INTRODUCTIONThe Infraorbital Foramen is located in the maxilla bilaterally on its front side and is guided in the inferomedial direction located under the infraorbital edge at about 1.0cm. The artery, vein and infraorbital nerve pass by it (1,2,5,11,12).
The foramen may also be close to another foramen, referred to as Infraorbital accessory (1,2,5,6,7,9,10,11,12).
In the literature researched we have found the presence of up to four of such accessory foramens, and they are more common in the Mexican population (6.9).
The infraorbital nerve is taken as a continuation of the maxillary nerve, the second division of the trigeminal nerve (11, 12); it enters the orbit through the lower orbital fissure and successively occupies the Infraorbital infundibulum, channel and foramen.
The trigeminal nerve (V cranial pair) is the main sensitive nerve of the cephalic region, and is the motor nerve for the chewing muscles. It is divided into three branches: Ophthalmic, maxillary and mandibular. The maxillary nerve emits meningeal branches in its portion that is found in the medial cranial cavity and, when in the pterygopalatine cavity, it forms the sensitive part of the pterygopalatine ganglion. Upon leaving this cavity, it originates nerves: Upper alveolar, upper medial and frontal upper nerves and ends at its major branch, the infraorbital, which is externalized in the face through the foramen, with the same name, and is divided into branches that conduce the face skin, nose side, upper lip and lower eyelid sensitivity (1,2,5,7,9,10,11,12).
The infraorbital foramen and nerve are important surgical parameters for the Caldweel-Luc surgery.
The Caldwell-Luc surgery is a type of maxillotomy, whose passage has external access to the maxillary sinus, and has its idealizers' eponym. Having been carried out for many years, its main application is to benign diseases that affect the maxillary sinuses, such as: chronic sinusitis, fungal sinusitis, polyposis, biopsy, internal maxillary artery ligation for epistaxis, for benign tumors, oroantral fistulas and dental procedures. Some small malign tumors may also be extirpated by such passage. Its advantage is a good exposure of this sinus and its cavity, and may be enlarged up to the ethmoidal sinus and pterygopalatine cavity. Once its surgical limits and care with asepsis are met, a technique for closure and hemostasis is a relatively safe procedure. Its most frequent complications are lesions of the infraorbital nerve and lead to paresthesia/anesthesia of the facial region innervated by it and oroantral fistula for error in the closure or surgical injury infection. Maxillotomy is performed under local and general anesthesia, and an incision is made in the upper gengivolabial and gengivojugal sulcus, which extends from the lateral incisive tooth to the second or third molar tooth and makes a lifting of the muscular tissues up to the location of the infraorbital nerve that represents the upper limit for it has a passage in the orbit floor or in its anatomic variation in the roof of the maxillary sinus. At this moment, with the maxilla exposed, an osteotomy is made above the dental alveolus on the maxillary sinus front wall, which forms a window with approximately 0.2 cm
2 that gives access to the maxillary sinus cavity. The closure is made with plan by plan suture with absorbable strings (4,13).
The purpose of this study is to establish an average distance between the first pre-molar tooth alveolus top and the Infraorbital Foramen and nerve, in order to obtain a safe margin during the surgical access through the Caldwell-Luc's way.
METHODStudy authorized by the Medicine College of University of Santo Amaro and parts granted by the Anatomy discipline of UNISA (University of Santo Amaro), in the period of February to July, 2004.
We have dissected 32 heads of Brazilian adult corpses, already formolized, and the distinction of age, sex and color were not possible.
Surgical approach was made through the Caldwell-Luc's operation, until full exposure of the Infraorbital Foramen and nerve and then a line was traced from the first pre-molar tooth alveolus top to the abovementioned structures and the measures were made with the help of a pachymeter (Pictures 1 and 2) in both maxillas.

Picture 1. Infraorbital nerve in remark (blue string).

Picture 2. Access to the maxillary sinus (Caldwell-Luc).
The statistical methods were average estimates and the standard deviation.
RESULTSFor the analysis of our measures we used statistical methods where we calculated the average and the standard deviation.
The result found of the general average of distances between the alveolus top and the foramen was of 3.34 cm, with a standard deviation of 0.52 cm (Table 1 and Chart 1).
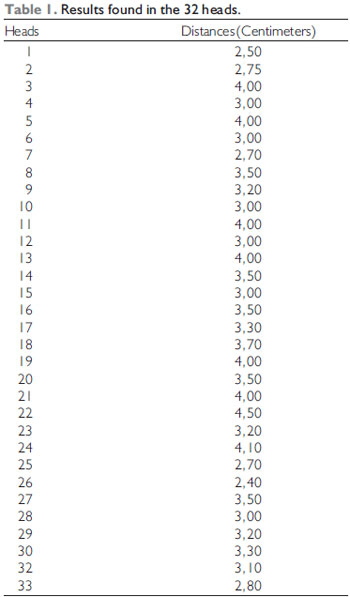
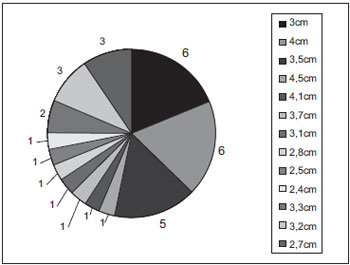
Chart 1. The average distances found in all dissected heads.
By the calculation of the standard deviation, 95% of such distances were between 2.30 cm and 4.38 cm and 68% between 2.82 and 3.86 cm.
In our crania studied the major distance found was of 4.50 cm and the minor was of 2.5 cm.
DISCUSSIONThe anatomic location of the Foramen and infraorbital nerve became significant with the advances of the surgical technique, both in otorhinolaryngology and ophthalmology, plastic surgery, head and neck surgery and dental surgery, as well as for the performance of local anesthesia in this nerve for manipulation of the area innervated by it.
The Infraorbital Foramen may have an accessory foramen by its side, which may be single or multiple as shown by Kaskayazi et al. (1), where 35 X-rays of adult crania face were analyzed, by using both sides. Single Infraorbital Foramen were found in 66 sides (94.3%), double ones in 04 sides (5.70%) and a bilateral double Foramen in 01 case.
Canan et al. (2), 54 (11.50%) of single accessory foramens were found in 119 crania and 229 maxillas studied; double accessory Infraorbital Foramens were found in 6 (1.28%) crania. This single accessory foramen was found in the left side of 26 corpses (48.10%) and in the right side of 28 (51.90%) corpses. In 46 parts studied (85.20%), these accessory foramens were in a horizontal plan relating to the Infraorbital Foramen, higher than it in 46 cases (85.20%), lower in 3 cases (5.60%) and in the same level in 5 cases (9.30%).
Karakas et al. (6) included that the accessory foramen may appear in 2 to 18% among all the populations, with a major prevalence in Mexicans, and it was also proved by studies of Aziz et al.(9) that also report up to 4 accessory foramens of the same side. In our study we have not found any accessory Infraorbital Foramen.
Most of the authors research the distance between the Infraorbital Foramen until the (MIO) Orbit's Lower Margin; in his book of descriptive anatomy, Moore reports this distance is of about 1.0 cm (11, 12).
Kazkayazi et al. (1) in their studies of 35 crania using both sides found an average distance of 7.19 mm and also traced an average distance between the Infraorbital Foramen and the lateral nasal edge of the pear-shaped opening, whose average found was of 17.23 mm.
Canan et al. (2) in their study with 45 corpses, 14 of female sex and 31 of male sex, reported they found the distance of 10 mm between the foramen and the MIO in 18 corpses in the right side (40%) and 14 in the left side (31.10%), total number with this distance: 32 corpses (35.50%). They also reported that in 31 corpses (68.90%), in the right side, the distance ranged from 08 to 12 mm and in 25 (35.50%) in the left side, with a total of 52 corpses. According to these results the interval of distance between the Infraorbital Foramen and the MIO was of 0.7 to 09.70 mm in the right side and 6.80 to 9.80mm in the left side, without significant difference between both sides and sex. However, they concluded that, between the foramen and the MIO in the women the distance is of 8.30 mm and in the men of 10.90 mm.
In the studies of Karakas et al. (6) who used crania (62 sides) of Caucasian adult men they found the distance of 7 mm between the Infraorbital Foramen and the MIO, in the same study they measured the distance between the aforesaid foramen and the Lower Orbital Fissure and the result was of 32 mm, compared to the studies of Rontal (15) who found distances of 24 mm and the study of Hwang and Baik (14) who found the distance of 26 mm.
Cutright et al. (7) upon analysis of 80 corpses of 20 white men and 20 black men, and 20 white women and 20 black women, reported 0.64 mm of distance between the Infraorbital Foramen and the MIO and stated there is a significant difference between men and women. In the same study they traced an average distance of 2.70 cm between the mid-maxillary line, in a horizontal plan, and the Infraorbital Foramen, with difference between men and women. They found an average distance of 0.03 cm between the foramen and the vertical zygomaticomaxillary in a horizontal plan.
Chung et al. (8) showed that the Infraorbital Foramen and the MIO have a distance of 9.0 mm in men and 7.80 mm in women. They used pictures of 124 Korean crania, 35 of male sex and 18 of female sex and in 71 crania it was not possible to tell the sex. However, they found the distance of 27.20 mm between the Infraorbital Foramen and the median line and 45.60 mm between this foramen and the Supraorbital Foramen, which showed us that relating to the latter, the Infraorbital Foramen is in a lateral position in 63.60% and that in 38.10% the Supraorbital Foramen, Infraorbital Foramen and the Mental Foramen are aligned.
Aziz et al. (9), upon studying 47 corpses of 24 men and 23 women, 33 white, 11 black and 3 Hispanics, reported that the distance between the Infraorbital Foramen and the MIO in men is of 8.50 mm to the right and 8.5 mm to the left and in women of 8.10 mm to the right and 7.5 mm to the left, having as the general average in both sexes: right side 8.3 mm; left side 8.10 mm. They have also studied the distance between the foramen and the mid-line and found an average of 27.90 mm to the right and 27.50 mm to the left in men and 25.50 mm to the right and 26.90 to the left in women. As for the Supraorbital Foramen, they found a distance of 43.30 mm to the right and of 43.20 mm to the left in men and of 42.20 mm to the right and 42.30 mm to the left in women. They also reported that about 50% of these two foramens are in the same vertical plan and found 30% to the right and 54% to the left in men and 52% of bilateral incidence in women. They further describe the Infraorbital Foramen is lateral to the Supraorbital Foramen in 40% of the times in man and 33% in women.
In 15% of the men and 13% of the women, the Infraorbital foramen is in medial relation with the Supraorbital. In addition, they show in the vertical plan the relation between the Infraorbital Foramen and the teeth, and at the right the foramen is in the same vertical line as the first pre-molar tooth in 64% of the times, with the canine tooth and second pre-molar in 17% and the first molar tooth in 2%. In the left side: 72% of incidence in the first pre-molar, 17% in the second pre-molar, 8% in the canine and 3% in the molar.
These results as to the incidence have led us to choose as a parameter the first pre-molar tooth for it is more often in the same horizontal plan of the Infraorbital Foramen and made our measuring to be as close as possible of a straight line.
In the worldwide literature surveyed we did not find a research on the distance between the dental alveolus and the Infraorbital Foramen and nerve.
Kazkayazi et al. (1) was the only author to trace this average of distance by using X-rays of the face. They have used as a parameter the lateral process of the canine tooth up to the Infraorbital Foramen and found the average distance of 3.39 mm, taking into account that they used the lateral process of the canine tooth alveolus and we have used the alveolus top of the first premolar tooth. Since both these structures are contiguous we can verify a slight difference in the average found, that was of 3.34 mm in our study and it led us to believe that this distance has a little difference since they have studied European crania and we have studied Brazilian crania.
CONCLUSIONThe average distance from the first premolar tooth alveolus top to the Infraorbital Foramen is an important surgical parameter for the external access to the maxillary sinus.
Our study has revealed an average of 3.34 cm and a standard deviation of 0.52 cm.
We have not found works relating to this kind of measure.
We remark the continuity of the study
in vivo or fresh corpse with distinction of race, age and sex so we can trace with major precision this average distance, which may contribute for more safety in the Caldwell-Luc's operation.
BIBLIOGRAPHICAL REFERENCES1. Kazkayasi M, Ergin A, Ersoy M, Bengi O, Tekdemir I, Ethan A. Certain Antomical Relations and the Precise Morphometry of the Infraorbital Foramen-Canal and Groove: An Anatomic and Cephalometric Study. The Laryngoscope. 2001, 111:609-14.
2. Canan S, Asim OM, Okan B, Alper M. Anatomic Variations of the Infraorbital Foramen. Annals of Plastic Surgery. 1999, 43(6):613-17.
3. Ohki M, Takeuchi N. Objective Evaluation of Infraorbital Nerve Involvement in Maxillary Lesions by Means of the Blink Reflex. Arch Otoryngol Head Neck Surg. 2002, 128:952-55.
4. Couldwell WT, Sabit I, Weiss MH, Gainnota SL, Rice D. Transmaxillary Approach to the Anterior Cavernous Sinus: A Microanatomic Study. Neurosurgery. 1997, 40(6):1307-11.
5. Kazkayasi M, Ergin A, Ersoy M, Tekdemir I, Ethan A. Microscopic anatomy of the infraorbital canal, nerve and Foramen. Otolaryngology-Head and Neck Surgery. 2003, 129(6):692-97.
6. Karakas P, Bozkur MG, Oguz O. Morphometric measurements from various reference points in the orbit of male Caucasians. Surg Radiot Anat. 2002, 24:358-62.
7. Cutright B, Quillopa N, Schubert W. An Anthropometric Analysis of the Key Foramina for Maxillofacial Surgery. J Oral Maxillofac Surg. 2003, 61:354-57.
8. Chung MS, Kim HJ, Kang HS, Chung IH. Locational Relationship of the Supraorbital Notch or Foramen and Infraorbital and Mental Foramina in Koreans. Acta Anat. 1995, 154:162-66.
9. Aziz SR, Marchema JM, Puran A. Anatomic Characteristics of the Infraorbital Foramen: A Cadaver Study. J Oral Maxillofac Surg. 2000, 58:992-96.
10. Danko I, Hang RH. An Experimental Investigation of the Safe Distance for Internal Orbital Dissection. J Oral Maxillofac Surg. 1998, 56:749-52.
11. Moore KL. Anatomia Orientada para o Clínico; 1992, 3ª edição, Cap. 07, 578-91,600-01.
12. Moore KL. Anatomia Orientada para o Clínico; 1992, 3ª edição, Cap. 09, 782-83.
13. Hungria, H. e cols. Hungria Otorrinolaringologia; 2000, 8ª edição, Cap. 01,46-47.
14. Hwang K, Baik SH. Surgical Anatomy of Korean Adults. Journal Craniofacial Surgery. 1999, 10:129-134.
15. Rontal E, Rontal M, Guilford FT. Surgical Anatomy of the Orbit. Ann Otol. 1979, 88:382-386.
1. Specialist. Medical Residence Coordinator UNISA Otorhinolaryngology.
2. Doctor Professor. Head of the UNISA Otorhinolaryngology Discipline.
3. Doctor Professor. Professor and Head of UNISA Otology Discipline.
4. Resident Medical Doctor of UNISA Otorhinolaryngology.
Institution: Otorhinolaryngology Discipline of the Medicine College of UNISA (University of Santo Amaro). São Paulo / SP - Brazil.
Mail address:
Fabiano Haddad Brandão
Avenida Engenheiro José Salles, 200 - Apto. 136 - Bloco 5
Interlagos - São Paulo / SP - Brazil - Zip Code: 04776-100
E-mail: fh.brandao@terra.com.br
Article received on July 14, 2008.
Approved on September 25, 2008.