse endoscopic dissection study has been to identify and to describe the topographic inter-relation of frontal sinus ostium with the frontal-ethmoid cell otiums which are present in the frontal recess.
CASUISTICS AND METHODAfter approval of Ethics Committee for Research Project Analysis (CAPPesq - protocol number 414/02), 32 corpses from the SVO (Obit Verification Service) have been studied (59 nasal fosses), and 22 of them (68.75%) were men and 10 of them (31.25%) were women. They aged from 20 to 88 years old, average of 63 and standard deviation of 14.29 years old.
The following exclusion criteria have been used in this study: less than 20 years old; bilateral frontal sinus agenesis; previous history of nasal trauma; nasossinus surgery background; nasossinus affections which changed the local anatomy (ex: nasal polyposis and tumors).
The video-documentation system used in this study has been made of a halogen light source (Komlux-HL2250); a micro-camera (Toshiba/IK-CU43A); a screen (Radioschack TV/VCR Combo 16-420); and a digital camcorder (Sony DCR-TR7000). This system provided the documentation of all cases through dissection digital recording.
The surgical instrument used during the dissections have consisted of: 10mm chisel and a hammer (Factory Instrumental Cirúrgico); 4mm 0° rigid endoscope Karl Storz (Hopkins II Telescope - 7210 AA); 4mm 45° rigid endoscope Karl Storz (Hopkins II Telescope - 7210 FA); a Cottle clamp (Factory Instrumental Cirúrgico); a non-sharp straight clamp (456001 B Rinoforce Blakesley Nasal Fórceps/Storz); a sharp straight clamp (451000 B Rinoforce Blakesley Nasal Fórceps/Storz); 55° angled curette (628712 Kuhn-Bolger Frontal Sinus Curette/Storz); a latero-lateral opening giraffe clamp (651020 Rinoforce Stammberger Fórceps/Storz) and a anterior-posterior opening giraffe clamp (651010 Rinoforce Stammberger Fórceps/Storz).
All corpses already had a coronal incision behind the hair implantation line made by the on-call SVO employee, once such procedure is part of this institution exam protocol. After the coronal incision, the dissections have been made only by the executor researcher and followed the following procedures:
External Access
1. Subperiosteal abruption (Picture 1) of the fronto-orbitary anterior flap until the complete exposition of frontal bone board and bilaterally superior orbitary ridge visualization;
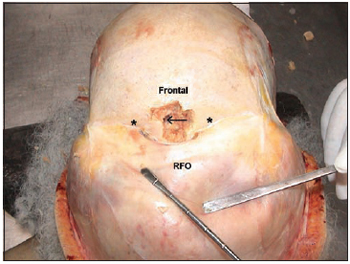
Picture 1. Picture taken during dissection showing the fronto-orbitary anterior flap subperiosteal abruption and the osteotomy in a frontal sinus agenesis case. The arrow indicates the presence of encephalic tissue (* = orbitary ridge; RFO = fronto-orbitary flap).
2. Osteotomy (Pictute 1) of immediately above and medium frontal bone board around the upper orbitary ridge, using chisel and hammer;
Endonasal Access
3. FS ostium cateterization under direct view, through the external access, with a flexible plastic probe;
4. Incision and exeresis of uncinate process (UP) and of other ethmoid cells until the identification of flexible plastic probe in the FR cateterizing the frontal sinus ostium (Picture 2A and 2B);
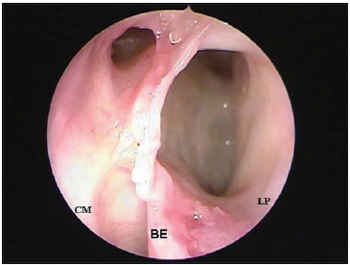
Picture 2A. Left nasal fossa endoscopy (45 degrees 4 mm rigid endoscope) making the presence of two ostiums in the frontal recess evident, making the frontal sinus ostium recognition difficult (CM = medium shell; BE = ethmoid bubble; LP = papyraceous lamina).
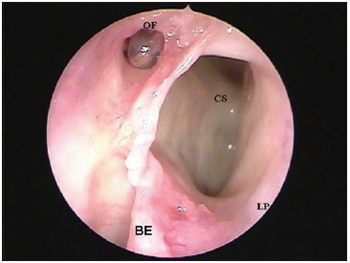
Picture 2B. Left nasal fossa endoscopy (45 degrees 4 mm rigid endoscope) making the presence of a supra-orbitary cell evident, located laterally to the fostium of frontal sinus, cateterized by flexible plastic probe (CS = supra-orbitary cell; LP = papyraceous lamina; OF = ostium of frontal sinus).
5. Fronto-ethmoid ostium cells reserach in the FR and their localization in relation to FS ostium by using 4mm 45º rigid endoscope.
RESULTSOut of the 32 dissected corpses, five of them (15.63%) presented FS unilateral agenesis. Consequently, the evaluation of the present study has been performed in 59 nasal fossas.
Among the 59 dissected nasal fossas, 16 (27,12%) presented ostium of fronto-ethmoid cells in the frontal recess. Out of those 16 nasal fossas, 15 (25.42%) presented 1 (one) ostium of fronto-ethmoid cell, while only one nasal fossa (1.7%) presented two ostiums of fronto-ethmoid cells, adding up to 17 ostiums (Table 1).
Out of the 15 nasal fossas which presented 1 ostium of fronto-ethmoid cell, it has been observed that in 12 (20.34%) nasal fossas such ostium was originated in a supra-orbitrary cell (Pictures 2A and 2B), while in two nasal fossas (3.39%) the origin was in a bulla frontalis (Picture 3) and in one (1.7%) the origin was in a intersinus septal cell (Pictures 4A and 4B). In the only nasal fossa which presented two ostium of fronto-ethmoid cells, the existence of a supra-orbitary cell and of a bulla frontallis (Table 1) has become evident.
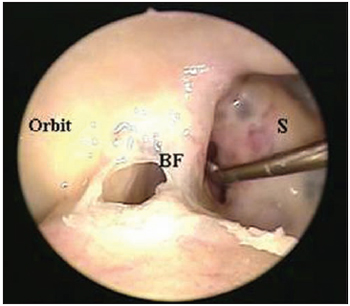
Picture 3. External visualization (with 0 degrees 4 mm rigid endoscope) of left frontal sinus making the presence of a bulla frontalis evident, located laterally to the ostium of frontal sinus identified by Cottle clamp (BF = bulla frontalis; S = intersinus septum).

Picture 4A. External visualization (with 0 degree 4 mm rigid endoscope) of left frontal sinus making a bulging in the intersinus septum region evident due to an intersinus septum (CSI - intersinus septal cell; OF = ostium of frontal sinus; S = intersinus septum).
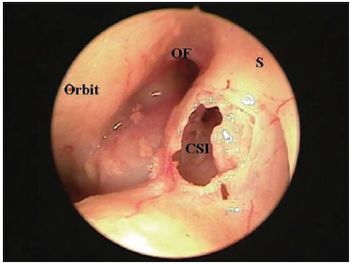
Picture 4B. External visualization (with 0 degree 4 mm rigid endoscope) of left frontal sinus making the presence of an intersinus septum cell evident (CSI - intersinus septal cell; OF = ostium of frontal sinus; S = intersinus septum).
The FS ostium localization in relation to ostium of fronto-ethmoid cells may be observed in Picture 5. Out of 17 ostium of fronto-ethmoid cells studied, 10 presented posterior drain to frontal sinus otium, while seven ostiums presented drain exactly next to frontal sinus ostium, that is, not being able to be classified as anterior os posterior. In relation to those 17 ostium localization, 11 of them presented lateral drain when compared to frontal sinus ostium, 2 of them presented medium drain and in four cases such drain was performed right posteriorly to the frontal sinus ostium at the same axis, that is, not being able to be classified as lateral or medium.
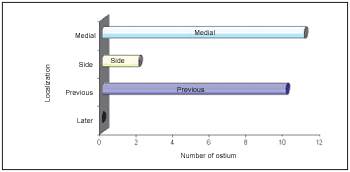
Picture 5. Distribution of frontal sinus ostium localization in relation to frontal-ethmoid cells ostium in the Frontal Recess.
Our knowledge about nasofrontal anatomy was, until recently, originated from anatomic studies made during the first half of last century, before the nasosinus endoscopic surgery (8,9,10). Such studies were based on corpses dissections and were responsible for valueble and detailed anatomy description which brought a solid base for nasosinus surgery development. However, the nasofrontal region fragile structure remained unknown for most of otorrhinolaryngologists and even for some experienced rhinologists surgeons. With the nasosinus endoscopic surgery sophistication and development, the idea that the antique literature anatomic description was not enough for advanced nasosinus endoscopic surgery has become common (11).
The supra-orbitary cell is an ethmoid cell which pneumatizes the orbitary ceiling of frontal bone posteriorly to FR and laterally to FS(12). The pneumatization degree may be 44 mm wide (measured from the medium line) for anterior cells (in the anterior 2/3 of orbit) and 16 mm for posterior cells (13). Such cells have already received several denominations: supra-orbital recess; supranumerary frontal sinus; fronto-orbital cell (14). During the nasosinus endoscopic surgery such cells' detection may be difficult and an accurate evaluation of a paranasal sinus computer tomography is essencial so that there will be no confusion with the FS (7).
The supra-orbitary cell has been the most frequent fronto-ethmoid cell in our study, found in 13 (22.03%) out of 59 evaluated nasal fossas. Our results in relation to the presence of supra-orbitary cells have been similar to Jovanovic's (15) (1961) and to Meloni and col. (1992), who reported 21% and 18% cases respectively.
According to Seiden & Stankiewicz16 (1998), the supra-orbitary ethmoid cell may shrink the FS ostium. However, the fact that its ostium may be easily confused with the FS ostium may be the most important one. It is not incommon to confuse a big supra-orbitary cell with the FS. We agree with those authors when they state that the supra-orbitary ethmoid cell usually presents its ostium more postrior and lateral in relation to the FS, once out of the 13 supra-orbitary cells presented in our sample, only one had its ostium more medium in relation to FS ostium, while none of them had anterior opening.
Bulla frontalis are anterior ethmoid cells which invade the frontal bone and grow in direction to the FS bulging its floor, not having connection to this sinus. Depending on its dimensions and pneumatization, such cells may change the FS draining system, which represents a real challenge for the diagnosis and even more to the surgical treatment of inflammatory diseases involving such sinus (4,5,17). In a similar way to the one reported by Dixon17 (1958) who observed the presence of bulla frontalis in around 8% of the cases, in this study we have made such cell evident in three nasal fossas (5.08%) among the 59 dissected ones. In relation to our three cases, the FS ostium localization has been more medium and anterior in relation to bulla frontalis ostium. When we analyse those three cases, we firmly agree with Stammberger5 (1999) when he states that in some cases it may be impossible to determine which cell represents the real FS and which corresponds to bulla frontalis.
The intersinusal septal cell is a medium line cell which pneumatizes the frontal bone between two frontal sinus (12). When there is intersinus septum deviation narrowing the frontal sinus ostium, the presence of a pneumatized cell in the lower part of such intersinus septum must be suspected (18). Such cell has been made evident in one among the 59 nasal fossas dissected in our study, which is diffrent from Van Alyea's19 (1941) results, who observed the presence of intersinus septal cells in 28 samples out of the 242 evaluated ones. One important factor to be pointed out is that in the presence of an intersinus septal cell, the FS ostium is not the most medium one anymore and becomes the most lateral one. Unfortunately, during the endospic surgical procedure and facing the circunstances, the probe cataterizing the FS ostium has not been available in this study for its accurate identification. However, the image examinations, mainly the paranasal sinus computer tomography, may readly determine the presence of such intersinus septal cells in the pre-operatory phase, as well as of other fronto-ethmoid cells, thus helping the correct identification of anatomic structures during the surgery.
Only in two situations, the FS ostium presented lateral localization in relation to the ostium of fronto-ethmoid cells, while the FS ostium has not been observed in posterior position in any of the cases (Picture 5). Such observation seems very important to us from the practical point of view, once in case of doubt and before two ostiums in the FR, the surgeon must first consider the most anterior and medium ostium as being the real FS ostium.
CONCLUSIONThe presence of fronto-ethmoid cells (bulla frontalis; supra-orbitary cells and intersinus septal cells) makes endonasal recognition of real ostium of frontal sinus difficult due to multiple openings found in the frontal recess, usually being the ostium of frontal sinus more anterior and medium in relation to the ostiums of those other cells.
BIBLIOGRAPHY1. McLaughlin RB, Rehl RM, Lanza DC. Clinically relevant frontal sinus anatomy and physiology. Otolaryngologic Clinics of North America 2001, 34(1):1-22.
2. Gaafar H, Abdel-Monem MH, Qawas MK. Frontal sinus outflow tract "anatomic study". Acta Otolaryngol 2001; 121:305-309.
3. Messerklinger W. Uber den Recessus frontalis und seine klinik. Laryngol Rhinol Otol. 1982; 61:217-23.
4. Stammberger H. Functional Endoscopic Sinus Surgery - The Messerklinger Technique. 1a ed. Philadelphia: BC Decker; 1991.
5. Stammberger, H. "UNCAPPING THE EGG"-The Endoscopic Approach to Frontal Recess and Sinuses. 1a ed. Tuttlingen: Endo-Press; 1999.
6. Navarro JAC. Cavidade do nariz e seios paranasais. 1a ed. Bauru: All Dent;1997.
7. Owen RG, Kuhn FA. Supraorbital ethmoid cell. Otolaryngol. Head Neck Surg. 1997, 116:254-61.
8. Kasper KA. Nasofrontal connections: a study of one hundred consecutive dissections. Arch. Otol. 1936, 23:322-43.
9. Schaeffer JP. The genesis, development and adult anatomy of the nasofrontal region in man. Am. J. Anat. 1916, 20:125-46.
10. Van Alyea OE. Frontal sinus drainage. Ann. Otol. Rhinol. Laryngol. 1946, 55:267-77.
11. Landsberg R, Friedman M. - A computer-assisted anatomical study of the nasofrontal region. Laryngoscope 2001, 111:2125-30.
12. Bent JP,Cuilty-Silver CC, Kunh FA. The frontal cell as a cause of frontal sinus obstruction. Am. J. Rhinol. 1994, 8:185-91.
13. Lang J. Clinical anatomy of the nose, nasal cavity & paranasal sinusis. New York: G Thieme Verlag; 1989.
14. Meloni F, Mini R, Rovasio S, Stomeo F, Teatani GP.Anatomic variations of surgical importance in ethmoid labyrinth and sphenoid sinus. A study of radiological anatomy. Surg. Radiol. Anat. 1992, 14:65-70.
15. Jovanovic S. Supernumerary frontal sinuses on the roof of the orbit: their clinical significance. Acta. Anat. 1961, 45:133-42.
16. Seiden AM, Stankiewicz JÁ. Frontal sinus surgey: the state of the art. Am. J. Otolaryngol. 1998, 19:183-93.
17. Dixon FW. The clinical significance of the anatomical arrangement of the paranasal sinuses. Ann. Otol. Rhinol.Laryngol. 1958, 67:736-41.
18. Lawson W. Frontal sinus. In: Blitzer A, Lawson W, Friedman WH. Surgery of the paranasal sinuses. Philadelphia: WB Saunders; 1985. pp.120.
19. Van Alyea OE. Frontal cells. An anatomic study of these cells with considerations of their clinical significance. Arch. Otolaryngol. 1941, 31:11-23.
1. Doctor of Science by the Faculty of Medicine of the USP (Research Associate Services of Otolaryngology and Immunology of HUPES - UFBA).
2. Doutorando Discipline of Otolaryngology, Faculty of Medicine of the University of Sao Paulo.
3. Medical Resident of the Office of Otorhinolaryngology, University Hospital Professor Edgard Santos Federal University of Bahia.
4. Associate Professor of Discipline of Otolaryngology, Faculty of Medicine of the University of Sao Paulo.
Department of Otolaryngology at University Hospital Prof.. Edgar Santos, Federal University of Bahia.
Marcus Miranda Lessa
Mailing address: John Street of boots s / n - Shin - Salvador / BA - Brazil - CEP 40110-160 - Office of Immunology - 5 floor - University Hospital Professor Edgard Santos - UFBA - Fax: (71) 3245-7110 - E-mail: imuno@ufba.br / lessamm@terra.com.br
This article was submitted in System Management Publications by R@IO em 17/11/2006 and approved on 21/2/2007 22:32:09