INTRODUCTIONEndoscopic surgery has gained universal acceptance for the treatment of inflammatory sinonasal disease. With increasing familiarity with endoscopic techniques and instrumentation and with the help of image-guided systems, one can extend the use of these techniques to more inaccessible paranasal spaces (1-2).
For example, tumors of the pterygopalatine fossa (PPF) which are difficult to remove because of limited access to this region and the rich vasculonervous contents of it allowing only external large-scale procedure for complete remove.
Because of poor specific symptomatology, these tumors can be very big at diagnosis time and can involve the skull base structures.
Here we will describe a strictly endoscopic transnasal approach to the pterygopalatine fossa.
With the help of computer-assisted surgery we respected the intracranial structures with minimal morbidity for the patient. These approaches allow good visualization of difficult-to-access areas with decreased morbidity and shorter recovery periods.
CASE REPORTA 33-year-old woman was referred to our center for evaluation of a right PPF mass, first presumed to be a nasopharyngeal fibroma, on the basis of radiological data.
The patient suffered for several years of facial pain and nasal obstruction with no other symptoms. She used a lot of antalgic drugs. First of all she had refused surgery because only an external approach (paralateronasal) has been proposed to her. In 2002 she was treated by radiotherapy with no success. Then the mass was followed during a period of three years by magnetic resonance imaging: it became bigger and more painful.
When referred to our center, the patient accepted the option of an endoscopic surgical excision; she was counseled regarding the risk of a possible need to convert to an open approach if the removal can not be complete.
- MRI: showed a right PPF tumor of 5 cm with extension: to the maxillary sinus through the posterior wall, to the sphenoidal sinus, to the nasal fossa with destruction of the middle and inferior turbinate. It also showed an intimate contact with the orbital apex and the optic nerve; and an extension to the skull base with an erosion of the cavernous sinus (Figure 1A).
- Arteriography: the mass had a poor vascularisation but for safety reasons we proceeded to a pre-operative embolisation of the facial and internal maxillary arteries.
- Surgical procedure: image guidance helped us for rapid localisation of intracranial structures and limits of the tumor. The split screen format allows simultaneous visualization of the PPF tumor from axial, coronal and sagittal views, as well as the lesion itself by the way of endoscopy (Figure 2 A).
After skin surface registration method and validation of the calibration by pointing on anatomical landmarks, the procedure was begun with a large maxillary antrostomy and ethmoidectomy, the sphenoidal sinus was already invaded. To expose the medial and anterior aspects of the tumor the thinned posterior wall of the maxillary sinus was easily removed, then we saw a large friable yellow tumor with a capsule (extemporaneous analysis: schwannoma).
Because of the tight confines of the PPF and the attachments of the tumor, this one could not be removed in one piece; the capsule was there for opened to allow complete removal of the tumor progressively with special attention to the region of the optic nerve and cavernous sinus (Figure 2 B).
- Recovery period: after surgery the patient was totally free of pain, she had no visual sequela, no trigeminal territory dysesthesia, and neither cerebrospinal fluid leak. She left the hospital after one week. The anatomopathologic result revealed a benign schwannoma.
- Control: An MRI made 4 months after surgery showed no recurrence. The patient was followed regularly by nasal endoscopy: three years later the cavity is free of tumoral recurrence even with the capsule left in place (3) Figure 1B.
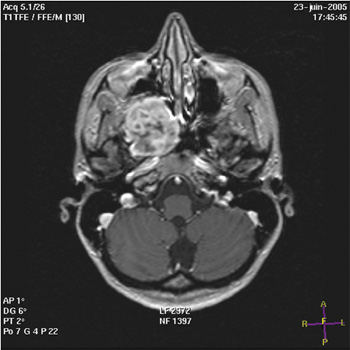
Figure 1A. MRI: situation before surgery showing a large tumor (diameter: 5 cm) arising from the pterygopalatine fossa and extending to the temporal bone and cavernous sinus.
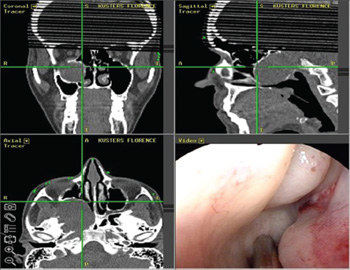
Figure 2A. Image guidance helps for rapid localization of the limits of the tumor. We can see the extension of the tumor through the maxillary sinus, partial destruction of the middle and the inferior turbinate; intimate contact with the orbital apex.
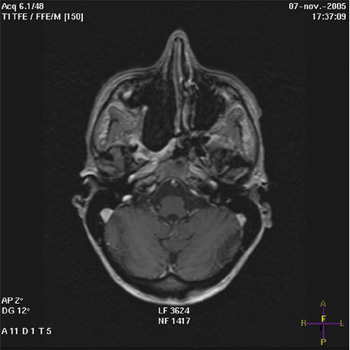
Figure 1B. MRI: 4 months after surgery: the cavity is free of tumoral recurrence; we see the capsule left in place.
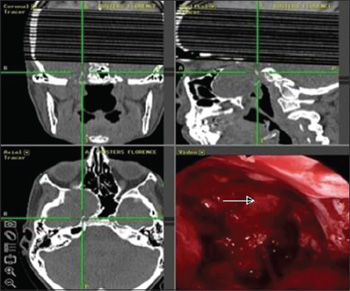
Figure 2B. Computer-assisted surgery shows that we have an intimate contact with the cavernous sinus (arrow).
The PPF is one of the subregions of the infratemporal fossa (ITF) and a difficult to access anatomic area. It is located behind the posterior wall of the maxillary sinus, bordered by the pterygoid plates posteriorly and the greater sphenoid wing and middle cranial fossa superiorly (4).
It has connections with the infratemporal fossa laterally through the pterygomaxillary fissure, the posterior nasal cavity medially through the sphenopalatine foramen, the orbit superiorly through the inferior orbital fissure, and the skull base structures through the foramen rotundum. Structures contained within the PPF include the internal maxillary artery and its branches, the maxillary division of the trigeminal nerve and the vidian nerve (4-5).
It is because of all this complicated anatomic relations that standard approaches to the PPF require large scale external procedure, and even in the better cases there are a lot of complications. The most common procedures: transmaxillary, transzygomatic and transmandibullary techniques violate the anterior and posterior walls of the maxillary sinus with the risks of facial edema and pain, infraorbital nerve injury, oroantral fistula, chronic sinusitis and vascular injury (5).
Endoscopic approach potentially reduces these risks and provides better visualisation.
PPF is rarely the site for primary disease; generally the tumors arise from the ITF and extend to the PPF (3-4).
We only found 4 reported cases of endoscopic resection of PPF tumors, all of which were schwannomas, only 3 were completely resected. None of them had an intracranial extension. In fact all authors conclude that endoscopic surgery has been possible because of no extension to the skull base (Table 1).
But with the help of computer-assisted-surgery (CAS), we could resect the all tumor even with an intracranial extension. In fact CAS has an accuracy of 1 to 2 mm, and this enables the surgeon to have a more thorough understanding of the complicated anatomy of paranasal spaces. It is also helpful when normal anatomic landmarks are lacking. Of course the skin surface registration must be reliable and must allow patient head movement during the procedure.
For the PPF three endoscopic approaches are possible:
- Transpalatine: first identify the sphenopalatine foramen, proceed to artery ligation then remove the posterior wall of the maxillary sinus. This technique provides a good medial view and is suitable for small tumors.
- Transantral: first proceed to a large antrostomy and ethmoidectomy then remove the posterior wall of maxillary sinus. This technique provides a good lateral view.
- Transturbinal: first proceed to an inferior turbinectomy followed by an antrostomy, and then remove the posterior wall of the maxillary sinus. This technique provides the widest view for maneuvering in the medial and lateral compartments of the PPF and infratemporal fossa.
By the way we think that all these approaches are safer if they are preceded by an embolisation of the mass vascularisation.
CONCLUSIONTransnasal endoscopic surgery is a good solution to approach the PPF, when vascular danger has been excluded.
This technique allows a good visualisation of the region with decreased morbidity and shorter recovery period.
With the help of CAS the surgeon has a more thorough understanding of the complicated anatomy of the paranasal spaces, and can explore more easily the skull base with minimal risks.
In our case the computer-assisted-transnasal endoscopic surgery allowed us to resect completely a large tumor of the PPF and his intracranial extensions with no complications.
REFERENCES1. Mann W, Klimek L. Indications for computer-assisted surgery in otorhinolaryngology. Comput Aided Surg. 1998, 3:202-4.
2. Parikh SR, Fried MP. Navigational systems for sinus surgery: new developments. J Otolaryngol. 2002, 31 Suppl 1:24-7.
3. Klossek JM, Ferrie JC, Goujon JM. Pranasal schwannomas. Ann Oto-laryngol. 1993, 110:341-5.
4. Aronsohn M, Stringer S, Brown H. Utility of image guided surgery in the diagnosis of pterygopalatine fossa lesions. The Laryngoscope. 2004, 114:424-7.
5. Delgaudio JM. Endoscopic transnasal approach to the pterygopalatine fossa. Arch Otolaryngol Head Neck Surg. 2003, 129:441-6.
6. Martinez Ferreras A, Rodrigo Tapia JP, Llorente Pendas JL et al. Endoscopic nasal surgery for pterygopalatine fossa schwannoma. Acta Otorhinolaryngol Esp. 2005, 56:41-3.
7. Pasquini E, Sciarretta V, Farneti G et al. Endoscopic endonasal approach for the treatment of benign schwannoma of the sinonasal tract and pterygopalatine fossa. Am J Rhinol. 2002, 16:113-8.
1. Doctor (ENT and Head and Neck Surgeon).
2. Doctor (Radiologist).
3. Professor (Neurosurgeon).
4. Doctor (Ent and Head and Neck Surgeon).
5. Professor (Ent and Head and Neck Surgeon).
Intitution: Department of Otorhinolaryngology & Head and Neck Surgery, Erasme Hospital. Brussels, Belgium. Mail Address: Dr. R. Ghanooni - Department of Otorhinolaryngology & Head and Neck Surgery - Erasme Hospital - Route de Lennik 808, 1070 - Brussels - Belgium - Telephone: 003225554632 - Fax: 003225556826 - E-mail: rosemaryam_ghanooni@yahoo.fr. Article received November 15, 2008. Article approved May 27, 2009.