INTRODUCTIONSinusal diseases affect millions of people. North-American studies assert that annually approximately 31 millions of North-Americans are affected by chronic rhinosinusitis (1).
The therapeutic options include since the medication treatment through immunoallergic cares up to surgical interventions. Fortunately in most cases the clinical treatment is efficient. Even though this therapeutic option has some limitations, such as bacterial resistance to the antibiotics, collateral effects and discipline of the patients (2).
In some cases of failure in the clinical treatment, mainly when structural anatomic changes are involved to the nasal endoscopy or computerized tomography (CT) exams, the functional endoscopic surgery is the current choice method for the patients surgical treatment.
The objective of the functional endoscopic surgery (FES), although it's been discussed by some authors, is to increase the ventilation and draining of the paranasal sinuses involved and allow the return of adequate functioning of the mucociliary movements of the nasal mucosa (2).
In spite of embodying several benefits when compared to traditional open procedures, this method still raises some issues and inherent limitations, mainly because it ends up removing the nasal mucosa and osseous tissue, which leads to pain, bleeding, physiological changes of the nasosinusal mucosa, specially of the mucociliary movements and local cicatricial fibrosis (2,3).
Annually approximately 330 thousand North-Americans are submitted to FES and many of them end up presenting with some recurrent symptoms, even after the accomplishment of such procedures, mainly when they present with allergic features (4,2).
Many of these patients who are submitted to FES could be benefited with less invasive methods, with major preservation of the nasal mucosa (2). In the interim, alternative technologies and techniques for the accomplishment of the nasal endoscopic surgery. In a work published in 2001, Nayak and collaborators proposed the physiological endoscopic approach, with conservation of the nasal mucosa and the hamate process in the surgical management of patients with chronic rhinosinusitis associated with allergic symptoms. The authors propose the performance of physiological nasosinusal surgery, with very good results when compared to patients submitted to traditional functional endoscopic surgeries (2). Unfortunately, a few later studies were published by these authors with follow-up and a higher number of patients involved. Other methods have also been published, but with scarce works of later follow-up.
As from 2006, a still less invasive procedure was remarked in our specialty: the balloon dilation of the paranasal sinuses ostia. Such technique was raised with a great remark in the United States for the increase of the PNS's ostia, specially in the frontal and sphenoidal maxillary sinuses, in an attempt to treat nasosinusal diseases (6,7,8). Such balloon dilation system followed the principle of guide thread already consecrated in vascular surgeries, intervening cardiology and urology.
What such system allowed was the dilation of PNS ostia and their vicinities through the use of balloon which could support high pressures. The system was also drawn for the insertion of catheters for secretion washing and aspiration (6,7,8).
The method, titled sinuplasty, initially presented a new concept of nasal endoscopic surgery, but received several criticisms from the North-American medical community. Today the sinuplasty is taken as a tool that in some cases dilates the PNS natural ostia; however without tissue removal. This new tool doesn't replace the nasal endoscopic surgery, but it may be a new resource in the treatment of some selected patients.
In Brazil we don't have works on this theme yet, therefore the objectives of this article are:
a) To define the concept of sinuplasty, action mechanism and describe the material required for the procedures performance.
b) To describe the techniques used with the Equipment Relieva Sinus Balloon Catheter System (Acclarent, INC, Menlo Park, California) in functional endoscopic surgery simulator model - Sinus Model Otorhino-Neuro Trainer, S.I.M.O.N.T. (Prodelphus, Brazil).
c) To review in the current literature, the indications, complications, results and follow-ups of patients submitted to this procedure.
LITERATURE REVIEW
ConceptSinuplasty is a medical procedure with dilation by means of a balloon of the PNS ostia region. This procedure is currently used in the maxillary, frontal and sphenoidal sinuses (6,7,8,9). These tools functioning basic concept is that the dilation of the desired region, which may lead to 16 pressure atmospheres in the balloon, produces local microfractures that end up remodeling the anatomy, dilates the ostia and allows a PNS normal aeration without, however, the removal of the tissues and damage to the nasal mucosa. This makes this procedure still less invasive than the consecrated FES (6,7).
We initially made safety and feasibility studies of dilation in corpses in the United States, which presented with good results, followed-up in 2006, for the first study in patients (8).
In 2008, in a multicentric study of the paranasal sinuses ostia dilation results in 1.036 patients, the authors came to a conclusion the use of these instruments for the dilation was safe, effective and improved the life quality of the patients (9).
These procedures are carried out under general anesthesia and may be made separately, and are called pure sinuplasty or, in cases of nasal polyps or other diseases, specially in ethmoid, matched with traditional endoscopic surgeries, referred to as hybrid procedures.
Material requiredFor the performance of the sinuplasty, traditional functional endoscopic surgery material is required, as well as specific tools (3).
Endoscopes sets of 0, 30, 45 or 70 degrees may be used. In addition, a set of guide-catheters, flexible guide-threads, flexible balloon-catheters, washing catheters and pump for the balloon insufflation with manometer are necessary (3).
The guide-catheters are available in several angulations. There are catheters for the sinuses: frontal, with 70 degrees angulations; maxillary, with 90 to 110 degrees angulations; and sphenoidal, with 0 to 30 degrees angulations. There is also the maxillary sinus catheter for pediatric use, with a diameter minor than 110 degrees angulations (Picture 1).

Picture 1. Available guide-catheters. There are several angulations for the different paranasal sinuses. S-0 and S-30 for sphenoidal sinus; M-110 and M-90 for maxillary sinus; M110S for pediatric maxillary sinus; F-70 for frontal sinus.
The insufflation pump (Picture 2) consists of a high pressure syringe with piston and manometer used for the balloon pressure monitoring at the tip of the catheter.

Picture 2. Insufflation pump with manometer.
The solution used for balloon insufflation may be physiologic saline at 0.9%, when luminous catheter is used, which allows the identification of the paranasal sinus through dermametropathism, or contrast, in cases of fluoroscopy use (3).
Six to eight millimeters are required to achieve the recommended pressures. The system must be free from air bubbles for the correct functioning.
The balloons are coupled in catheters (Picture 3). The balloon standard size is of 5 millimeters, although there are balloons of 7 and 3 mm. The suitable size of the balloon to be used will depend on the size of the paranasal sinus ostium desired by the surgeon (3).

Figura 3. Balloon catheter.
The balloon insufflation maximal pressure recommended by the manufacturer is of 16 atmospheres (atm). Generally pressures ranging from 8 to 12 atms are used with good results (3,10).
The same balloon may be used and dilated in several paranasal sinuses in the same session of the same patient (3).
There are also several catheters available for washing, and the guide-thread, made of hard material, but with a very flexible and atraumatic tip for the location of the PNS ostia.
Currently there are basically two tools for location and certainty that the balloons are well positioned for the paranasal sinuses ostia dilation: the use of fluoroscopy and luminous catheters. When fluoroscopy is used an arc in "C" must be used, because all the material available for the performance of this procedure has radiopaque markers that enable the orientation through fluoroscopy (3).
The luminous catheters have small optical fibers at their ends which make the location possible through dermametropathism (3).
In our service, we have been developing a system for localization of the balloons through a browsing system based on portable PC - "compact laptop image-guidance system" (Picture 4A). In this case, we would not use fluoroscopy or dermametropathism.
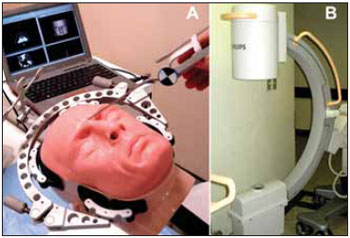
Picture 4. A: Browsing system under development based on portable computer. B: Arc in "C", common to several surgical centers, for procedures performance with the help of fluoroscopy.
Although seldom used by otorhinolaryngologists, the arcs in "C" (Picture 4B) are generally available in most surgical centers, and their operation is relatively easy.
For performance of the procedure with the help of fluoroscopy, the arcs in "C" are positioned close to the end at which the patient's head is positioned in the surgical table. Depending on the sinuses ostia to be dilated, an antero-posterior or lateral image is carried out (Table 1).
In patients with involvement of the three groups of paranasal sinuses (maxillary, frontal and sphenoidal) we recommend the start of procedure with AP image, for the performance in the maxillary and frontal sinuses. After their dilation, we recommend the use of profile image for identification and dilation of the sphenoidal sinus ostium (3).
TechniqueWe describe the technique for carrying out this procedure, similar to the manufacturer instruction and the techniques described in the literature for accomplishment of sinuplasty in patients (3).
Therefore, we use the dilation equipment by balloon Relieva Sinus Balloon Catheter System (Acclarent, INC, Menlo Park, California) in a model similar to FES, entitled S.I.M.O.N.T. (Sinus Model Otorhino-Neuro Trainer) developed in our center along with ProDelphus (Picture 5).

Picture 5. Equipment for balloon dilation Relieva Sinus Balloon Catheter System (Acclarent, INC, Menlo Park, California) and functional endoscopic surgery simulator model - Sinus Model Otorhino-Neuro Trainer (S.I.M.O.N.T.) (Prodelphus, Brazil).
After mounting of the catheter-guide set, balloon catheter, guide-thread and pump, the equipment was smoothly inserted into the nasal cavity.
It's worth remarking that each PNS ostium to be dilated requires a specially developed guide-catheter. We started with the left frontal sinus ostium dilation, followed of the left maxillary and sphenoidal and right maxillary, sphenoidal and frontal ostia dilation.
We used 0 to 45 degrees endoscopes. Under an endoscopic view, with positioning of the guide-catheter in the region close to the PNS ostium (Picture 6), the guide-thread was slowly inserted for catheterizing of the desired PNS (Picture 7). After certification of the guide-thread insertion into the PNS, the balloon catheter was introduced, by using the guide-thread as a rail.

Picture 6. Endoscopic view (45 degrees) of the guide-catheter positioning in the region close to the left frontal sinus ostium in a S.I.M.O.N.T. model.

Picture 7. Endoscopic view (45 degrees) of the catheterizing with guide-thread of the right frontal sinus in the S.I.M.O.N.T. model.
The balloon catheter has radiopaque markers for identification of the proper positioning into the PNS ostium under fluoroscopy.
After certification of the catheter positioning, the balloon was insufflated with the help of the pump. We used the pressure of 10 atm for the PNS ostia dilation of our model (Picture 8).

Picture 8. Endoscopic view (45 degrees) of ostia dilation of the right frontal sinus in the S.I.M.O.N.T. model.
The dilation was successfully made, since each PNS ostium didn't present with major difficulties.
Patients' indicationsPerhaps the most precise current indication with more subsides in the literature for the performance of these procedures is for patients with chronic rhinosinusitis associated to allergies (2,3,7).
A recent retrospective study with 70 adults with chronic rhinosinusitis and surgical indication for failure in the clinical therapy was divided into two groups: patients submitted to FES and patients submitted to balloon dilation, showed that both FES and balloon dilation resulted in a significant improvement of the patients' life quality; however the postoperative satisfaction and complaints were greater in the patients submitted to balloon dilation. The paranasal sinuses infection recurrence index was similar in both groups (11).
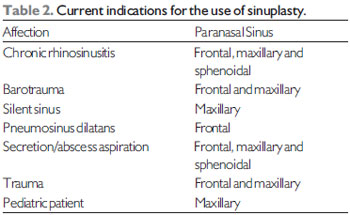
Other indications that use the PNS ostia balloon dilation include (Table 2): barotrauma, in which the dilation, without removal of the mucosa, may benefit the patients when compared to the commonly used procedures; pediatric surgeries, in which there is affection of PNS in children and the surgeon opts for the less local invasive procedure; secretion aspiration in patients in intensive care unit, where PNS ostium dilation is made and enables secretion aspiration, by avoiding more traumatic biopsies; cases of post-operative cicatricial stenosis, in which the dilation may remodel the local tissues and prevents stenosis of the PNS ostium region; trauma, in which fractures may be reduced with the use of balloons (12,13), silent sinus syndrome, pneumosinus dilatans etc.
Currently, there are two large trends in the use of catheters and balloons: performance of the procedures referred to as hybrid, in which there are traditional FES steps and steps in which the balloon is used both for dilation and identification of the paranasal sinuses with major difficulties, such as the frontal sinus, and use of local medications by means of catheters in PNS.
It's important to remark this is a recent procedure and many indications may still appear and disappear.
ComplicationsIn a recent multicentric study in which 1.036 patients were retrospectively evaluated with chronic rhinosinusitis, not responding to clinical treatment, submitted to balloon dilation in the PNS ostia; there was no case of major adverse complication with the use of the devices utilized in the sinuplasty procedure (9).
There were two cases of liquoric fistula reported in patients submitted to hybrid procedures, balloon dilation and concomitant ethmoidectomy. However, such fistulas were not ascribed to the balloon tools, but to instruments used in the ethmoidectomy accomplishment (9).
In six cases of patients submitted to hybrid procedures, there was nasal bleeding in which surgical cauterization and nasal splint were required. None of the cases presented the need for blood transfusion. The bleeding were also associated to the use of FES traditional techniques and not the use of balloons (9).
Out of 1.036 patients treated in this study, 25 (2.4%) needed review procedures. As for the number of ostia dilated , out of 3.276 ostia, 41 (1.3%) needed review: 1.3% maxillary; 1.2% frontal and 1.3% esphenoidal (9).
Results and follow-upIn this very multicentric study, out of 1.036 patients treated with PNS ostia balloons dilation, 95.5% had symptoms improvement in the surgeon's opinion (9).
With 24-month follow-up, 73.8% of the patients were free from sinusal infections after accomplishment of PNS ostia dilation with balloon, compared to 18.5% of patients with 1 postoperative sinusal infection, 5.2% with two postoperative sinusal infections; 1.9% with three sinusal infections; 0.5% with four cases of postoperative sinusal infection and 0.1% with five or more sinusal infections.
The postoperative cares were also evaluated in the 60 initial days after the procedures performance. Less crusts removal was required and there were less complaints in patients submitted to sinuplasty compared to those submitted to hybrid procedures (9).
DISCUSSIONRecent advances in the understanding of new concepts, such as biofilms, in the optimization of medications and surgical techniques and tools make the nasosinusal diseases treatment to go on in full evolution (5).
In the surgical area microdebriders and browsing systems were advances recently incorporated in the practice of otorhinolaryngologists. Initially such new appliances were resisted by surgeons due to changes to consecrated operatory techniques, technology usage and cost. However, the use of such new tools enabled the advance in the treatment and better results proved by the patients.
The introduction of sinuplasty, PNS ostia dilation by means of balloon, seems to undergo a similar phase too. Some works have been published on this theme since 2006, but there are still many questions without answers.
With this review, we attempt to bring such discussion to Brazil, a country with more than 4 thousand otorhinolaryngologists and that may play an important role for the development and applications of this new tool. Many doctors place special resistance against the use of radiation for the accomplishment of these procedures. There are some works in the literature concerning the exposure of patients and surgeons to radiation in the performance of sinuplasty procedures (14,15).
The surgeons must be aware there is a learning curve and adaptation for this procedure accomplishment. This requires longer time of radiation exposure, which may bring problems such as radiation exposure to the retina and mainly to the lens of the eyes of the patients.
The use of fluoroscopy in the sinuplasty operation must not exceed 30 minutes for dilation of the six potential paranasal sinuses ostia, which ensures a fluoroscopy time of about 5 minutes per ostium. Where this time is respected, the use of fluoroscopy in the PNS ostia dilation with the use of balloons expose both the patient and the surgeon to low dosages of radiation (14,15).
A FES success evaluation objective parameter is the number of review procedures. Although the literature is variable on the review indexes with FES in chronic rhinosinusitis, most studies bring rates of 10% after one year of follow-up. In the frontal sinus such indexes may be of up to 30% (11).
With the use of balloons for remodeling of the PNS ostia and adjacent spaces, recent studies show high indexes of patency with a much longer duration than the typical cicatricial period. The review indexes of 1.3% show this technology is very promising for the treatment of patients (9).
It's important to remark as it's a recent technology, there are only a few studies in the literature with long follow-up. A prospective and randomized study on this new technique has not yet been carried out so far. The most detailed study in the literature may also bring satisfactory data, but it has, for a more critical reader, several questions such as ostia patency, in which the objective parameter for such evaluation is not clarified.
FINAL COMMENTSThe sinuplasty is a new procedure in which balloons are inserted into dilated PNS ostia and produces local micro-fractures, remodels the anatomy without, however, removing the nasal mucosa.
This new tool is safe and seems to be efficient for the life quality improvement of patients who don't respond to conventional clinical treatments.
The literature brings several works on this new theme, with very good results. This technology development goes on and our country may play a critical role for the appearing of new equipment, with adaptation of the balloons to a browsing system.
New applications and indications for this equipment must also be raised and researched. Nevertheless, such novelties will bring more questioning, challenges, criticisms and resistance of some surgeons.
It's important to be attentive to be, like today, at the vanguard of surgical techniques development in our specialty.
BIBLIOGRAPHICAL REFERENCES1. Benninger MS, Ferguson BJ, Hadley JA, Hamilos DL, Jacobs M, Kennedy DW, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003, 129:S1-S32.
2. Nayak DR, Balakrishnan R, Murty KD. Endoscopic physiologic approach to allergy-associated chronic rhinosinusitis: a preliminary study. Ear Nose Throat J. 2001, 80:390-403.
3. Friedman M, Schalch P. Functional endoscopic dilatation of the sinuses (FEDS): patient selection and surgical technique. Op Tech Otolaryngol Head Neck Surg. 2006, 17:126-34.
4. Anand, VK. Epidemiology and economic impact of rhinosinusitis. Ann Otol Rhinol Laryngol Suppl. 2004, 193:3-5.
5. Vaughan W. Review of balloon sinuplasty. Curr Opin Otolaryngol Head Neck Surg. 2008, 16:2-9.
6. Brown CL, Bolger WC. Safety and feasibility of balloon catheter dilation of paranasal sinus ostia: a preliminary investigation. Ann Otol Rhino Laryngol. 2006, 115:293-9.
7. Bolger WE, Brown CL, Church CA, Goldberg AN, Karanfilov B, Kuhn FA, et al. Safety and outcomes of balloon catheter sinusotomy: a multicenter 24-week analysis in 115 patients. Otolaryngol Head Neck Surg. 2007, 137:10-20.
8. Bolger WE, Vaughan WC. Catheter-based dilation of the sinus ostia: initial safety and feasibility analysis in a cadaver model. Am J Rhinol. 2006, 20:290-4.
9. Levine HL, Sertich AP 2nd, Hoisington DR, Weiss RL, Pritikin J. Multicenter registry of balloon catheter sinusotomy outcomes for 1,036 patients. Ann Otol Rhinol Laryngol. 2008, 117(4):263-70.
10. Brehmer D. Catheter-based balloon dilatation of the frontal, maxillary, and sphenoid ostia: a new procedure in sinus surgery. HNO. 2008, 56(1):65-70.
11. Friedman M, Schalch P, Lin HC, Mazloom N, Neidich M, Joseph NJ. Funcional endoscopic dilation of the sinuses: patient satisfaction, postoperative pain, and cost. Am J Rhinology. 2008, 22: 204-9.
12. Slow JK, Al Kadah B, Werner JA. Balloon sinuplasty: a current hot topic in rhinology.Eur Arch Otorhinolaryngol. 2008, 265(5):509-11.
13. Hueman K, Eller R. Reduction of anterior frontal sinus fracture involving the frontal outflow tract using balloon sinuplasty.Otolaryngol Head Neck Surg. 2008, 139(1):170-1.
14. Chandra RK. Estimate of radiation dose to the lens in balloon sinuplasty.Otolaryngol Head Neck Surg. 2007, 137(6):953-5.
15. Church CA, Kuhn FA, Mikhail J, Vaughan WC, Weiss RL. Patient and surgeon radiation exposure in balloon catheter sinus ostial dilation.Otolaryngol Head Neck Surg. 2008, 138(2):187-91.
1. Master's Degree in Medicine. Resident in Otorhinolaryngology.
2. Doctor. Director of the Otorhinolaryngology and Phonoaudiology Center of São Paulo - Hospital Professor Edmundo Vasconcelos.
Institution: Centro de Otorrinolaringologia e Fonoaudiologia de São Paulo - Hospital Professor Edmundo Vasconcelos. São Paulo / SP - Brazil
Mail address:
João Flávio Nogueira Júnior
Rua Borges Lagoa, 1450 - 3º Andar - Prédio dos Ambulatórios
Vila Clementino - São Paulo / SP - Brazil - Zip code:
04038-905 - Fax: (+55 11) 5080-4357
www.centrodeorl.com.br
E-mail: joaoflavioce@hotmail.com
Article received on July 30, 2008.
Approved on October 19, 2008.