INTRODUCTION The foreign bodies ingestion is a relatively common diagnosis in the otorhinolaryngology emergency services and occurs mainly in low socioeconomic condition and advanced age individuals due to the use of prosthetic dentistry. About 80-90% of the foreign bodies that reach the gastrointestinal tract will be spontaneously eliminated, 10-20% will need non-surgical interventions and 1% of surgery (1). The complications relating to the foreign bodies ingestion are esophageal perforation, formation of cervical abscess and foreign bodies migration, and they are of low prevalence, but potentially severe (2).
We present a case of retropharyngeal abscess of late evolution after foreign body ingestion.
CASE REPORT Female sex, 56 year old, brown patient seeks the otorhinolaryngology emergency service of the Clinical Hospital of the Medical School of the University of São Paulo (HCFMUSP) with a history of foreign bodies ingestion (fish-bone) for 48 h evolving with odinophagy and cervical pain. A profile neck radiography was carried out in the occasion, and demonstrated a radiopaque foreign body in the cricopharyngeal level (Picture 1) and high digestive endoscopy (HDE) with removal of the foreign body from the pharyngoesophageal segment (Picture 2) and viewing of discreet local laceration. The patient evolved with partial improvement of the dysphagia and neck pain after the procedure, and was discharged with nonsteroidal antiinflammatory and guided as for alert signs.
About one month after, the patient returns to the service reporting a gradual worsening of the dysphagia, pain and antero-posterior left cervical movement, sensation of foreign body in the pharynx, without any episode of fever. Upon physical exam there was a slight difficulty for cervical movement and loss of laryngeal crepitation. A blood count was then collected with 4930 leukocytes without left deviation, a radiography of the neck in profile was carried out and showed an enlargement of the prevertebral soft tissues and a loss of the cervical lordosis (Picture 3). Then we requested a computed tomography (CT) of neck that confirmed a multiloculated collection with intense peripheral enhancement after injection of contrast and with a small amount of internal liquid occupying the left medial and paramedial retropharyngeal region (Picture 4).
With such findings, antibiotic therapy was introduced with cephtriaxone and clyndamicine, hydrocortisone and the surgical approach was chosen for draining of the abscess, via suspension laryngoscopy. During the procedure a convexity of the posterior wall of the pharynx was viewed, from the height of the arytenoids up to some millimeters upwards the pharyngoesophageal transition, and a longitudinal section of the mucosa was carried out with outflow of purulent secretion in a small amount, followed by the passage of the nasogastric probe (NGP). In the material forwarded for culture, there was a growth of negative Staphylococcus coagulase and Streptococcus bovis.
The patient evolved with clinical and laboratorial improvement, with control CT in the 6th postoperative day without collections or edema, and was discharged on the 8th postoperative day with oral feeding.

Picture 1. Radiography of the neck in profile demonstrating a radiopaque foreign body impacted on level of M. cricopharyngeal.

Picture 2. Foreign body removed by endoscopy.

Picture 3. Radiography of the neck in profile showing enlargement of prevertebral soft tissues and loss of the cervical lordosis.
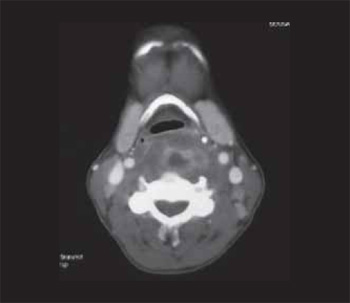
Picture 4. Computed tomography of neck confirming a multiloculated collection occupying the left medial and paramedial retropharyngeal region.
Infections that affect the retropharyngeal space may be generated by contiguity or be secondary to penetrating trauma. In the first case, there may occur suppuration of retropharyngeal lymph nodes that drain upper airways infections or extension from the affection of other cervical spaces. In the second way, the infection is secondary to a penetrating trauma, that may be a foreign body ingestion and even a iatrogenic body after high digestive endoscopy (HDE), orotracheal intubation, laryngoscopy and passage of the nasogastric probe (NGP) (3).
By taking as a complication the development of cervical abscess, esophageal perforation and the need for surgical approach, LAI et al found as predictive factors of complications after foreign bodies ingestion the presence of more than two days of history, the viewing of the foreign body in the radiography of the neck profile and the presence of foreign body with impact on cricopharyngeal and upper esophagus (due to a higher risk of perforation) (2).
The computed tomography presents a high sensitivity and specificity both for the location of the foreign body and to evaluate the presence of possible complications (4,5,6).
According to CIRIZA et al the immediate installation of symptoms after ingestion of a foreign body, dysphagia and absence of pharyngeal location were predictive factors foreign body finding with impact on the EDA (1).
In the case reported, the long period of time observed between the ingestion of the foreign body and the manifestation of the retropharyngeal abscess draws attention. It is possible that a small fragment of the foreign body has remained in the retropharyngeal tissues after removal of its major portion, which caused local abscess. Other studies report the late occurrence of retropharyngeal abscess after ingestion of biologically less active foreign bodies, such as glass (7,8). The abscess remained limited and with little systemic manifestations, such as fever and leukocytosis, which is another important aspect of the case reported. The surgical draining may have allowed the nonidentified extrusion of this fragment and the resolution of the picture.
FINAL COMMENTS The retropharyngeal abscess may occur several weeks after foreign bodies ingestion. The absence of fever and leukocytosis does not exclude the diagnosis even in immunocompetent patients. A high level of suspicion leads to the performance of suitable diagnostic exams and procedure.
BIBLIOGRAPHIC REFERENCES 1. Ciriza C, García L, Suárez P, Jiménez C, Romero MJ, Urquiza O, Dajil S. What predicitve parameters best indicate the need for emergent gastrintestinal endoscopy after foreign body ingestion? J Clin Gastroenterology. 2000, 31(1):23-28.
2. Lai ATY, Chow TL, Lee DTY, Kwok SPY. Risk factors predicting the development of complications after foreign body ingestion. Br J Surg. 2003, 90:1531-1535.
3. Sennes LU, Tsuji DH, Imamura R, Angélico Junior FV. Head and Neck Space Infections: A prospective study. Otolaryngol Head Neck Surg. 2000, 123(2):255-256.
4. Lue AJ, Fang WD, Manolidis S. Use of plain radiography and computed tomography to identify fish bone foreign bodies. Otolaryngol Head and Neck Surg. 2000, 123(4):435-438.
5. Palme CE, Lowinger D, Petersen AJ. Fish Bones at the Cricopharyngeus: A Comparison of Plain-Film Radiology and Computed Tomography. Laryngoscope. 1999, 109(12):1955-1958.
6. Frizzarini R, Wiikmann C, Imamura R, Tsuji DH, Sennes LU. Achados Radiológicos de Corpo Estranho de Esôfago. Limitação da Radiografia Simples para o Diagnóstico Diferencial com Abscesso Retrofaríngeo. Int Arch Otorhinolaryngol., 2003, 7(4):254.
7. Allotey J, Duncan H, Williams H. Mediastinitis and retropharyngeal abscess following delayed diagnosis of glass ingestion. Emerg Med J. 2006, 23(2):e12.
8. Woolley SL, Smith DR. History of possible foreign body ingestion in children: dont forget the rarities. Eur J Emerg Med. 2005, 12(6):312-6.
1. Medical Doctor. Otorhinolaryngology Third-year resident at the Clinical Hospital of the Medical School of the University of São Paulo.
2. PhD. Assistant Doctor at the Clinical Hospital of the Medical School of the University of São Paulo.
3. PhD. Collaborator Professor of the Otorhinolaryngology Discipline at University of São Paulo Assistant Doctor at the Clinical Hospital of the Medical School of the University of São Paulo.
Institution: Departamento de Otorrinolaringologia do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo. São Paulo / SP - Brazil. Mail Address: Henrique Faria Ramos - Rua Dr. Enéas Carvalho de Aguiar, 255 - Secretaria do Departamento de Otorrinolaringologia - São Paulo / SP - Brazil - Brazil: 05403-000 - Telephone: (+55 11) 3088-0299 - E-mail: henriquefariaramos@terra.com.br
Article received on August 30, 2008. Article accepted on March 5, 2009.