INTRODUCTION The nasal polyposis has a great impact on the patients' life quality, and brings social and occupational limitations. It affects vitality and the general health, and mental health is more affected than physical health (1).
It presents a worse impact on life quality than when compared to other chronic diseases such as, for instance, rheumatoid arthritis, insulin-dependent diabetes and chronic obstructive pulmonary disease (2).
It is estimate that the incidence in the general population is of about 1 to 4% (3). Without predisposition for sex, it affects preferably middle-aged people.
The main complaints of the patients are usually nasal obstruction, rhinorrhea, posterior discharge, headache, hyposmia/anosmia and coughing (4).
The polyps are generally multiple, non-neoplastic, soft, bright, non-bleeding, translucent, pedunculate and fixed on a base. And it more frequently affects the region of the middle meatus (5).
There are growing evidences that the nasal polyposis represents an immunological and inflammatory response from the host in addition to an initial infection (6).
There is association with non-allergic asthma in about 26% of the patients and association with intolerance to acetylsalicylic acid (AAS) in 36%. There may also be association with other diseases such as cystic fibrosis, allergic fungal sinusitis, Young's syndrome, Churg-Straus's Syndrome and Kartagener's Syndrome (7).
Histologically the disease presents an epithelial damage, with a thick basal membrane, edematous stroma, with reduction of the number of vessels and glands and inflammatory infiltrate predominantly eosinophilic (8).
Most available damages on this theme portraits the American or European reality. The objective of this study is to research characteristics of patients with nasal polyposis in a sample of the Brazilian population.
MATERIAL For this study, we used the review of 50 records of patients followed up in a tertiary hospital, from January 2006 to January 2008.
The patients were asked about the main symptoms, presence or record of asthma, history of intolerance to acetylsalicylic acid and the main signs were verified. The evaluation was also complimented through tomography of the paranasal sinuses.
All patients were treated clinically with topical corticoids for at least 3 months and in some cases with systemic corticoids (09 patients).
All patients were submitted to surgical treatment, with general anesthesia and nasal videoendoscopy. Septoplasty was also carried out (16 patients) when necessary. In seven patients concomitant access to the maxillary sinus was carried out via Caldwell-Luc.
The following variables were analyzed: age, sex, smoking, presence of asthma, presence of AAS intolerance and also the following clinical manifestations? anterior and posterior rhinorrhea, nasal obstruction, hyposmia, breezing and pruritus.
The tomographic evaluation system adopted was Lund-McKay (9) (Table 1).
For statistical analysis the chi-square test was applied with p<0.05).
RESULTS Out of 50 patients evaluated, 28 were male (56%) and 22 were female (44%). The mean age range was of 40.8 years, ranging from 11 to 70 years. Nine patients presented history of asthma, five men and four women. Three patients presented history of intolerance to salicylates, two men and one woman, all with diagnosis of asthma. As for smoking, 17 patients were found who used,on average, 5 cigarettes per day, ten men and seven women.
The main clinical manifestation was nasal obstruction in 100% of the patients, followed of nasal pruritus with 62%, sneezing in 60%, anterior rhinorrhea in 50%, posterior rhinorrhea in 32% and hyposmia/anosmia in 20% of the patients as shown in Graphic 1. There was no significant differences of complaints between men and women (p>0.05).
Other complaints were less frequent, such as headache in 6% of the patients, hypacusis in 4%, halitosis in 2% and snoring in 2% of the patients. 4% of the patients presented with periorbitary cellulitis.
In the asthmatic patients the main clinical findings were of nasal obstruction, anterior rhinorrhea, pruritus, sneezing, posterior rhinorrhea and hyposmia/anosmia, in a decreasing order of frequency.
In those who presented intolerance to salicylates, the main clinical findings were similar to the asthmatic ones.
In the tomographic evaluation, according to Lund-McKay system, the average score was of 10.9. In the tomography of asthmatic patients, the average score was of 17.6. The patients with intolerance to salicylates obtained an average of 21.3 points (Graphic 2).
In all patients the anatomopathological exam showed histological cuts with fragments of mucosa and an epithelialized columnar epithelium, thickening of the basal membrane, lymphoplasmocitary inflammatory infiltrate with edema and vasocongestion, and verified 75% of eosinophilic cells and the remaining predominantly neutrophils.
No statistically significant difference was obtained in the symptoms of the general patients compared to the patients with asthma or AAS intolerance (p>0.05). But there was statistical significance when compared by the Lund-MacKey score (p<0.05).
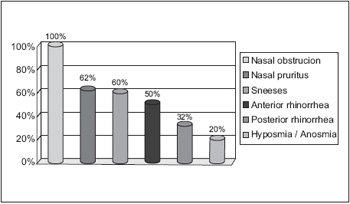
Graphic 1. Clinical manifestations.
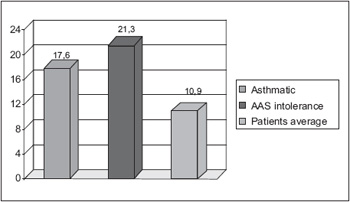
Graphic 2. Lund-McKay tomographic evaluation.
The nasal polyposis is a common disease in the population, with prevalence of about 4% (10). The mean age, at about 40 years, found in our study was similar to that of the studies by Settipane, Larsen and Drake-Lee (11,12,13). Several studies appointed the increased prevalence in men compared to women, which we did not find in our study (7,10,11,12,13).
Despite the recurrence was not evaluated in our study, we believe the patients with asthma and AAS intolerance actually present with a major risk of recurrence after surgery, irrespectively of the treatment performed. (14,15)
In our research, 34% of the patients smoked, in the literature there is not yet a relationship of the role of smoking in the development of the nasal polyposis. (16,17)
The main symptoms found also confirmed other works published, and nasal obstruction was the main symptom (18), obstruction is generally constant, by it may vary depending upon the size and region of the polyps. Some studies also presented a good relationship between the severity of the nasal obstruction with objective tests such as rhinomanometry and nasal peak flow (19,20).
Other symptoms, such as anterior and posterior rhinorrhea, nasal pruritus, anosmia, hyposmia, facial pain, were also frequent, but lower than nasal obstruction, according to other studies (15,16,18).
There was no significant differences between the main complaints of the patients evaluated when compared to patients with AAS intolerance or asthma (p>0.05).
The patients who had asthma or AAS intolerance presented with a major affection of the paranasal sinuses, verified in tomography, which confirmed the data available in the literature (21). The tomography makes a good correlation with the endoscopic findings, but it presents a poor correlation with the symptomatology and is not a good exam for prognosis of the disease (22).
A possible explanation for the most severe case in patients with AAS intolerance is the inhibition on cyclooxygenase-1 enzyme, with a subsequent activation of inflammatory cells and releasing of lipid and non-lipid mediators (24). They also present an increased production of enzymes with leukotrienes. The more asthma is associated with polyposis the more severe is the asthma stage; we believe that polyposis may be due to the air veins remodeling as a consequence of the action of chronic inflammatory processes; then there may occur epithelial hyperplasia, increased deposition of the extracellular matrix, degradation and accumulation of plasmatic proteins, in addition to the lack of suitable repair of chronic lesions (4).
CONCLUSION In our study, we found that the main complaint of the patient with nasal polyposis is still nasal obstruction, and most affected age is 40 years, without prevalence of sex. The severity of the tomographic findings is higher in patients who presented AAS intolerance and asthma.
BIBLIOGRAPHIC REFERENCE 1. Radenne F, Lamblin C, VandezandeLM, Tillie-Leblond I, Darras J, Tonnel AB, ET AL. Quality of life in nasal polyposis. J Allergy Clin Immunol. 1999, 104(1):79-84.
2. Gliklich RE, Metson R. Effect of sinus surgery on quality of life. Otolaryngol Head Neck Surg. 1997, 117(1):12-7.
3. Puwankar R. Nasal Polyposis: An Update. Curr Opin Allergy Immunol 2003, 3:1-6.
4. Revista Brasileira de Otorrinolaringologia, Diretrizes Brasileiras de Rinossinusites (suplemento). 2008, 74 (2):19-20.
5. Bateman ND, Fahy C, Woolford J. Nasal Polyps Still More Questions Than Answers. T J Laring. Otol. 2003, 117(1):1-6.
6. Norlander T, Brönnegard M, Stierna P. The relationship of nasal polyps, infection, and inflammation. Am J Rhinol. 1999, 13 (5):349-355.
7. Settipane GA. Epidemiology of nasal polyps. Allergy Asthma Proc. 1996, 17 (5):231-236.
8. Hellquist HB. Nasal polyps update. Histopathology. Allergy Asthma Proc. 1996, 17 (5): 237-242.
9. Lund VJ, McKay IS. Staging in rhinosinusitis. Rhynology. 1993, 31:183-4.
10. Hedman J, Kaprio J, Poussa T, et al. Prevalence of asthma, aspirin intolerance, nasal polyposis and chronic obstructive pulmonary disease in a population-based study. Int J Epidemiol. 1999, 28:717-22.
11. Settipane G. Epidemiology of nasal polyps. In: Settipane G, Lund VJ, Bernstein JM, Tos M, editor. Nasal polyps: epidemiology, pathogenesis and treatment. Rhode Island: Oceanside Publications; 1997, p. 17-24.
12. Drake-Lee AB, Lowe D, Swanston A, Grace A. Clinical profile and recurrence of nasal polyps. J Laryngol Otol. 1984, 98(8):783-93.
13. Larsen K, Tos M. Clinical course of patients with primary nasal polyps. Acta Otolaryngol. 1994, 114(5):556-9.
14. Caplin I, Haynes JT, Spahn J. Are nasal polyps an allergic phenomenon? Ann Allergy. 1971, 29(12):631-4.
15. Fokkens W, Lund V, Mullol J, et al. European Position Paper Rhinosinusitis and nasal polyps 2007. Rhinology. 2007, 45(20):1-139.
16. ChenY, Dales R, Lin M. The epidemiology of chronic rhinosinusitis in Canadians. Laryngoscope. 2003, 113(7):1199-205.
17. Greisner WA,3rd, Settipane GA. Hereditary factor for nasal polyps. Allergy Asthma Proc. 1996, 17(5): 283-6.
18. Newton JR, Ah-See KW. A review of nasal polyposis. Therapeutics and clinical risk management. 2008, 4 (2) 507-12.
19. Numminen J, Ahtinen M, Huhtala H, Rautiainen M. Comparison of rhinometric measurements methods in intranasal pathology. Rhinology. 2003, 41(2):65-8.
20. Szucs E, Clement PA. Acoustic rhinometry and rhinomanometry in the evaluation of nasal patency of patients with nasal septal deviation. Am J Rhinol. 1998,12(5):345-52.
21. Dalziel K, Stein K, Round A, Garside R, Royle P. Systematic review of endoscopic sinus surgery for nasal polyps. Health Technol Assess. 2003, 7:1-159. Intl. Arch. Otorhinolaryngol., São Paulo, v.13, n.3, p. 259-263, 2009.
22. Browne JP, Hopkins C, Slack R, Topham J, Reeves B, Lund V, et al. Health-related quality of life after polypectomy with and without additional surgery. Laryngoscope. 2006, 116(2):297-302.
23. Fokkens WJ , Lund VJ, Mullol J, et al., European Position Paper on Nasal Polyps. Rhinology. 2007, 45(suppl. 20):1-139.
24. Stevenson DD, Szczeklik A. Clinical and pathologic perspectives on aspirin sensitivity and asthma. J Allergy Clin Immunol. 2006, 118(4):773-86; quiz 87-8.
1. Resident Doctor of the Otorhinolaryngology Service of PUC-SP. Resident Doctor R3 ORL PUC-SP.
2. Resident Doctor of the Otorhinolaryngology Service of PUC-SP. R3 ORL PUC-SP.
3. Resident Doctor of the Otorhinolaryngology Service of PUC-SP. R2 ORL PUC-SP.
4. Head Doctor of the Otorhinolaryngology Service of PUC-SP. Professor in Course for Master's Degree of ORL of PUC-SP.
Institution: Pontifícia Universidade Católica de São Paulo - Hospital Regional de Sorocaba. Sorocaba /SP - Brazil. Mail Address: Dr. Juliano Irita Haro - Rua Dinamarca, 245 Apto. 23 - Jardim Europa - Sorocaba / SP - Brazil - Zip code: 18045-400 - Telephone: (+55 15) 3232-2009 -E-mail: crespo@otoclinica.com.br
Article received on June 8 2009. Approved on July 4 2009.