INTRODUCTIONThe nasosinusal surgery presented a fast development in the last two decades, mainly levered by the introduction of endoscopes to its praxis. The concept of functional endoscopic sinus surgery (FESS) (1), that approaches the paranasal cavities so as to provide conservation of the nasosinusal mucosa as much as possible, is well accepted, broadcast and has great results. However, cicatricial stenoses secondary to surgical manipulation still occur, even in the hands of experienced surgeons and, mainly, in narrow regions, such as the frontal recess (2,3).
Recently, the techniques based on catheterization and dilation have been benefiting many patients in the most different areas of medicine. This method has been used successfully in the fields of urology, gastroenterology, vascular surgery and cardiology (3). Based on this, in 2002, bioengineers of California started projects aiming at adapting the dilation system by balloon used in interventionist cardiology to perform the sinusal ostia dilation. Balloon sinuplasty appeared, also called "functional endoscopic dilatation of the sinuses" (FEDS) by some authors (4,5). We suggest this principle of dilation by catheter-guided balloons is less traumatic to delicate tissues than the common surgical procedures. The balloon dilation primarily distends the tissue while in the surgery the material is cut and removed. As for the delicate nasosinusal mucosa, the dilation may prevent mucous lesion, by reducing the tissue damage and the formation of adhesions.
In 2005, this new technology was approved for use in the United States by the Food and Drug Administration (FDA) as a minimally invasive treatment alternative for the chronic rhinosinusitis. Since then, some articles have been showing its feasibility, safety and capacity for improvement of the patients' life quality.
The objective of this work is to present and discuss the balloon sinuplasty surgical technique, indications, costs and results, through articles published so far about the subject.
LITERATURE REVIEW
IndicationsThe ideal patient would be that with a chronic or acute recurrent rhinosinusitis record, without improvement with the use of antibiotics, topic corticosteroids and/or allergy management. The patients studied in the first works presented with an altered computerized tomography with a Lund-Mckay score of (6) < 10 or 12 (4,5).
In addition to its use in patients with chronic rhinosinusitis, this system may also be a good option in those patients at intensive care units, where there is a suspicion of sinusal focus resulting in a febrile picture (2,4). As these patients are generally anticoagulated and in a critical clinical state, a minimally invasive approach, with low risk of bleeding and short time duration (by the anesthetic risk), would be an excellent option (3). After the ostium dilation, material collection for culture, biopsy and sinus lavage are possible (3,4). The sphenoidal ostium, for example, may be easily dilated to an extent of allowing access to a 4mm-endoscope (4).
Patients with coagulopathy may also benefit from less bleeding risk (2,3).
The use of balloon has other indications of great interest. It may be an alternate for the Silent Sinus Syndrome, in which the uncinectomy, in a fine uncinated and lateralized process, represents a risk of lesion of the orbitary contents (2)
Another possible indication would be its use in combination with the functional surgery, specially in the difficult review cases. The cannulation guided by fluoroscopy and dermametropathism may be very helpful in the frontal review surgeries (4). Hueman et al, 2008 mentions the use of balloon for reduction of fractures in the anterior table frontal sinus. In this case, the balloon is inflated inside the sinus and then in the frontal recess region. After 7 months of follow-up, there was recovery of the frontal sinus physiologic function without any cosmetic sequel (7).
Table 1 shows the main indications and contraindications for the use of balloon (2-4,8).
Surgical techniqueThe procedure is carried out under partial endoscopic viewing and may be made with local or general anesthesia. Rigid endoscopes of 0o, 30o and 45o are used in the procedure. In addition to the catheters with balloons (Picture 1), there are guide-catheters with several angulations (Picture 2), required to lead the catheters with balloon to the margins of the region to be dilated. The set also includes catheters for sinus lavage and a device coupled to a monometer (Picture 3) used to inflate the balloons. The balloons are inflated with an iodized contrast diluted in water or sterile saline, in an approximate concentration of 150-180mg/ml. The contrast is used to enable the location of the inflated balloon through fluoroscopy. Generally 6 to 8 ml of contrast are required to achieve the desired pressures. The normal balloon has 5 mm, but there are also with 3 to 7 mm. Generally pressures from 8 to 12/atm are sufficient for dilation, and the maximum recommended pressure is of 16 atm. Pressures above these increase the risks, for instance, of Agger Nasi cell fracture and of the terminal recess in cases of frontal recess dilation (4). Recently we have also been using an optical fiber system for location of the sinus through dermametropathism.

Picture 1. Catheters with balloons for sinusal dilation of different sizes (Cortesy by Acclarent Inc., Menlo Park, CA).

Picture 2. Semi-flexible guide-catheters of several angulations (Cortesy by Acclarent Inc., Menlo Park, CA).

Picture 3. Device to inflate balloon (Cortesy by Acclarent Inc., Menlo Park, CA).
Under endoscopic viewing, the guide-catheter is placed close to the sinusal ostium. A guide thread is passed across the guide-catheter, by fluoroscopy, through the sinus. The balloon catheter is then passed on the guide thread through the sinusal ostium region. After the correct location of the balloon in the sinusal ostium by fluoroscopy, the pressure inside the balloon is gradually increased by the iodized contrast infusion. After dilation, the balloon is gradually emptied and the catheter is removed (Picture 4).
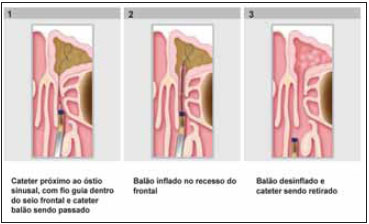
Picture 4. Balloon Sinuplasty technique (Cortesy by Acclarent Inc., Menlo Park, CA).
The first works published sought to evaluate the feasibility and the safety of the use of balloon in the practice. In the first study using corpses, Bolger WE (3) et al used six human heads, in which 31 ostia were dilated. These included 11 frontal, 11 sphenoid and 9 maxillary ostia. Computerized tomography was made with fine cuts of 1.25mm, before and after the dilations. In addition to the dilation success confirmation in the endoscopy, special attention was given to possible accidental lesion signs of the cranial base and the papyraceous lamina. The corpses were also examined as for possible lesions in the lateral lamella and the cribriform plate. The balloon catheters dilated all ostia successfully. The dissections didn't show lesion of any noble structure adjacent to the ostia. Upon observation of the ostia after dilation, the sphenoidal sinus ostia dilation proved to be more significant in its lateral portion, and the procedure also resulted in the lateralization of the posterior and lower portion of the upper infundibulum. In the frontal recess, the dilation prevailed medially, the Agger Nasi cell was molded mainly in its medial and posterior portion and was displaced in its lateral, anterior and lower parts. When inserted in the papyraceous lamina, the uncinated process had its upper portion lateralized. In the maxillary sinus ostium, the dilation provoked an anteriorization of the uncinated process lower third.
After accomplishing the balloon dilation in 10 patients, and a total of 18 sinuses, Brown CL et al (2) considered that: The easiest sinus to cannulate was the sphenoidal one, followed by the frontal and the most difficult was the maxillary sinus, due to the large angulation of the guide-catheter required to transpose the posterior end of the uncinated process towards the ethmoidal infundibulum and its natural ostium. This study didn't register any major complication, such as liquoric fistula. It confirmed a high level of mucosa conservation and a low level of bleeding, which led us to conclude this method is relatively safe and feasible.
During fluoroscopy, patient and surgeon are exposed to ionizing radiation. Aware this radiation brings inherent risks mainly to tissues such as skin, thyroid and eyes, aiming to know whether the level of exposure to radiation is harmful for patients and surgeons, Church CA (9) et al used thermoluminescent dosimeters for the dosage of such radiation. The results showed that both are exposed to very lower dosages than those permissible, considering the prevention of occupational diseases.
Results AnalysisFriedman et al (5) compared a group of patients treated with balloon sinuplasty with a group submitted to FESS. A total of 70 adult patients were evaluated. All patients were submitted to SNOT 20 test (11) before and after the procedure. The results showed a significant improvement in the SNOT 20 in both procedures. As for the patients satisfaction with the interventions; 91.4% answered "yes, they would undergo the procedure again", for sinuplasty, against 48.6% of the patients submitted to FESS. The number of days the patients used analgesic medication was also significantly lower in the patients submitted to sinuplasty (0.80 ± 0.72 days) against FESS patients (1.34 ± 0.99 days; p = 0.011). The expenditures with sinuplasty were of approximately US$ 12,656.57 ± 3,184.08 against US$ 14,471.14 ± 2,743.68 for FESS, and this difference is significant (p = 0.013). The author confirms the sinuplasty and FESS were similar in the postoperative symptoms improvement, however, the sinuplasty obtained a better performance in the patients satisfaction and in the postoperative pain.
Bolger et al (8) carried out a prospective multicentric study to evaluate the balloon sinuplasty in patients with rhinosinusitis without response to clinical treatment and with surgical indication. A total of 115 patients were evaluated and 21 of whom had been submitted to sinusal endoscopic surgery. There were no severe adverse events such as lesion of orbitary tissue, cranial base or bleeding. In 12 of the 358 applications, the appliances had a malfunctioning (balloon break in 7 cases, catheter obstruction by tissue in 4 cases and in 1 case the balloon took long do desinflate). After 24 follow-up weeks, the ostia remained patent in 80.5% of the sinuses, non-patent in 1.6% and indeterminate due to the impossibility of endoscopic viewing in 17.9%; and considering only the ostia which could be viewed, 98% were patent and 2% were obstructed. The revisional treatment was necessary in 3 sinuses of 3 different patients. The SNOT-20 questionnaire showed a significant improvement of the postoperative symptoms.
Levine HL et al (12) carried out a retrospective study of patients submitted to nasosinusal endoscopic surgery with the use of balloon dilation in 27 American services from December 2005 through May 2007, including a total of 1036 patients. Out of whom, 855 (82.5%) had never been submitted to sinusal surgery and 181 (17.5%) were revisional. A total of 3276 sinuses were treated with balloon dilation. These were followed-up on an average of 40.2 weeks after the procedure. No major adverse event regarding the procedure was reported. The average bleeding was of 77.5ml, and it was of 27.7ml in cases where only balloon was used and 101.6ml in the cases combined with FESS. A total of 2.4% of the patients required revision due to the disease's recurrence. They represented 1.3% of the sinuses treated by balloon dilation. As far as the symptoms are concerned, 95.5% of the patients had an improvement. They concluded the balloon dilation is safe, effective and improves the quality of life of patients who didn't have a response to the clinical treatment.
DISCUSSIONWhenever we find a new surgical instrument, we need to evaluate its safety, feasibility, capacity to eliminate the disease and improve the quality of life of the patients. The balloon sinuplasty is an alternative for the minimally invasive treatment of the patients with chronic rhinosinusitis contrary to the exclusive clinical treatment. It doesn't seem to be an alternate to the paranasal sinuses functional surgery, but an option for selected patients. The combined use of the balloon sinuplasty and FESS techniques may be a good option in some cases (2,5,8). The initial approach may be surgical with manipulation of the anterior ethmoidal cells and the osteomeatal complex, and the balloons remain as an alternative for use in the frontal recess and sphenoidal sinus region, for instance.
ICU patients who have a higher anesthetic risk and present with isolated sphenoidal disease may benefit from the use of balloons, since this provides a fast treatment and with low bleeding risk (2-4). The possibility to perform the dilation with local anesthesia is also advantageous in the approach of patients with high anesthetic risk (5). As for the frontal recess region, Vaughan WC (13) reports this area surgery may lead to severe complications relating to the cranial base, anterior ethmoidal artery, olfactory mucosa and periorbitary tissue. In the author's experience, this region is the one which requires more review due to cicatricial stenosis. The large removal of mucosa, edema, infection and incomplete surgery also lead to the disease's recurrence. He mentions one of the main advantages relating to the use of balloon is its potential to a minimally invasive treatment of the frontal recess. The use of balloon combined to the endoscopic surgical approach may minimize the surgical complications relating to the frontal recess. Rehl et al (14) reviewed a series of patients in whom 136 frontal recesses were treated with balloon dilation. Out of 95 recess that could be reevaluated, 99% were patent. Payne SC et al (15) reported the frontal recess dilation of 20 patients with chronic rhinosinusitis. In a follow-up of 5 months, they described the absence of complications and the significant tomographic improvement in the Lund-Mackay score.
As for the risks, these seem to be low, in spite of the possibility of noble structures lesion, such as the cranial orbit and base. To prevent this, Bolger et al (3) reported we should evaluate the structures carefully as the cranial base for dehiscences and also anatomic variations of the ethmoid roof, such as Keros' ranking (16) type III for instance. Brown CL et al (2) also mention the care we must take in patients with Keros type III. They also recommend caution in patients with osseous neoformation signs, because an attempt to dilate may not be efficient and there's the risk, in case we use an exaggerated pressure, it is transmitted to adjacent structures such as the cranial base and orbit. We must also take a lot of care during the procedure to avoid postoperative complications, such as the middle infundibulum lateralization and its adherence with the uncinated process (4,5). In order to prevent such complication the authors suggest the use of absorbable gel in the middle meatus after the procedure. Levine et al (12) reported 3 cases of liquoric fistula in patients submitted to balloon dilation. However they related these events to the endoscopic surgery that was performed simultaneously to dilation.
Church et al CA (9) and Chandra RK (10) demonstrated the radiation dosages to which surgeon and patient are exposed during fluoroscopy are very low. But we must always take care to minimize such exposure as much as possible. Chandra RK (10) advises the surgeons who practice many procedures with the use of fluoroscopy must be encouraged to use specific clothes, goggles and cervical protectors against radiation. He also mentions the left eye of the patient is more exposed to radiation, because the radiation source is normally located as his left side in the lateral incidence.
There are no randomized studies that compare the use of balloon associated with FESS with the separate use of FESS. Such study would be extremely important, since the use of balloon seems to be one more tool to be used simultaneously with FESS and not its alternate therapy.
As far as costs are concerned, Friedman et al (5) showed the expenditures are similar when balloon sinuplasty is compared to FESS. However in the expenditures relating to FESS they take into account the browsing routine use. In the Brazilian reality we know browsing is used eventually and even though generally only in cases of tumors and revisional complicated cases. Therefore, the FESS costs here in Brazil would probably be lower than those mentioned in the study. Moreover, due to the Brazilian taxing, probably the price of the products required for performance of the balloon sinuplasty would be higher.
FINAL COMMENTSThe balloon sinuplasty seems to be a feasible, safe and efficient technology in selected patients. It presents as an auxiliary and complimentary therapy to FESS, mainly in the disease relating to the frontal recess. It also has an excellent perspective in ICU febrile patient with sinusal focus and patients with high anesthetic and bleeding risks. Studies to confirm its cost here in Brazil are still necessary to evaluate its economical feasibility in the Brazilian scenario, as well as randomized studies with high evidence levels that compare its use associated with FESS to the use of FESS separately.
BIBLIOGRAPHICAL REFERENCES1. Stammberger H. Functional endoscopic sinus surgery: the Messerklinger technique. Philadelphia: Decker, 1991:283.
2. Brown CL, Bolger WE. Safety and feasibility of balloon catheter dilation of paranasal sinus ostia: a preliminary investigation. Ann Otol Rhinol Laryngol. 2006, 115(4):293-299.
3. Bolger WE, Vaughan WC. Catheter-based dilation of the sinus ostia: initial safety and feasibility analysis in cadavermodel. Am J Rhinol. 2006, 20:290-294.
4. Friedman M, Schalch P. Functional endoscopic dilatation of the sinuses. Patient selection and surgical technique. Operat Tech Otol. 2006, 17:126-134.
5. Friedman M, Schalch P, Lin HC, Mazloom N, Neidich M, Joseph NJ. Functional endoscopic dilatation of the sinuses: Patient Satisfation, postoperative pain, and cost. Am J Rhinol. 2008, 22(2):204-9.
6. Lund V, Mackay IS. Staging in rhinosinusitus. Rhinology. 1993, 31(4):183-4.
7. Hueman K, Eller R. Reduction of anterior frontal sinus fracture involving the frontal outflow tract using sinuplasty. Otolaryngol Head Neck Surg. 2008, 139:170-171.
8. Bolger WE, et al. Safety and outcomes of balloon catheter sinusotomy: A multicenter 24-week analysis in 115 patients. Otolarygol Head Neck Surg. 2007, 137:10-20.
9. Church CA, Kuhn FA, Mikhail J, Vaughan WC, Weiss RL. Patient and surgeon radiation exposure in balloon catheter sinus ostia dilation. Otolaryngol Head Neck Surg. 2008, 138:187-191.
10. Chandra RK. Estimate of radiation dose to the lens in balloon sinoplasty. Otolaryngol Head Neck Surg. 2007, 137:953-955.
11. Piccirillo JF, Merritt MG, Richards ML. Psychometric and clinimetric validity of the 20-item sino-nasal outcome test (SNOT-20). Otolaryngol Head Neck Surg. 2002, 126:41-47.
12. Levine HL, Sertich II AP, Hoisington DR, Weiss RL, Pritikin J. Multicenter Registry of Balloon Catheter Sinusotomy Outcomes for 1,036 Patients. Ann Otol Rhinol Laryngol. 2008, 117(4):263-270.
13. Vaughan WC. Review of balloon sinuplasty. Curr Opin Head Neck Surg. 2008, 16:2-9.
14. Rehl RM, Vaughan WC. Initial use of baloon dilation in the frontal recess. Proceedings at the Triologic Society Annual Meeting. 2006. Available at http://www.triological.org/pdf/2007COSMProgramSort.pdf.
15. Payne SC, Catalano PJ. Balloon dilation of the frontal recess in patient with chronic frontal sinisitis. Presented at the American Rhinologic Annual Meeting. 2007. Available at http://app.american-rhinologic.org/controller.jsp.
16. Keros P. Uber die praktische beteudung der Niveau-Unter-scheideder lamina cribrosa des ethmoids. In Head and Neck Surgery, Face and Facial Skull, Vol 1. Naumann HH. Philadelphia PA: WB Saunders, 392, 1980.
1. Otorhinolaryngologist. Otorhinolaryngology Preceptor of the Clinical Hospital of the Medicine College of the University of São Paulo, FMUSP Brazil.
2. Doctor's Degree in Otorhinolaryngology. Medicine College of the University of São Paulo, FMUSP, Brazil. Otorhinolaryngology Collaborator of the Rhinology Group of the Otorhinolaryngology of the Clinical Hospital of the Medicine College of the University of São Paulo, FMUSP Brazil.
3. Free Professor. Medicine College of the University of São Paulo, FMUSP, Brazil. Affiliate Professor of the Otorhinolaryngology Clinic Discipline of the Medicine College of the University of São Paulo, FMUSP, Brazil.
Institution: Hospital das Clínicas da Faculdade e Medicina da Universidade de São Paulo. São Paulo / SP - Brazil
Mail address:
Waldir Carreirão Neto
Rua Athur de Azevedo, 142 - Apto. 31
São Paulo / SP - Brazil - Zip code: 05404-000
Fax: (+55 11) 3069-6539
E-mail: carreiraoneto@hotmail.com
Article received on October 19, 2008.
Approved on December 8, 2008.