INTRODUCTIONThe cleft lip and palate (CLP) is one of the most common congenital malformations in the human race, it is caused by lack of fusion of the embryonic facial processes. The anatomic impairment appears as a cleft lip and / or palate, and it may occur with a frequency of 1:700 births (MURRAY, 2002). In Brazil it is estimated that between the CLP reaches 1.24 and 1.54 per 1000 live births (NAGEM FILHO et al, 1968; FRANÇA & LOCKS, 2003, NUNES et al, 2007). Surgical repair of primary cleft palate and / or so-called soft palatoplasty is a surgical procedure for anatomical and functional reconstruction of this structure (BERTIER & TRINDADE, 2007; KUMMER, 2001a).
There are numbers of techniques for palatoplasty, in which surgeons choose their approach, according to its received notions and experience (SHPRINTZEN & BARDACH, 1995). In the Service of Plastic Surgery Craniomaxillofacial of HCPA it was used for many years the VW-K + B technique in practically all cases. This technique uses the concepts of VY palatoplasty in order to obtain a good stretch of the anteroposterior palate, along with the basis on the intravelar veloplasty (posterior muscle) from BRAITHWAITE (1964), which provides the reorganization of the whole muscle of the soft palate. In the middle of 2003 the staff switched to a modification of the V-W-K + B called V-W-K + B + Z (Veau-Wardill-Kilner+ Braithwaite+Zetaplasty). This hybrid technique uses the concepts of V-Y palatoplasty in order to obtain a good stretch of the anteroposterior palate, which is complemented by the notions of intravelar veloplasty (posterior muscle) from BRAITHWAITE (1964), promoting the reorganization of the whole muscle of the soft palate . To stretch the nasal mucosa, it was used the Z-plasty, which is characterized by the transposition of two scissorings with triangular shapes (FROES FILHO, 2003). FURLOW idealized palatoplasty through the double reverse zetaplasty that takes place on the posterior palate, one in the oral mucosa of the soft palate and the other with reverse orientation, in the nasal mucosa of the soft palate with retropositioning of hoist posterior muscles of the palate (BERTIER & TRINDADE, 2007; FURLOW, 1986, D'ANTONIO et al 2000).
The main goal of palatoplasty is not only restoring the anatomy of the palate (LEOW & LO, 2008), but also promote an adequate velopharyngeal function that consequently provides conditions for the production of speech without changes (PEGORARO-KROOK et al, 2004). However, many times even after the patient has palatoplasty, the ladder presentas the velopharyngeal function changed, which settles the presence of harmful symptoms to the speech. The most common symptoms are hypernasality, the nasal air escape and compensatory articulation disorder (D'ANTONIO & SCHERER, 1995; TRINDADE & TRINDADE, 1996; ALTMANN, 1997; KUMMER, 2001a; GENARO et al, 2007).
Methods of evaluation of the velopharyngeal function can be divided into direct and indirect. Direct methods allow the evaluator to visualize the structures in velopharyngeal closure, as well, to observe how these structures move in the swallowing, speech and others other functions. On the other hand, there are indirect assessments which provide data on the functional outcomes of velopharyngeal activity, which allow experts to make inferences about the appropriation or otherwise of velopharyngeal function (GENARO et al, 2004; TRINDADE ET al, 2007).
The perceptual evaluation is used as a method for initial evaluation by the majority of physicians who investigate the velopharyngeal function. It is an indirect method, because it is considered that the human ear is a "tool" and the perceptual spread of velopharyngeal function are used to make inferences about the velopharyngeal mechanism. The hearing trial indicates the clinical relevance of the signs of velopharyngeal dysfunction for both for the speaker as the listener. Moreover, it contributes to the diagnosis along with information from clinical history, physical examination and instrumental of the patient (PEGORARO-KROOK, 1995; TRINDADE & TRINDADE, 1996; SELL et al, 1999; KUMMER, 2001a; SHPRINTZEN, 2005). However, for diagnosis, therapeutic procedure, and also get the functional results of the surgical technique of the palate reconstruction, it is necessary, at least, to carry out an evaluation among the many available tools. The videonasoendoscopy is one the most common used tests in clinical practice, and allows physicians to investigate the nature, extent of the problem in the structures and functions of the velopharyngeal mechanism. In this, it is possible to observe the patterns of closure (or even, the best attempt of occlusion) of the EVF including speech with specific features and degree of movement of the soft palate and pharyngeal walls (WILLIAMS, 1998; KUEHN & HENNE, 2003; SHPRINTZEN, 2004; TRINDADE et al, 2007; PEGORARO-KROOK et al, 2008, AMERICAN CLEFT PALATE-CRANIOFACIAL ASSOCIATION, 2007; BZOCH, 2004; GENARO et al, 2007; LESSA, 1996).
Some researchers consider the speech performance of individuals with cleft lip and palate, as a pattern to analyze the advantages and disadvantages of one or more of palatoplasty techniques (DREYER & TRIER, 1984, HARDIN-JONES, 1993; SCHÖNWEILER et al, 1999, WILLIAMS et al, 1999; MARRINAN et al, 1998; NAKAJIMA et al, 2001; BAE et al, 2002; VAN LIERDE et al, 2004; POLZER et al, 2006; HASSAN & ASKAR, 2007; KOSHLA et al, 2008). The speech results of these patients in different palatoplasty techniques are issues that arouse interest of surgeons who perform the procedure, in addition to other professionals who work treating these patients (VAN LIERDE et al, 2004; SHPRINTZEN & BARDACH, 1995).
There are studies that compare the different techniques of palatoplasty though features of speech, although it is known that there are many factors that contribute to the failure of the primary palatoplasty related to speech. In some cases, it is possible to observe the short veil, a greater variability in amount of the muscle mass; interference of the insertion of hoist muscle and anatomical alterations in the pharyngeal walls (NAKAMURA et al, 2003). Other factors may also contribute to the results, as the influence of the surgeon's experience (WITT et al, 1998; GOMES & MÉLEGA, 2005, WILLIAMS et al, 1999); interference of speech therapy (HARDIN-JONES, 1993; KHOSLA et al, 2008); surgical technique of the palate and the type and extent of cleft lip and / or palate (KRAUSE, et al 1976, VAN DEMARK & HARDIN, 1985; MCWILLIAMS et al, 1990; FROES FILHO, 2003).
It was found no studies investigating the different palatoplasty techniques and its clinical results in the current literature. However, there are few studies in the current literature that attempt to control most of the already known facts, which might influence the palatoplasty results, such as, a single surgeon perform all primary palatoplasty in one or more techniques; influence of speech therapy, and especially, the homogeneity of the sample characterized by morphometrical measurements of the palate in the same type of cleft.
This study aimed to compare the results of instrumental and perceptual evaluations of patients with unilateral cleft lip and palate operated by three different palatoplasty techniques.
METHODSDesign: a transversum prospective study for perceptual and instrumental evaluations, in patients with cleft lip and palate underwent to a randomized clinical trial, using three different techniques of palatoplasty between 2000 and 2001, performed by a single surgeon.
Sample: The sample consisted of the same participants in the research developed by Fróes Filho (2003), which had 30 children with complete unilateral cleft lip and palate, with similar morphometrical characteristics, showing no syndromical changes, not undergoing to previous surgeries on the palate.
The sample had been divided into 3 groups of 10 patients who underwent to primary palatoplasty between 12 and 24 months old, by a single surgeon with experience in the three palatoplasty techniques. The choice of surgical procedure applied to each patient was a raffle, conducted by a member of the surgical staff, without the surgeon's previous knowledge. On each group was carried out one of the three surgical techniques whicho were compared: the Furlow technique, the Veau-Wardill-Kilner + Braithwaite (V-W-K + B) technique, and the technique proposed by the author, originally called the V-W- K+B+Z (FRÓES FILHO, 2003).
All the participants in the sample had the same type of cleft. To examine the homogeneity of the sample, it was performed a measurement of the fixed points of the hard palate (longitudinal dimension of the palate, cleft bone width and transverse dimension of the palate) illustrated in Figure 1. After this procedure, it was examined that in this sample, the palate did not differ in the anthropometric point of view. Thus, it was found no significant differences in the size of the cleft, in the cleft width and the miomucosa cleft. Patients were located by a searching the medical records held by the surgeon and gotten in touch by mail or telephone. In order to make easier the reading of the symbols listed below, it had been established the terminology for each one. Besides, it was included the number of evaluated individuals, a total of 26 people.
Group 1: 10 participants underwent to the Furlow's technique:
F TECHNIQUE
Group 2: 7 participants underwent to the Veau-WARDIL-Kilner techinique with veloplasty, that is, Veau-Wardil-Kilner + Braithwaite (V-W-K+B):
V-W-K+B TECHNIQUE
Group 3: 9 participants underwent to the V-W-K+B+Z:
Z NASAL TECHNIQUE
Inclusion criteria
The participants of this study are all from a group of patients who underwent to one of the three techniques of palatoplasty by the same surgeon.
Exclusion Criteria
Participants or guardians who have not authorized their inclusion in the study through the Term of Free and Enlight Consent (TFEC-ANNEXE 1); who did not cooperate in the examination for evaluation of the velopharyngeal sphincter. We also excluded people with choanal atresia, nasal septum deviation or other important anatomical obstructions that prevented the examination. And also that they had been undergone to secondary palatoplasty.
Ratings
Patients underwent to two evaluations, one perceptual and one instrumental, besides a brief interview with the responsible family member about the patient's medical history and if he or she had undergone to some speech therapy. The first evaluation was by recording a sample of the patients speech saying two sentences in Portuguese with plosive phonemes and fricative phonemes: Plosive, "Papai pediu Pipoca" ("Daddy asked for popcorn) and fricative, "O Saci sabe assobiar" (Saci knows how to whistle), besides a count from one to ten. The second evaluation took place because of a videonasoendoscopy, in which the patient emitted the sound of the phoneme / s / continuously. Both procedures were evaluated separately, by three evaluators blinded to the type of surgical technique. Besides, an otorhinolaryngologist examined the tonsils and the adenoids, according to BRODSKY (1989) and WORMALD and PRESCOTT (1992) respectively. In perceptual assessment evaluators should consider the presence or absence of hypernasality and if this rate your second degree severity scale of HENNINGSSON (2008) adapted, presence or absence of audible nasal air emission (EANA) and compensatory articulation disorder (DAC). Beforehand in videonaso-endoscopy, evaluators should have to estimate clinically the size of the Velopharyngeal Sphincter gap (VFS) through the severity scale proposed by GOLDING-KUSHNER et al (1990) and LAM et al (2006) in an adapted form. This has a score that represent has its minimum value, 0.0 (zero) which is visually considered by the opening area of the VFS at rest during nasal inhale, that is, it represents the residual position or absence of movement. The maximum score is 1.0, which represents complete closure and the maximum possible movement of the VFS. Comparing to the opening area of the VFS at rest and during speech, it is possible to obtain the closure or residual gap, in which will be observed or not a residual opening of the velopharyngeal sphincter, when it is supposed to be completely closed. After the database creation, it was classified in a gathered way, a clinical computation of the size of the gap in 5 categories, according to GOLDING-KUSHNER et al (1990) and LAM et al. (2006), in an adapted form, it was possible to visualize in Figure 2. To compose this record, two important aspects were considered in image analysis: one is the gap and the other, the VFS closure quality. Scale adapted from LAM et al (2006) and GOLDING-KUSHNER et al (1990)
0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0
1.0 (no gap, complete closure)
0.8-0.9 (small gap, efficient closure)
0.4-0.7 (average gap, intermediate closure)
0.1-0.3 (large gap, inefficient closure)
0 (very large gap, lack of closure)
Statistical analysis
To statistical analysis was calculated using the frequency and percentage of all variable of this study.
For clinical estimate of the size of the VFS gap in the instrumental for the perceptual assessment as for perceptual assessment of speech (hypernasality, CAD, ANAE) was performed in agreement with the judgments of the three evaluators about the total sample. As there was an agreement with the Kappa test, the assessment of one of the evaluators was used as reference for data analysis.
To evaluate the difference between the techniques regarding to the perceptual assessment to mention the presence or absence of: hypernasality, Compensatory Articulation Disorder and Audible nasal air emission, were applied to the Fisher's Exact Test. In what applies to hypernasality, it was used the Kruskal-Wallis Test. In what refers to the instrumental assessment in the clinical computation of the size of the gap, it was also used the Kruskal-Wallis Test. Data were analyzed in the SPSS 14.0 software and the level of significance was set at 5%.
Herewith the size of the original sample, it would be possible to detect absolute differences of around 60% in the variables between the techniques, with 80% power and level of significance of 0.05.
Ethical Aspects
The present study was conducted at Hospital de Clinicas de Porto Alegre and was approved by the Ethics Committee of the same institution by the number 04-433. Wherein all parents or responsible relatives signed the Term of Free and Enlighten Consent.
RESULTSA total of 26 individuals, in which 10 of the F Technique (10/10), 7 of the V-W-K+B Technique (07/10) and 9 of the Z nasal technique (9/10).
With regards to age when the palatoplasty was performed, the participants were between the one and two years old. The current age of patients ranged between 8 and 10 years old. There was no statistically significant difference between the techniques regarding the age at the time of the surgery (p = 0.156) and current age
(p = 0.427).
The percentage of males and females was similar between groups. In all three techniques, the majority of the sample belonged to the male, with no statistically significant difference between techniques (p = 0.280).
Statistical analysis was performed to verify the possible influence of the size of the tonsils, adenoids, speech therapy among the groups of the sample, besides the goals proposed by this study.
For the three groups, the classification of the tonsils prevailed in degree I and II, none referred to degree III and IV. Regarding to the adenoids, in all groups the vast majority was in degree I. Comparing the classification of the tonsils (p = 0.804) and the adenoids (p = 0.482) among the techniques, there was no statistically significant difference.
Throughout the study, it was identified only one individual who underwent to the Furlow's technique with a small fistula in the soft palate, with no statistically significant difference between techniques (p = 0.435).
For the participants who had speech therapy, it was only identified one participant belonging to the group "Z nasal technique". This participant underwent treatment to change in nasality and articulation of speech disorder since he or she was 3 years to about 6 years once a week. After this period, he or she had speech therapy once a month. The remaining participants did not undergo speech therapy until the assessments. Thereby, there was no new statistically significant difference. In the four investigated items and considered as possible disorder factors (tonsils, adenoids, fistula and speech therapy) it was not found statistically significant differences among the groups.
In the perceptual assessment regarding to hypernasality and other features of the speech samples, were obtained from the inter-judging correlation through the Kappa coefficient of agreement by matching the findings of one evaluator with the other two which resulted in three pairs (1 and 2; 1 and 3; 2 and 3). The coefficients of inter-rater and inter-observer variability is a measure of agreement / disagreement among different raters. In this study, the interpretation of Kappa coefficients FLEISS (1973) was performed as proposed by LANDIS AND KOCH (1977), as follows: lower than 0.00 which do not indicate agreement; from 0.00 to 0.20 indicates little agreement; from 0.21 to 0.40 indicates regular agreement; from 0.41 to 0.60 indicates moderate agreement; from 0.61 to 0.80 indicates substantial agreement; from 0.81 to 1.00 indicates perfect agreement (or almost perfect).
As in sentences as on numbers countdown, it was obtained from substantial agreement to almost perfect. The comparison of hypernasality and other aspects (DAC and ANAE) judged the perceptual assessment of speech samples among palatoplasty techniques are presented in Tables 1, 2 and 3. It was found few differences between the two sentences and the segment of connected speech (numbers countdown) as much as the hypernasality, DAC and ANAE. This data shows that regardless of the prevalence of phonemes and connected speech segment, there is no significant change in the evaluators' judgement or the comparison between the techniques.
In the instrumental assessment as much as the clinical estimate of the size of VFS's Gap, it was obtained with inter-judging an agreement by the Kappa coefficient by matching the findings of an evaluator on each of the other two which resulted in three pairs (1 and 2; 1 and 3; 2 and 3) the same way as in the hypernasality assessment, CAD and ANAE. On table 4, it is possible to observe that among the evaluators 1 and 2 and 2 and 3 the agreement is substantial, as among judges 1 and 2 indicates almost perfect agreement.
The classification of the clinical estimate of the size of the velopharyngeal sphincter gap on the three techniques (F, V-W-K + B, Z NASAL) is illustrated in Figure 6. It was considered without gap in the complete closure of the VFS, small gap in the effective closure, average gap in intermediate closure, large gap in inefficient closure, very large in the absence of closure.
Although there is no statistically significant difference as regards to the classification of the estimate clinical size of the VFS Gap among the three types of techniques, it is possible to observe in figure that the highest proportion of children without the orifice, that is, with total closure of the VFS, it was found in the Znasal technique. Regarding to the large orifice that corresponds to a inefficient closure of the VFS, it was found only two participants who underwent to the V-W-K+B technique. In the classification, a very large orifice corresponds to the absence of closure of VFS and it was not found in any of the participants among the three techniques.
DISCUSSIONPalatoplasty can be considered the basis for the treatment of patients with cleft lip and palate, because among many procedures and assessments in various multidisciplinary areas, only after the reconstruction of the palate it is possible the relocation and restoration of the velopharyngeal sphincter physiology.
The variety of techniques employed in palatoplasty has considerably grown since ancient times until the new millennium. The challenge in the art of modern palatoplasty is not only the successful closure of the cleft in the soft and/ or hard palate, but achieving an excellent speech result without compromising the maxillofacial growth (LEOW & LO, 2008).
The VPD, in other words, the impairment of velopharyngeal closure may remain even after surgical repair of the palate and therefore lead to a change in resonance making speech impaired (AMARAL & GENARO, 1996). The hypernasality and nasal air emission are some of the symptoms present in the speech that may be associated with VFD (TROST-CARDAMONE, 2004). In addition, compensatory articulation disorders occur in an attempt to compensate for the VFD.
This study aimed to compare three techniques of palatoplasty, by two evaluations, one perceptual and one instrumental, providing functional data of the VFS, in what regards to speech. The literature offers a variety of information regarding the physiology of the velopharyngeal mechanism in several professional areas (ALTMANN & LEDERMAN, 1990, PULKKINEN et al, 2002). However, it is important to highlight that studies that attempt to compare techniques of palatoplasty by using functional results differ. There is little research that consider in the same study: 1) the sample (the same type of cleft and morphometric characteristics; individuals not taken by neurological problems); 2) clinical assessment protocols and instruments proclaimed in the literature; 3) only one surgeon involved; 4) a skillful surgeon in the investigated techniques; 5) agreement among evaluators; 6) the possible confounding variables (influence of the tonsils, the adenoids, the speech therapy on velopharyngeal function).
Even though the subject is not the focus of the study, it is worth mentioning that the age of the patients during the evaluations was between 8 and 10 years. Regarding specifically to instrumental assessment, individuals in this age group can already collaborate in the exam, allowing a proper assessment of the velopharyngeal functional musculature (CARVALHAL, 2003; KRUSE, 2005, SILVA, 2008). Regarding to the perceptual assessment at this age, children should have already acquired all the speech sounds (CANO & NAVARRO, 2007). Therefore, the age of the sample was suitable to conduct evaluations. As much as this subject did not belong to the purposes of the study, it is appropriate to consider an investigation of the patients' hearing. For this, they were all referred to a specialist.
The perceptual assessment has great clinical relevance, it is an essential part in the diagnosis of VPD, along with the patient's physical / instrumental and clinical history. There are many researchers that propose the use of specific protocols for evaluation of speech in cleft individuals (PEGORARO-KROOK, 1995; TRINDADE & TRINDADE, 1996; SELL et al, 1999; KUMMER, 2001b; SHPRINTZEN, 2005). It was decided for an adapt to the protocol proposed by HENNINGSSON et al (2008), because besides providing instructions on the phonetic composition of the sample of speech and its record, it also provides a severity rating and descriptors related to hypernasality.
Regarding to the details of the perceptual assessment, that is, the steps that followed the criteria established by the literature. First, it took the precaution in the choice of sentences belonging to the speech sample. It was decided for sentences with a predominance of plosive and fricative phonemes of Portuguese, because these are already used in studies of the reference in Brazilians (ALTMANN & LEDERMAN, 1990; GENARO et al, 2004; SILVA, 2007). Furthermore, the high-pressure consonants, such as plosives and fricatives, are considered vulnerable sounds speech for individuals with cleft palate. Therefore, these phonemes are part of the inventory of all languages (WATSON et al, 2001, PETERSON-FALZONE, 2006; HENNINGSSON et al, 2008). The second important aspect so as far it concerns to perceptual assessment, are the conditions in which they were obtained. In this work, it was used the audio recording of speech samples in a sound-treated environment. Afterwards, the speech was analyzed separately by evaluators, which enabled to verify the inter-judge reliability. The coefficients of agreement between evaluators, the perceptual assessment of this study ranged from substantial to almost perfect for all assessed items (hypernasality and degree, presence of CAD and ANAE). JOHN et al. (2006) considers that this form of analysis of the speech provides a higher scientific credibility. It was found excellent agreement among the evaluators, which agrees with the findings with LEWIS et al (2003), PALL et al (2005) and KEUNING et al (1999) studies, who reported the influence of clinical experience in perceptual assessment. According to the authors, there is a higher concordance of skillful professionals in comparison to less skillful ones. This fact affects directly the interpretation of the results.
It was not found in the literature a similar study in format, in order to compare the three techniques with different approaches of palatoplasty in patients with cleft palate with homogeneous characteristics, which tacled one of the interfering factors in clinical results of speech and velopharyngeal function.
There are studies in the literature that adopt different variables to compare different techniques of palatoplasty, such as the need of pharyngeal flap (MARRINAN et al, 1998), morphometric measurements of the palate (BAE et al, 2002; FROES FILHO, 2003) and others who use variables related to speech and velopharyngeal function (DREYER & TRIER, 1984; FURLOW, 1986; VAN LIERDE et al, 2004).
It was initially established in this study the presence or absence of hypernasality (and its severity correspondent degree), CAD and ANAE in all techniques. These changes in speech are some of the variables of interest by researchers who investigate speech production in individuals with cleft lip and palate (HARDIN-JONES et al, 1993, KIRSHNER et al, 2000; VAN LIERDE et al, 2004; KOSHLA et al, 2008, HENNINGSSON et al, 2008). As it is possible to observe in Tables 1, 2 and 3, in the total sample of three groups, there is little occurrence of hypernasality, and when the present degree of hypernasality ranged around slight to moderate. For other changes, most of the sample presented no CAD and ANAE.
The precepted theoretical framework presents consistent data that agrees with the findings described above, that is, when studies compare primary palatoplasty techniques in relation to speech, even with enough "n" sample, it does not present a statistically significant difference among the techniques (SCHÖNWEILER, 1999; HARDIN-JONES, 1993). However, it was found a study in the proofread literature which difference between the two techniques. Van Lierde et al (2004) examined the speech results between FURLOW technique and WARDILL-KILNER techniques. The evaluation was performed 18 years after the surgery, in which was found that individuals in the group who underwent to the FURLOW palatoplasty presented statistically more hypernasality and a worse performance on speech intelligibility than the group of the WARDILL-KILNER technique. Whereas, another study proposed to verify the performance of the FURLOW technique achieved satisfactory results in relation to speech. From a sample of 140 participants with cleft lip and palate, 83% had no hypernasality, 84% had velopharyngeal insufficiency, 91% had no nasal air escape, 69% had no compensatory articulation (KOSHLA, 2008).
When comparing the results of the judgments obtained from the speech recordings among the techniques, it was examined that no significant statistical difference was found. This result was included because of the fixed sample. But even with this restriction, a very favorable information was obtained, that is, the findings of perceptual assessment were satisfying in all three techniques.
There is no consensus in the literature regarding to the best technique of palatoplasty because of a range in factors associated to the development of speech (YU et al, 2001). Many studies mention that different techniques of palatoplasty lead to different results of speech. This possibly happens due to disagreements in applied methodologies in studies that compare the techniques of palatoplasty. Because of this fact, difficulty in relating our findings with other research located in the literature came across this research. To LEOW & LO (2008) and SHAW (2004) one of the best ways to identify the most appropriate surgical technique is through well-controlled and randomized studies, originally conducted by a clinical prospective experiment for each type of cleft.
With technological advances occurred over the years, there are a series of diagnostic tools available which are used for different types of evaluation, and most of the references mention the combination of one or more tests to concur to the understanding of VFS physiology (GOLDING-KUSHNER et al, 1990; D'ANTONIO & SCHERER, 1995; ROCHA, 2002, SILVA, 2007; RAIMUNDO, 2007).
Videonasoendoscopy is an instrumental method for assessing velopharyngeal function that enables viewing of nasal cavities, pharynx and larynx with dynamic, direct and in locus images of anatomical structures, and it is considered one of the most appropriate for evaluating the VFS (PONTES & BEHLAU, 2005). It is possible to observe in this test the closure patterns (or even the best attempt of occlusion) of the VFS, including speech with specific features and degree of movement of the soft palate and the pharyngeal walls (WILLIAMS, 1998; KUEHN & HENNE, 2003; SHPRINTZEN, 2004; TRINDADE et al, 2007; PEGORARO-KROOK et al, 2008).
This exam should be carried out in the presence of trained and skillful professionals, and when carried out, being performed in the presence of otorhinolaryngologists, plastic surgeons and speech therapists to examine, interpret and define the conduct. It was used the Golding-Kushner scale to standardize the final interpretation regarding to the clinical estimate of the size VFS gap, which means, to estimate the velopharyngeal competence of the individuals.
This scale has been used by YOON (2006) and tested by SIE et al (2008) in a multicentric study that assessed the variability inter-and intra-examiner and found out satisfying and reliable correlated coefficients in the description of disturbances in the VFS, mainly concerning to estimate of the gap. There are also national surveys assessing velopharyngeal function according to the International Working Group Guidelines organized by GOLDING-KUSHNER. PEGORARO-KROOK et al (2008) analyzed the movements of the pharyngeal and velar walls and the velopharyngeal gap during the nasal endoscopy assment in the velopharyx before and during diagnostic therapy. It was used in the research group the same protocol in the study conducted by SILVA (2008), which sought to correlate the performance of velopharyngeal function using the same GOLDING-KUSHNER instrument and the results of otoscopy in children with cleft lip and palate.
It was found on the proofread literature that the experience as much as in the accomplishment as and in the analysis of videonasoendoscopy exam is paramount. For this reason, this study's proposal examine the agreement among evaluators in which regards to the clinical estimate of the size of the gap, which ranged from substantial to almost perfect. This finding allows an inference that the evaluators staff is very capable and illustrates that the adopted criteria for the interpretation of the findings are quite homogeneous among the judges. The findings agree with previous scientific studies that used the protocol proposed by GOLDING-KUSHNER and colleagues, that is, the information obtained is reliable to the proposed goal. However, as already discussed earlier in this chapter, possibly a statistically significant difference was not found between the techniques of palatoplasty on the clinical estimate on the gap's size due to the fixed sample belonging to the research.
This study was confined itself to analyze separately the results of each assessment. There is a real risk to make a direct correlation among the severity of the results of perceptual assessment with the instrumental (videonasoendoscopy examination). Although many physicians agree that many of the patterns found in the slurred speech of individuals with cleft are probably the results of previous or current VPD, there is a hiatus of research data to confirm this causal relationship (D'ANTONIO & SCHERER, 1995). The cause of velopharyngeal closure and speech is rarely so well defined as both physicians and researchers would like to be.
Studies that associates specific problems of speech (and the severity of these problems) for measurements of velopharyngeal closure have frequently produced contradictory and confusing results because of problems in measuring as much as in the production of speech as in the velopharyngeal function (PETERSON-FALZONE et al, 2001). According to WARREN et al (1994), hypernasality is possibly associated with the time of opening of the VFS in certain circumstances than directly with the opening degree or the volume of airflow that escapes through the nasal cavity. For example, there was a case in which the velopharyngeal closure is appropriate, according to the assessment of the instruments, it may have hypernasality due to the abnormality in the temporal spectrum of velopharyngeal closure.
It is suitable to emphasize that the hypernasality and ANEA are clinical manifestations of VPD, and the latter can also be a result of changes in the articulations. However, it is not possible to affirm the same regarding to compensatory articulation disorders. These may be the result of bad articulation habits acquired in childhood, that do not present physical or neuromuscular changes (JOHNS et al, 2003). Besides, if there is a change in velopharyngeal closure, it may also occur the appearance of compensatory articulation, which can be considered as a strategy in an attempt of compensating the inefficiency of imposing air pressure in the oral cavity. Regarding to the deficit in the performance of the articulation of velopharyngeal structures may result in the formation of intraoral pressure insufficient to form the plosive and fricative phonemes, for instance. Thus, the individuals with cleft palate who have VFD can replace the anterior sounds of speech by posterior articulating points in an attempt to compensate the velopharyngeal impairment (PETERSON-FALZONE et al, 2001; TRINDADE & TRINDADE, 1996).
LEOW & LO (2008) state that the surgical techniques suffer a profound influence of confusing variables, when not controlled. In this study regarding to a possible control of confusing factors, it was found out that the size of tonsils and adenoids, the presence of fistulas and speech therapy did not affect the results in comparison among surgical techniques.
The absence of differences among the techniques, as much as in the perceptual assessment and instrumental, it may have happened due to methodological flaws inherent in cross-sectional surveys, to limitations of each assessment by the subjectivity of interpretation of both tests, and especially, as the size of the fixed sample.
For the reasons shown, it was observed that the ratings, either instrumental or perceptual, provide important data with regards to the velopharyngeal function and speech of individuals with cleft lip and palate. The interpretation of both assessments demand from professionals an understanding of the velopharyngeal sphincter, speaking physiology, especially about the advantages and limitations of each assessment protocol. Through its results, the staff will decide which therapeutic measures to be taken. Each technique is characterized by its peculiarity, but regarding to velopharyngeal function and its repercussion on resonance, speech and velopharyngeal closure, it was found in this study similar satisfying findings in three types of palatoplasty.
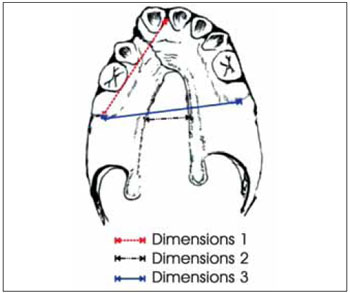
Figure 1. Dimensions of the palate.
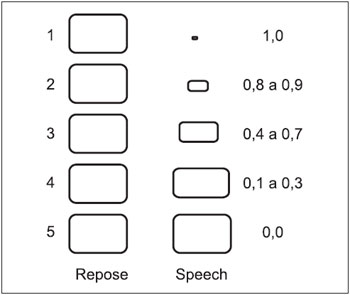
Figure 2. Estimate the size of the clinical gap, divided into five categories.
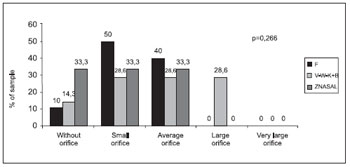
Figure 3. Estimating the clinical gap size of the velopharyngeal sphincter in the three techniques.
The findings of the perceptual and instrumental assessment did not presented statistically significant differences among the three different techniques of palatoplasty. However, the results in both evaluations were satisfying.
In the perceptual assessment, it was found in all techniques little occurrence of hypernasality, and when this exam presents the severity, it ranged from slight to moderate. Regarding to the CAD, it was found its the presence only in the Furlow technique. In what concerns the ANAE, it was found its presence in the minority of individuals in the three techniques.
There was no difference in the results of perceptual assessment as to the phonetic composition of the speech sample.
In the instrumental assessment , it was found in all techniques a variation of the clinical estimate of the size of the gap between the rating "no gap" (total closure of the VFS) and "large gap" (inefficient closure).
REFERENCES1. Altmann EBC, Lederman H. Videofluroscopia da Deglutição e do Esfíncter Velo-Faríngico: Padronização do Exame. Pró-fono Rev de Atual Cient.1990, 2(1):9-16.
2. Altmann EBC. Anatomia e fisiologia do esfíncter velofaríngeo. In: Altmann EBC, editor. Fissuras labiopalatinas. 4 ed. Carapicuíba: Pró-fono; 1997, p.133-156.
3. Amaral SA, Genaro KF. Análise da fala em indivíduos com fissura lábiopalatina operada. Pró-fono Rev de Atual Cient. 1996, (8)1:36-46.
4. American Cleft Palate-Craniofacial Association [página na internet]. Parameters for evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Chapel Hill: American Cleft Palate-Craniofacial Association. Revised Edition November 2007. Disponível em: http://www.acpa-cpf.org/teamcare/Parameters07rev.pdf. Acessado em 4 de janeiro de 2009.
5. Bae YC, Kim JH, Lee J, Hwang SM, Kim SS. Comparative Study of the Extent of Palatal Lengthening by Different Methods. Annals of Plastic Surgery. 2002, 48(4):359-364.
6. Bertier CE, Trindade IEK. Cirurgias primárias de lábio e palato. In: Trindade IEK, Silva Filho OG, editors. Fissura Labiopalatinas uma abordagem interdisciplinar. São Paulo: Santos; 2007, p. 73-86.
7. Braithwaite F. Congenital deformities II. Cleft palate repair. Mod. Trends Plast. Surg. 1964, 16:30-49.
8. Brodsky L. Modern assessment of tonsils and adenoids. Pediatr Clinic N Am. 1989, 36:1551-69.
9. Bzoch KR. Introduction to the study of communicative disorders in cleft palate and related craniofacial anomalies. In: Bzoch KR. Editor. Communicative disorders related to cleft lip and palate. 5 th. Ed. Austin: pro-ed.; 2004, p.3-66.
10. Cano M I, Navarro MI. Dificuldades no desenvolvimento da fala e da linguagem oral na infância e na adolescência. In: manual de Desenvolvimento e Alterações da Linguagem na Criança e no Adulto. Puyuelo M, Rondal J. (org). Porto Alegre: Artmed. 2007, p.277-314 .
11. Carvalhal LHSK. Descrição das alterações otológicas de pacientes com fissura labiopalatina ou palatina isolada [dissertação]. Porto Alegre: Faculdade de Medicina - Universidade Federal do Rio Grande do Sul; 2003.
12. D'Antonio L L, Eichenberg BJ, Zimmerman GJ, et al. Radiographic and aerodynamic measures of Velopharyngeal anatomy and function following Furlow Z plasty. Plast. Reconstr. Surg. 2000, 106-539.
13. D'Antonio LL, Scherer NJ. The Evaluation of speech Disorders associated with clefting. In: Cleft Palate Speech Management: Multidisciplinary approach. Shprintzen RJ, Bardach J.(editors). St Louis Missouri: Mosby; 1995, p.176-218.
14. Dreyer MT, Trier CW. A Comparison of palatoplasty techniques. Cleft palate Journal. 1984, 21(4):251-253.
15. Fleiss JL. Statistical methods for rates and proportions. New York: John Wiley & Sons, 1973. França CMC, Locks A. Incidência das fissuras lábio-palatinas de crianças nascidas na cidade de Joinville (SC) no período de 1994 a 2000. Jornal Brasileiro de Ortodontia e Ortopedia Facial. 2003, 47(8):429-36.
16. Froes Filho RR. Estudo Morfométrico comparativo entre três técnicas cirúrgicas de palatoplastia para reposicionamento do palato mole [dissertação]. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2003.
17. Furlow LT Jr. Cleft palate repair by Double opposing Z-plasty. Plast. Reconstr. Surg. 1986, 78:724-36.
18. Genaro KF, Fukushiro AP, Suguimoto MLFCP. Avaliação e tratamento dos distúrbios da fala. In: Trindade IEK, Silva Filho OG. Fissuras Labiopalatinas: Uma abordagem Interdisciplinar. São Paulo: Santos; 2007, p.109-122.
19. Genaro KF, Yamashita RP, Trindade IKE. Avaliação clínica e instrumental na fissura labiopalatina. In: Ferreira LP, Befi-Lopes DM, Limongi SCO. Tratado de Fonoaudiologia. São Paulo: Rocca; 2004, p.456-477.
20. Golding-Kushner KJ et al. Standardization for the reporting of nasopharyngoscopy and multiview videofluoroscopy: A report from an international working group. Cleft Palate J. 1990, 27(4):337-47.
21. Gomes PRM, Mélega JM. Tratamento Cirúrgico. In: Altmann EBC. Fissuras labiopalatinas. 4 ed. Carapicuíba: Pró-Fono; 2005, p.61-71
22. Hardin-Jones MH, Jones DL. Speech production of preschoolers with cleft palate. Cleft Palate Craniofac J. 2005, 42(1):7-13.
23. Hassan ME, Askar S. Does palatal muscle reconstruction affect the functional outcome of cleft palate surgery? Plast. Reconstruct. Surg. 2007, 119(6):1859-65.
24. Henningsson G. et al. Universal parameters for reporting speech outcomes in individuals with cleft palate. Cleft Palate-Craniofacial J. 2008, 45(1):1-17.
25. John A, Sell D, Sweeney T, Harding-Bell A, Williams A. The Cleft palate audit for speech-augmented: a validated and reliable measure for auditing cleft speech. Cleft Palate Craniofac J. 2006, 43(3):272-288.
26. Keuning KH, Wieneke GH, Dejonckere PH. The intrajudge reliability of the perceptual rating of cleft palate speech before and after pharyngeal flap surgery: the effect of judges and speech samples. Cleft Palate Journal. 1999, 36(4):328-333.
27. Khosla RK, Mabry K, Charles L, Castiglione FACS. Clinical Outcomes of the Furlow Z-Plasty for Primary Cleft Palate Repair. Cleft Palate-Craniofacial Journal. 2008, 45(5):501-10.
28. Kirschner RE, Randall P, Wang P, Jawad A, Duran M, Huang BAK, Solot C, Cohen BAM. Cleft palate repair at 3 to 7 months of age. Plastic and Reconstructive Surgery. 2000, 105(6):2127-2132.
29. Krause CJ, Tharp RF, Morris HL. A comparative study of results of the von Langenbeck and V-Y pushback palatoplasties. Cleft Palate J. 1976, 13(1):11-19.
30. Kruse LS. Repercussões do momento da palatoplastia na otoscopia e audiometria de pacientes com fissura palatina entre seis e 12 anos de idade [dissertação]. Porto Alegre: Universidade Federal do Rio Grande do Sul, Programa de Pós-Graduação em Medicina: Cirurgia; 2005.
31. Kuehn DP, Henne LJ. Speech Evaluation and Treatment for Patients with Cleft Palate. American Journal of Speech-Language Pathology. 2003, 12:103-109
32. Kummer AW. Perceptual assessment. In: Kummer AW. Cleft Palate and craniofacial anomalies: the effects on speech and resonance. San Diego: Singular Thomson Learning; 2001. p.265-90b.
33. Landis Jr, Koch GG. The measurement of obsever agreement for categorical data. Bometrics, Washington. 1997, 33(1):159-174.
34. Leow AM, Lo LJ. Palatoplasty: Evolution and controversies. Chang Gung Med J. 2008, 31(4):335-45.
35. Lessa S. Insuficiência velofaríngea. In: Carreirão S, Lessa S, Zanini SA. Tratamento das fissuras labiopalatinas. 2 ed. Rio e Janeiro, Revinter. 1996, p.237-51.
36. Lewis KE, Watterson TL, Houghton S. The influence of listener experience and academic training on ratings of nasality. J Commun Disord. 2003, 36(1): 49-58.
37. Marrinan EM, LaBrie RA, Mulliken JB. Velopharyngeal function in nonsyndromic cleft palate: relevance of surgical technique, age at repair, and cleft type. Cleft Palate Craniofac J. 1998, 35(2):95-100.
38. McWilliams BJ, Morris HL, Shelton RL. Cleft Palate Speech. 2nd ed. Philadelphia: BC Decker. 1990, p.40-49.
39. Murray JC. Gene/environment causes of cleft lip an/or palate. Clin Genet, Copehagen. 2002, 61(4):248-256.
40. Nagem Filho H, Moraes N, Rocha RGF. Contribuições para o estudo da prevalência das más formações congênitas lábio-palatais na população escolar de Bauru. Revista da Faculdade de Odontologia da Universidade de São Paulo. 1968, 6(2):111-28.
41. Nakajima T. Mitsudome A. Yosikawa A. Postoperative speech development based on cleft types in children with cleft palate. Pediatrics International. 2001, 43(6):666-72.
42. Nakamura N, Ogata Y, Sasaguri M, Suzuki A, Kikuta R, Ohishi. Aerodynamic and cephalometric analyses of velopharyngeal structure and function following repushback surgery for secundary correction in cleft palate. Cleft Palate Craniofac J. 2003, 40(1):46-53.
43. Nunes LMN, Queluz DP, Pereira AC. Prevalence of oral cleft in Campos dos Goytacazes-RJ, 1999-2004. Rev Bras de Epidemiologia. 2007, 10(1).
44. Paal S, Reulbach U, Strobel-Schwarthoff K, Nkenke E, Shuster M. Evaluation of speech disorders in children with cleft lip and palate. J Orofaci Orthop. 2005, 66(4):270-278.
45. Pegoraro-Krook MI, Dutka-Souza JCR, Marino VCC. Nasoendoscopy of Velopharynx before and during diagnostic therapy. J Appl Oral Sci. 2008, 16(3):181-8.
46. Pegoraro-Krook MI. Avaliação da fala de pacientes que apresentam inadequação velofaríngea e que utilizam prótese de palato [dissertação]. São Paulo: Escola Paulista de Medicina; 1995.
47. Pegoraro-Krook MI, Dutka-Souza JCR, Magalhães LCT, Feniman MR. Intervenção fonoaudiológica na fissura palatina. In: Ferreira LP, Befi-Lopes DM, Limongi SCO. (Edit.). Tratado de Fonoaudiologia. São Paulo: Rocca; 2004, p.439-455.b
48. Peterson-Falzone SJ, Hardin-Jones MA, Karnell MP. Communication disorders associated with cleft palate. In: Peterson-Falzone SJ, Hardin-Jones MA, Karnell MP. Editor. Cleft Palate Speech.3 ed. St. Louis, Missouri: Mosby; 2001, p.162-99.
49. Peterson-Falzone SJ, Trost-Cardamone JE, Karnell MP, Hardin-Jones MA. The clinician's guide to treating cleft palate speech. Mosby: St. Louis, Missouri; 2006.
50. Polzer I, Breitsprecher L, Winter K, Biffar R. Videoendoscopic,speech and hearing in cleft palate children after levator-palatopharyngeus surgery according to Kriens. J Craniomaxillofac Surg. 2006, 34:52-6.
51. Pontes PAL, Behlau MS. Nasolaringoscopia. In: Altmann, E.B.C. Fissuras labiopalatinas. 4 ed. Carapicuíba: Pró-fono Departamento Editorial; 2005, p.175-183.
52. Pulkkinen J, Ranta R, Heliövaara A, Haapanen M. Craniofacial characteristics and velopharyngeal function in cleft lip/palate children with and without adenoidectomy. Eur Arch Otorhinolaryngol. 2002, 259(2):100-104.
53. Raimundo GM. Medidas de Nasalância em Crianças com Fissura Labiopalatina e Fala Normal [dissertação]. Ribeirão Preto: Universidade de São Paulo; 2007.
54. Rocha DL. Insuficiência velofaríngea. In: Mélega JM. Cirurgia Plástica: fundamentos e arte, cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002, p.178-96.
55. Schönweiler R, Lisson JA, Schönweiler B, Eckardt A, Ptok, M, Tränkmann J, Hausamen J. A retrospective study of hearing, speech and language function in children with clefts following palatoplasty and veloplasty procedures at 18-24 months of age. International Journal of Pediatric Otorhinolaryngology. 1999, 50(3):205-217.
56. Sell D, Harding A, Grunwell P. A screening assessment of cleft palate speech (Great Ormond Street Speech Assessment). Eur J Disord Commun. 1999, 29(1):1-15.
57. Shaw W. Global strategies to reduce the health care burden of craniofacial anomalies: report of WHO meetings on international collaborative research on craniofacial anomalies. Cleft Palate Craniofac J. 2004; 41(3):238-43.
58. Shprintzen RJ, Bardach J. Cleft palate Speech management: A Multidisciplinary Approach. New York, Mosby; 1995.
59. Shprintzen RJ.Nasopharyngoscopy. In: Bzoch KR, editor. Communicative disorders related to cleft lip and palate. 5th ed. Boston: Little & Brown; 2004.
60. Shprintzen RJ. Insuficiência Velofaríngea. In: Fissuras labiopalatinas. Altmann EBC. (org). Ed. Pró-fono. 4ª. Ed. 2005, p.157-183.
61. Sie KCY, Starr JR, Bloom DC, Cummingham M, et al. Multicenter interrater and intrarater reliability in the endoscopic evaluation of Velopharyngeal insufficiency. Arch Otolaryngol Head Neck Surg. 2008, 134(7):757-63.
62. Silva L. Medidas de nasalância da fala de crianças com fissura lábio-palatina e sua correlação com o julgamento perceptivo-auditivo da nasalidade. [dissertação] Bauru: Universidade de São Paulo; 2007.
63. Silva DP. Repercussões da disfunção velofaríngea na orelha média de pacientes com fissura palatina corrigida [dissertação]. Porto Alegre: Universidade Federal do Rio Grande do Sul. Faculdade de Medicina. Programa de Pós-Graduação em Medicina: Ciências Cirúrgicas; 2008.
64. Trindade IEK, Trindade Junior AS. Avaliação funcional da inadequação velofaríngea. In: Carreirão, S; Lessa, S; Zanini, AS. Editores. Tratamento das fissuras labiopalatinas. 2ª. Ed. Rio de Janeiro: Revinter; 1996. p.223-35.
65. Trindade IEK, Yamashita RP, Gonçalves CGAB. Diagnóstico instrumental da disfunção velofaríngea. In: Trindade IEK, Silva Filho OG. Fissuras labiopalatinas uma abordagem interdisciplina. São Paulo: Santos; 2007, p.123-143.
66. Trost-Cardamone JE. Diagnosis of specific cleft speech errors patterns for planning therapy or physical management needs. In: Bzoch, K.R. Communicative disorders related to cleft palate speech. 4th ed. Boston: Litle, Brown, 2004, p.137-173.
67. Van Demark DR, Hardin MA. Longitudinal evaluation of articulation and velopharyngeal competence of patients with pharyngeal flaps. Cleft Palate J. 1985, 22(3):163-172.
68. Van Lierde KM, Monstrey S, Bonte K, Van Cauwenberge P, Vinck B. The Long-term speech outcome in Flemish Young adults two different types of palatoplasty. Int. J. of Pediat Oto. 2004, 68(7):865-75.
69. Warren DW, Dalston RM, Mayor R. Hypernasality in the presence of "adequate" Velopharyngeal closure. Cleft Palate-Craniofac J. 1994, 30(2):150-4.
70. Watson ACH, Sell DA. Grunwell P. Management of cleft lip and palate. London: Whurr; 2001.
71. Williams WN, et al. A methodology report of a randomized prospective clinical trial to assess Velopharyngeal function for speech following palatal surgery. Contr Clin Trials. 1998, 19(3):297-312.
72. Williams AC, Sandy JR, Thomas S, Sell D, Sterne JAC. Influence of surgeon's experience on speech outcome in cleft lip and palate. The Lancet. 1999 Nov; 354:1697-8.
73. Witt PD, Wahlen JC, Marsh JL, Grames LM, Pilgram TK. The effect of surgeon experience on velopharyngeal functional outcome following palatoplasty: is there a learning curve? Plast Reconstr Surg. 1998, 102(5):1375-84.
74. Wormald PJ. Prescott CA. Adenoids: comparison of radiological assessment methods with clinical and endoscopic findings. J Laryngol Otol. 1992, 106(4):342-4.
75. Yoon PJ, Starr JR, Perkins JA, Bloom D, Sie KCY. Interrater and intrarater reliability in the evaluation of Velopharyngeal insufficiency within a single institution. Arch Otolaryngol Head Neck Surg. 2006, 132:947-51.
76. Yu CC, Chen PK, Chen YR. Comparison of speech results after Furlow palatoplasty an von Langenbeck palatoplasty in incomplete cleft of the secondary palate. Chang Gun Med J. 2001, 24(10):628-32.
1. Master by Post graduation in Child and Adolescent Health of the Federal university of Rio Grande do Sul (UFRGS). Clinic Therapist Speech.
2. Doctorate in Medicine and Surgery. Doctor contracted of the Hospital das Clínicas of Porto Alegre.
3. Doctorate in Medicine (Surgery Clinic). Professor Assistant of the Federal University of Rio Grande do Sul.
Institution: Federal University of Rio Grande do Sul (UFRGS). Porto Alegre / RS - Brazil.Mail Address: Lauren Medeiros Paniagua - Avenida João Wallig, 1705, Apto. 267 - Porto Alegre / RS - Brazil - ZIP CODE: 91340-001 - Telephone: (+55 51) 3273-5173 - E-mail: tchelauren@yahoo.com.br. Financial Support: Bolsa CNPq. Article received on July 1, 2009. Article approved on January 03, 2010.