INTRODUCTIONAlthough the diversion of the septum and/or the nasal pyramid occurs in all races and in almost all age ranges, it is more diagnosed in young adults and less frequently in children. Its prevalence varies according to the age ranges groups (1).
The homeostasis, or sufficiency of the stomatognathic system, is intensely changed by the commitment and inadequacies that act on the growth process and the craniofacial development. The septum deformity is one of the main causes of nasal obstruction and feeding difficulty in the childhood, in addition to being able to cause locking of nasolacrimal ducts, rhinosinusitis episodes, repetition otitis media and the severe sequels of the buccal respirator (2).
Septoplasty had its origin at the end of the nineteenth century and comprised the simple removal of all the nasal septum structure, without any concern with the post-operative consequences.
Septoplasty is a surgical procedure intended for the correction of the nose septum deviation. It became a systematic surgery from Killian (1905), and since then, famous otorhinolaryngologists have been developing several surgical techniques, each with their advantages and disadvantages, and they are indicated individually for each specific type of septum deviation.
The septoplasty achieved a high level of excellence with the works of Cottle e Guillen (10). Cotlle published works in which he could show the possibility of correction for the septum and other structures, by an approach taking into account the nose as a unit, as a functional whole and the nasoseptal access with under-osteo-perichondrium displacement as of the so-called maxilla-premaxilla, with the production of tunnels between the mucosa and the septum osteocartilaginous skeleton.
For all techniques the need for septum mucoperichondrium displacement is common. Such displacement produces a break of microcapillaries that may originate post-operative bleeding, that in turn may appear as septum epistaxis or hematoma. In the literature, for this type of surgery, adhesion, epistaxis, hematoma and the septum drilling figure as the most frequent complications. The two last ones may be prevented by using intra-operative technical cautions, but even so, the report of post-operative bleedings is common, sometimes they are important. The need for use of nasal splint in septoplasty surgeries is not proved, and the comorbidities are similar in both procedures with or without buffer (5).
Some authors even consider the buffer totally unnecessary. However, because of the surgical risk the use of nasal splints at the end of the surgery, that are removed in the post-operative, is a common practice. The nasal splints usually represent a great post-operative discomfort and sometimes it becomes even a reason for the patient's desistence of the surgery.
The morbidities associated to the placing of nasal splints do not justify their everyday use with the intention of preventing the formation of adhesions, the nasal splint increases comorbidities such as the post-operative pain and discomfort (23).
The incidence of complications in nasal surgeries is rare. Septoplasty operations are considered to be potentially contaminated surgeries and they have no need for antibioticoprophylaxis for the low risk of post-operative infection (24).
This study is intended for evaluating the patients' degree of satisfaction in the performance of septoplasty with and without the use of nasal splints and whether they would or not undergo a new nasal surgery. The main reason in case of rejection of a new surgery was approached.
It also aims at evaluating the most frequent complications pursuant to the use or not of nasal splints after the septoplasty operation. The segmental evaluation of patients included the presence of hemorrhage in the immediate post-operative, the presence of infection, formation of abscesses, evaluation of pain, serial intervals breathing complaints between 72h and seven days after the surgery, and the presence of nasal crusts and adhesion.
METHODA randomized prospective clinical study, in which 152 patients were evaluated, between 14 to 68 years of age, septoplasty-operated by the Cotlle technique in the period of June 2004 and February 2006 at Hospital Angelina Caron.
The work was submitted to the ethics committee of Hospital Angelina Caron under the protocol number 003/2004.
The patients were selected for surgery according to a detailed anamnesis, physical exam and complementary examinations. Included in the study were only patients with complaint of significant nasal obstruction, selected and evaluated by the nasofibroscopy and computerized tomography when necessary. Computerized tomography was necessary in 4 cases for exclusion of polypoid pathology or need for association for opening of the face sinuses.
Only cases serviced with moderate to severe septum deviation received surgery indication, taking into account the strong symptomatology for nasal obstruction.
The average age ranged from 14 up to 68 years. The surgeries were executed always under general anesthesia and orotracheal intubation, and used the nasoseptal access with under-osteo-perichondrium from the so-called maxilla-premaxilla, with the production of tunnels between the mucosa and the septum osteocartilaginous skeleton (Cotlle's Technique). The cases in which conchectomy was carried out with total or partial dissection were remarked, and only those with treatment for allergy through nasal spray or intra-operative bilateral technique of infundibula dislocation were maintained.
Nasal surgery protocol came after applied in the immediate post-operative and during the ambulatory follow-up, by the same medical doctor who carried out the surgery.
The nasal splint removal was made between 48 and 72 hours. All of them, with or without splint, received analgesia in the post-operative with nimesulide and paracetamol up to 7 days, and azithromycin for 3 days as an optional antibiotic for prophylaxis.
Daily nasal curatives for 21 days and in the 7 first ones with ointment of neomycin associated to the topic use of nasal oxymetazonine hydrochloride 0.5%. On the other post-operative days the curative was maintained with cleaning and oxymetazoline 0.5% drops (3x a day), and the neomycin ointment was suspended.
The patients were distributed between two groups: Group A - 72 patients without nasal splint and group B - 80 patients with nasal splint.
The post-operative evaluation comprised blood-count, coagulogram, cholinesterase and blood sugar. The electrocardiogram was requested in patients older than 40 years of age.
In 152 patients 84 men and 72 women were evaluated, divided in two groups (group A without the use of nasal splint and group B with the use of splint). Group A (72) comprised 38 men and 34 women. Group B (80) is dived in 46 men and 34 women.
The surgery was carried out with general anesthesia and orotracheal intubation and the septum correction was made with employment of Cotlle's technique (2). Local infiltration of 10mls was performed bilaterally with lidocaine at 1% diluted with adrenalin in the proportion of 1:100.000. conchectomy by dissection or cauterization was not accomplished, but all patients were submitted to bilateral infundibula dislocation.
The multiple choice questionnaire contained 2 questions and the first one was about the patients evaluation as to the surgery (4 items: very bad, bad, good and excellent) and the second question about nasal reoperation (yes, no), when negative, explain why. (5 items: pain, bleeding, anesthesia, nasal splint, cannot answer).
All patients or their responsible signed the authorization term informing about the risks and possible complications of the surgical act indicated by the Brazilian Society of Otorhinolaryngology. The protocol was approved by the Ethics committee of Hospital Angelina Caron.
The data were submitted to statistical analysis by method of Que - Square or exact test of Fisher with significance of 5%.
RESULTSEvaluation of 152 patients, between two groups A and B showed a major discomfort of patients with the use of splint. We observe that the satisfaction index evaluated as very bad was of about 30% in group B, in contrast with 28% of group A in 72 hours. After the seventh day, we observe a slight reduction in this difference that oscillated by approximately 28%. Another fact to draw attention was the high level of satisfaction, the evaluation as good and excellent both in the first 72 hours and after one week in the group without the use of splint. It's important to remark that as a comparison the data reflect a more comfortable and faster recovery of this group as shown in Table 1 and Graphics 1 and 2.
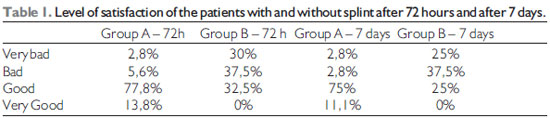
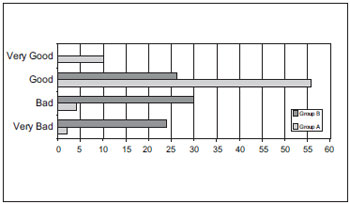
Graphic 1. Degree of Satisfaction in the first 72 hours.
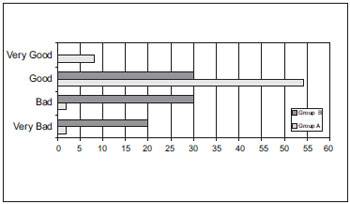
Graphic 2. Degree of Satisfaction after 7 days - Degree of Satisfaction after 7 days.
Another focus given to the work was a questioning about the possible future intervention. The majority of patients with splint was opposite to a new surgery, at least 70 of the 80 patients (87.5%), while in group A only 22.22% (16 patients out of 72) were contrary. This piece of information expresses the satisfaction and dissatisfaction as to the post-operative recovery and is compatible with the data evaluated 3 days after the procedure and along the first week. Questioned for the reason of such refusal, more than a half of group B, those who refused a possible new intervention (87.5%), described the splint as the main responsible (65.71%), superseding including the fear of anesthesia (17.14%), the pain amounted 5.71%, bleeding 11.42% and no patient opted for the answer of not being able to say (Graphic 3). In group A of those who wouldn't undergo the surgery, 50% opted for anesthesia, 12.5% for bleeding, 25% for pain and 12.5% couldn't say in a total of 16 patients who would refuse a new surgery, no patient mentioned the splint.
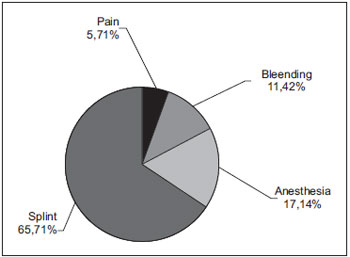
Graphic 3. Patients with the use of splint and who would not submit themselves to a new surgery.
The pain contradicts the results, because it was more frequent in group A, although a lower number of people, even though it didn't interfere directly with the most early and comfortable recovery of the patients analyzed.
152 operated patients were evaluated in the age range between 14 to 68 years, and the results were expressed in Tables 2 and 3 severally between group A (without nasal splint) and group B (with nasal splint).
Hemorrhage was light after 72 hours, and practically nonexistent in the immediate post-operative and after 7 days.
Septum-hematoma appeared in 5.5% of the cases in up to 72 hours, mainly in those in whom the relief incision was not suitable, and was generally lower than 0.5cm or much later.
Pain was major in the immediate period 5.5% and was controlled with analgesia.
Breathing difficulty reached 8.3% and was associated to the presence of nasal secretion.
Adhesion was confirmed in the upper portion, only in 2.7%, after 30 days.
Hemorrhage occurred moderately and was more intense in the immediate post-operative and practically nonexistent after 7 days.
Septum-hematoma appeared in 2.5% of the cases, right after the removal of the nasal splint.
Pain was major in the immediate period 5.0% and was controlled with analgesia.
Breathing difficulty was in 17.5%, and was associated to the presence of nasal secretion, not considered prior to the removal of the nasal splint, because it would be 100%.
Adhesion appeared in 5% of the cases, from moderate to severe, after 30 days.
In the comparison of the variables between groups A and B, the following results were observed (Table 4).
Compared statistically, the number was not significant (p0,013<0.05), but the absolute number of cases of group B with bleeding in the immediate post-operative (Table 5).
Compared statistically the number was not significant (p0,021<0,05), but the absolute number of cases in group A with septum-hematoma in the immediate post-operative was higher than expected (Table 6).
Compared statistically the number was significant (p>0.05), but the period prior to 72 hours in group B was not considered, because it would be 100% (Table 7).
Compared statistically the number was not significant (p0,001<0,05), but is remarkable the practically absolute control with analgesia after 72 hours in both groups (Table 8).
Compared statistically the number was not significant (p0,027<0,05), but group B had adhesions with higher anatomic extension than group A.
There were no signs of infection in the post-operative and the quantity of crusts and secretion was the same, moderate and light in both groups.
Both groups were evaluated according to the most frequent complications in the carrying out of the septoplasty surgery. The greatest of all complications presented in both groups was the presence of breathing difficulty, that occurred in 17.5% in group B and 8.3% for those who opted for not using the splint. It showed a significant difference between the groups after 72 hours, and suggested a faster recovery in group B. After 7 days this complaint was no longer identified. Differently, the pain showed to be present for a considerable period and the employment of analgesics was necessary in the first 72 hours, the complaint was not present anymore after the first week, and it was discreetly higher in group A, 5.5% before the 5% of group B.
The presence of hemorrhage in the immediate post-operative was major in group B (7.5%) than in group A (0%), and suggested the option for not using the splint at the first moment is positive in the short term, however such proportion was inverted after 72 hours, but not in as very significant manner as in the first moment (2.7% group A, 5% in group B). The abscess was observed with higher prevalence in the group without splint (5.55%), although these cases drainage incision had not been carried out previously.
The presence of infection in any of both groups was not observed. The presence of nasal crusts was from light to moderate in both groups without interference with the recovery after the suitable hygienization, therefore they were not registered in the table. Another crucial point was the identification of the major percentage of adhesion in the patients who used the splint (5%) compared to those who did not use it (2.7%).
DISCUSSIONAccording to Weber et al., the splint is used to compress not only the septum, but also the lower nasal infundibula, intended for preventing post-operative bleeding. However, such measures usually cause an enormous discomfort (specially the splint) to the patient (7). Our work comparing both groups confirmed the same statement mentioned in the study above, showed a higher number of complaints compared to the group that used nasal splint, about 30%, and evidenced the discomfort felt by such patients.
Sarandeses et al., in a study with 80 patients (40 with nasal splint and 40 without it) came to different results pursuant to the patient's satisfaction with the surgery and proved them to be similar in both groups (8). Our study showed a significant change in the patient's satisfaction. After 72 hours 77.8% of the patients considered the surgery to be good (satisfactory), and in group B 32.5% considered it to be good. After 7 days, even so the difference dropped a little compared to the 72 hours, passing to 75% group A and 25% group B, however an improving was observed compared to those who consider the surgery very bad, falling 5% in group B.
Guyuron et al., after evaluating 20 patients, came to the conclusion that 60% of the patients with splint, and its removal after 72 hours, complained of an extreme discomfort, when compared to the non-splint patients, and the main complaint was the splint removal (p<0.05) (9). After 72 hours 77.8% of the patients considered the surgery to be good (satisfactory), and in group B 32.5% considered it to be good. (p<0,005). In this comparative study, we cannot state that the main cause for discomfort was the splint removal, but it agrees with the data obtained in our work.
Weber et al., in a study with 60 patients, maintained the nasal splint for 5 days and it was well accepted by 58 patients (12). Our study compares in a conclusive manner since 87.5% of the patients who would not submit to a new nasal surgery, 65.71% would not undergo it for the discomfort of nasal splint use in the first surgery and its use tolerability is very low.
In their works most authors mentions as a great cause for the patient's non-acceptance of the surgery is the pain, aware (5, 7, 9, 10), but our study shows a percentage of 65.71% of patients operated who would not submit to a new surgery due to the use of splint and the pain is of 5,71% only of group B patients.
Gottschal et al. reports, upon comparing surgery with and without nasal splint (only suture, as in this work), that non-splint patients have a discomfort index lower without splint, because the air flows better right after the surgery (11). Perhaps this is the reason why non-splint patients reported a major fear of anesthesia (50%), for a lack of information this process of anesthesia induction still remains as a myth in our society, excluding the fear of using splint to a second plan. Since they didn't have to use it in the first surgery, they begin to have a higher degree of tolerability as for the procedure.
The splint is used to compress not only the septum, but also the lower nasal infundibula, intended for preventing post-operative bleeding. Such measures have been used since the beginning of nasal surgery (15) and generally bring an enormous discomfort (specially the splint) for the patient, in addition to delaying the recovery of mucociliary function and with this elevating the number of infectious complications (7).
However we have observed along the years a progressive diminishing in the splint use time and several groups all over the world have already been abandoning the use of such resources, with post-operative bleeding indexes similar to those found with their use. Probably the mastery of microendoscopic techniques of endonasal surgery, as well as the use of more efficient micro cauteries have been contributing to a reduction in the fear of nasal surgeries when it comes to these complications.
Recent studies showed that currently the septoplasty surgeries are carried out with a good satisfaction of the patient, with quality and safety; and low ranges of complication (25).
CONCLUSIONThe work information is specific for a region studied, but the use of nasal splint, although very diffused in our surgical middle, leads to the belief that it does not provide the patient's satisfaction, and many times a negative will to undergo a new nasal surgery, even if it is necessary.
Opposite from what is thought, the fear of general anesthesia or post-operative pain are not the main factor in the waive to submit to the nose surgery. The very splint can contribute in a decisive manner for the patients' option.
The surgical method acceptance is extremely important for its success. Therefore, as well as most surgeons do by proposing the carrying out of surgery with general or local anesthesia, they should also evaluate the technique to be employed and inform the patient on the possibility of carrying out the surgery with and without nasal splint.
The breathing difficulty got worse after the first 24 hours because of edema in the nasal infundibula, as well as the accumulation of secretion, fibrin and crusts, but such condition was reverted right in the first hours in the non-splint group, and was no longer a reason for complaint after the first week, differently from the group with splint. The pain was initially confirmed in the first 72 hours, as the table data, and simple analgesics were used resulting in symptoms improvement. The presence of nasal crusts was from light to moderate, however there were no signs of infection in the post-operative and the quantity of nasal crusts evolved similarly in both groups.
BIBLIOGRAPHICAL REFERENCES1. Wüllstein SR. Septoplasty without postoperative nasal packing. Mucosal repair of the upper airway with human biologica glue. HNO. 1979, 27(9):322-4.
2. Cottle M. Concepts of nasal physiology as related to nasal surgey. Arch Otolaryngol. 1960, 72:11.
3. Silvio C, Roberto L, Nelson C. Uso da cola de fibrina na prevenção de sangramento e hematoma pós-operatório em septoplastias. Rev Bras Otorrinolaringol. 2002, 68(5).
4. Otacilo e Campos. Tratado de Otorrinolaringologia. XXed. São Paulo: Roca LTDA; 1994. pp. 353-56.
5. Nunez DA, Martinz FW. Packing in nasal septal sugery. Clin Otolaryngol Allied SCI. 1991, 16(6):549-50.
6. Hytönen M, Blomgren K, Lilja M, Mäkitie AA. How we do it: Septoplasties under local anaesthetic are suitable for short stay surgery; the clinical outcomes. Clinical Otolaryngology. 2006, 31(1):64-68.
7. Weber R, Keerl R, Draf W, Schick B, Mosler P, Saha A. Management of dural lesions occurring during endonasal sinus surgery. Arch Otolaryngol Head Neck Surg. 1996, 122(7):732-6.
8. Sarandeses GA, López AM, Vázquez BJC. Ambulatory spetopyramidal surgery: methods,results and patients satisfaction. Acta Otorrinolaringol Esp. 2000, 51(8):703-7.
9. Lemmens W, Lemkens P. Septal suturing following nasal septoplasty, a valid alternative for nasal packing? Acta Otorhinolaryngol Belg. 2001, 55(3):215-21.
10. Guyuron B, Vaughan C. Evaluation of stents following septoplasty. Aesthetic Plast Surg. 1995, 19(1):75-7.
11. Gottschall KG. Am Improved suture technique. Am Plast Surg. 1978, 1(1):30-3.
12. Weber RK. Is packing of the nose up-to-date? Laringohinootologie. 2003, 82(9):650-4.
13. Eckel W. Tratamiento quirúrgico de las inflamaciones de las fossas nasales y de los senos paransales. In: Tratado de Otorrinolaringologia,Tomo I, Barcelona: Editora Cientifico-Medica; 1969, pp. 307-63.
14. Hayward PJ, Mackay IS. Fibrin glue in nasal septal surgery. J Laryngol Otol. 1987, 101(2):133-8.
15. Killiam G. The submucous window resection of the nasal septum. Ann Otol. 1905, 14:363.
16. Volkov A, Radev I. The use of autologous fibrin adhesive in septoplasty. Vestn Otorinolaringol. 1996, (1):45-7.
17. Wüllstein SR. Septoplasty without postoperative nasal packing. Mucosal repair of the upper airway with human biologica glue. HNO. 1979, 27(9):322-4.
18. Metzenbaum M. Replacement of the lower end of the dislocated septal cartilage versus submucous ressection of the dislocated end of the septal cartilage. Arch Otolaryngol. 1929, 9:282.
19. Passos CAC, Oliveira FMZ, Nicola JH.; Nicola JH, Nicola EMD. Cryptolysis via coagulation with CO2 laser for chronic caseous tonsillitis: conservatory technique and results. Rev Bras Otorrinolaringol. 2002, 68(3).
20. Hungria H. Otorrinolaringologia. 8th ed. Rio de Janeiro: Guanabara-Koogan; 2000, pp. 89-90.
21. Rosner B. Fundamentals of Biostatistics. 2nd ed. Boston: PWS Publishers; 1986.
22. Skevas A, Gosepath. Contribution to the closure of septal perforations (authors transl) Laryngol Rhinol Otol. 1975, 54(6):466-9.
23. Gaia R, Coelho J, Brandão FH, Carvalho MRMS, Aquino JEP, Paula SHP, Fabi RP, Eiras B. Frequência de Sinéquia Nasal após Cirurgia de Septoplastia com Turbinectomia com e sem Uso de Splint Nasal. Arq Int Otorrinolaringol. 2008, 12(1):24-27.
24. Caniello M, Passerotti GH, Goto EY, Voegels RL, Butugan O Uso de antibióticos em septoplastias: é necessário? Rev Bras Otorrinolaringol. 2005, 71(6):734-8.
25. Agha R, Heaton SR, Roberts D. Patient satisfaction with day-case septoplasty and septorhinoplasty. The Journal of One-Day Surgery. 2004, 14(1):22-25.
1. Master in Surgery by IPEM-PR. Otorhinolaryngologist Doctor and Preceptor of the Residential Services in Otorhinolaryngology of Hospital da Cruz Vermelha - Branch of Paraná and Hospital Angelina Caron.
2. Otorhinolaryngologist medical doctor. Preceptor of Residential Services in Otorhinolaryngology of Hospital da Cruz Vermelha - Branch of Paraná and Hospital Angelina Caron.
3. Otorhinolaryngologist medical doctor and Preceptor of Otorhinolaryngology Services of Hospitals da Cruz Vermelha and Angelina Caron.
4. Medical Doctor Specialized in Otorhinolaryngology.
5. Academic of the Twelfth period of the Medicine Course -FEPAR.
6. Academic of the Twelfth period of the Medicine Course - UNICEMP.
7. Academic of the Twelfth period of the Medicine Course - PUC.
Institution: Hospital Angelina Caron and Hospital da Cruz Vermelha - Branch of Paraná. Curitiba / PR - Brazil.
Mail address:
Eduardo Baptistella
Centro Médico Especializado Baptistella
Avenida João Gualberto, 1795, Conj. 01 - Juvevê
Curitiba / PR - Brazil - ZipCode: 80030-001
Fax: (+55 41) 3039-8878
E-mail: cmeb.cmeb@yahoo.com.br
Article received on May 25, 2008.
Article approved on August 28, 2008.