INTRODUCTIONThe practice of local anesthesia with sedation for rhinoplasty is a rapidly growing field (KOEPPE, CONSTANTINESCU et al., 2005). Procedures are considered appropriate for this practice, in addition to rhinoplasty, other cosmetic procedures such as SMAS rhytidectomy, blepharoplasty, liposuction, breast enhancement and reduction, and endoscopies, colonoscopies, procedures, urological, dental, and orthopedic and microlaparoscopy (HAUSMAN, 2003).
In Brazil, in 2003, the Federal Council of Medicine defined "sedation" as a medical act, performed by the use of drugs with the goal of providing comfort to the patient to perform medical or dental procedures, classifying it as mild, moderate (Conscious Sedation) and Deep (CFM, 2003). In the case of deep sedation, where the patient is hardly aroused by verbal commands but responds to painful stimuli, spontaneous ventilation may be compromised and inadequate assistance being necessary to the maintenance of patent airway, the doctor performing the procedure can not undertake if both the administration of deep sedation and this should be left to another qualified physician.
To ensure comfort and safety to patients during local anesthesia, analgesia / sedation should have fast onset of action, to promote amnesia, have minimal cardio respiratory depression without compromising the patient's cooperation during surgery (DENG, XIAO et al., 2001). Different medications can be used for this purpose, and common drugs used propofol, sevoflurane, midazolam, non-steroidal anti-inflammatory drugs (NSAIDs), ketamine, fentanyl, remifentanil, pethidine (meperidine) and local anesthetics (FRODEL and AHLSTROM, 2002; BING, MCAULIFFE et al., 2002).
In March 2006 in our hospital, a record was set parallel to the medical records to be used for all patients undergoing rhinoseptoplasty. In it were described data on anatomical, morphological and functional view of individuals, details of surgery and anesthesia, and the postoperative results. For many years local anesthesia and sedation have been used in rhinoseptoplasties, but until now had not been performed in our department any objective analysis of the frequency of their use in classes and quantities of drugs used and their effectiveness in promoting patient comfort during the procedure.
The objective of this study is to analyze the efficacy of intraoperative analgesia and amnesia by visual analog scales and subjective in rhinoseptoplasties performed under local anesthesia and sedation, seeking associations with the average quantities of drugs used in this operation.
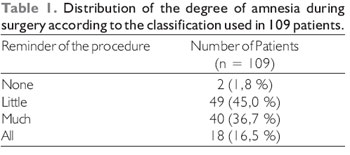
METHODWe conducted a retrospective study based on reports relating to 158 rhinoseptoplasties performed between March 2006 and January 2007. The surgeon was instructed to register, among other information, right after the end of each surgery, data on sex, age, or without use of lidocaine, bupivacaine, or other local anesthetics, midazolam, fentanyl, pethidine or other hypnotics / analgesics including concentrations and amounts used of each drug. In the first return postoperative patient was asked to quantify the pain experienced during surgery using a visual analog scale as described by HASEN et al (HASEN, SAMARTZIS et al., 2003) which classifies the pain from 0 (no pain) to 10 (worst pain imaginable) and answer the question: "How Mr. (a) remember the procedure?" choosing one of four options: "nothing", "little," "very" or "all" for the subjective assessment of intraoperative amnesia. Amnesia was considered as ideal one in which the patient reported recall "nothing" or "somewhat" of the surgical procedure.
Likewise, the report had space for the surgeon to report, briefly, an effect that could be associated with the use of drugs used (such as changes in blood pressure or heart rate).
The data collected in the surgical reports were stored in a database created with SPSS 10.0 for Windows (SPSS Inc, Chicago, IL), from which we obtained the mean, median and standard deviations of the quantities of medication used and the quantification of intraoperative pain. Correlations were made between pain and amount of medication used by the coefficient of Pearson correlation. The medium amounts of medications were compared between the group of patients who achieved optimal perioperative amnesia and those who have not obtained using the nonparametric Mann-Whitney U. Were considered statistically significant for p values <0.05.
RESULTSOf the reported 158 surgeries were excluded from analysis 3 (1.9%) having been performed with general anesthesia and 46 (29.1%) for not reporting the data relating to registration of intraoperative pain.
Of the 109 cases included in the analysis, 80 (73.4%) were female and 29 (26.6%) were males, mean age was 29.3 ± 9.5 years (minimum 15.4 and maximum of 56.6 years).
The first outpatient was in average 6.6 ± 2.1 days (minimum 4, maximum 19) after surgery. The median intensity of pain attributed by patients at the first outpatient return was 1 (25-75 percentile: 0 - 3). The distribution of intensities of pain during surgery is shown in Figure 1, the classification and distribution of amnesia during surgery is presented in Table 1.
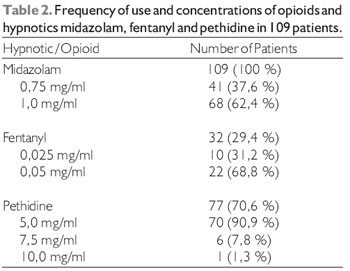
Midazolam was used in 100% of the surgeries, his association with pethidine was the most frequent, which is used in 77 (70.6%) surgeries, while the association with fentanyl was used in 32 (29.4%) of surgeries. There was no record on the use of other hypnotics / sedatives or opioids. The frequency of use of each drug dilution is presented in Table 2. The amount of midazolam used were not recorded in the reports of 11 (10.1%) of 109 surgeries in which it was used. Likewise, the amount of fentanyl used was not recorded in the report of 1 (3.1%) of 32 surgeries in which it was used, and quantities of pethidine were not available in 15 (19.5%) of 77 surgeries in that was used. The average quantities used for each medication hypnotic / opioids for surgery when they were recorded is shown in Table 3. There were no statistically significant differences between the quantities of medication used among the group of patients with amnesia considered ideal when compared with those who did not obtain satisfactory amnesia for the procedure.
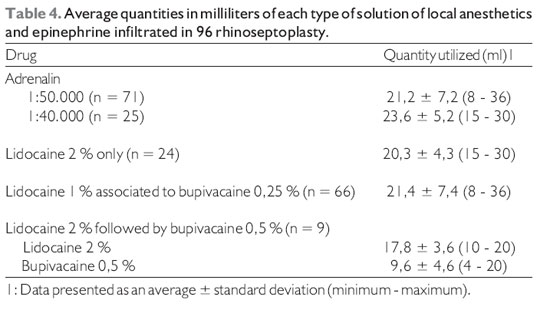
The adrenaline was used as a vasoconstrictor with local anesthetics in all 109 surgeries, and in 27 patients (24.8%) was used at 1:40,000 dilutions and 82 (72.5%) diluted 1:50,000. Also, lidocaine was used as a local anesthetic in all 109 surgeries, and in 25 patients (22.9%) was used alone and in 84 (77.1%) was used with or followed by bupivacaine. The mean amounts of epinephrine, lidocaine and bupivacaine infiltrated were available for 96 surgeries (88.1%), and are presented in Table 4. There was no significant correlation between the amount of local anesthetic infiltration and intraoperative pain score (Pearson correlation coefficient = 0.065, p = 0.53).
In a report (0.9%) had a description of a patient who developed bradycardia immediately after lateral osteotomies, with spontaneous recovery of heart rate after seconds without the need for maneuvers or drug administration. There were no reports of other major complications during surgery.
DISCUSSIONThe conscious sedation (mild sedation) is the most commonly accepted, in which the patient is able to respond to painful stimuli and verbal and aims to reduce patient anxiety, promote analgesia and retrograde amnesia. Furthermore, it should be safe, ie present the least adverse effects such as cardiorespiratory depression and promote rapid postoperative recovery.
In relation to local anesthesia, analgesia and promotes the region applied, can reduce the amount of systemic medication for sedation during surgery (KOEPP, CONSTANTINESCU et al., 2005). Therefore it is crucial that the surgeon is accustomed to, after reaching a satisfactory sedation and doing an adequate infiltration of the nasal mucosa and blockage of nasal sensory nerves, allowing less dependence on sedatives and analgesia of the patient.
Around the world, aesthetic and reconstructive facial surgeries are performed in increasing frequency under local anesthesia with or without sedation (KOEPP, CONSTANTINESCU et al., 2005). This fact stems from the advantages of this approach regarding the use of general anesthesia, such as lower morbidity and cost (ULLMANN, LEVY et al., 1999). Following this trend, it is remarkable the large number of procedures performed under local anesthesia and sedation compared with general anesthesia, the service evaluated. A mild to moderate sedation requires the patient to be able to respond to verbal and / or tactile and does not require interventions to maintain patency of the airways or breathing can be performed by non-physician anesthetist (Cfm, 2003). An important practical impact of this is to reduce costs, since general anesthesia requires the presence of an anesthesiologist and patient observation period in units of post-anesthetic recovery. Furthermore, when dealing with a public health service, the poor availability of anesthesiologists may limit the number of procedures that can be performed under general anesthesia. Other potential benefits of local anesthesia include greater versatility in the scheduling of surgeries and a short hospital stay or even perform the procedure on an outpatient basis, which also reduces costs, decreases the probability of acquiring nosocomial infections (BITAR, MULLIS et al. , 2003). Moreover, in procedures that exceed 3 to 4 hours in duration, criteria that fit in the vast majority of rhinoseptoplasties practiced in service measured, local anesthesia is associated with lower rate of deep vein thrombosis and pulmonary embolism compared with general anesthesia (REINISCH, BRESNICk et al., 1998). Therefore, conducting rhinoseptoplasties under local anesthesia and sedation is certainly of great value in terms of increased productivity, reduced costs and decreased postoperative morbidity in the service evaluated.
Demographic data of patients undergoing rhinoseptoplasties service are assessed according to published data in the literature that show a predominance of young adults (DENG, XIAO et al., 2001). The percentage of female patients, however, is smaller than that seen in other studies (BITAR, MULLIS et al., 2003; HASEN, SAMARTZIS et al., 2003). One possible explanation for this fact is the gratuity of the procedure in the institution evaluated, making it more attractive to males who traditionally do not tend to feel so uncomfortable with facial imperfections. Another possible explanation is that, more recently, there is social pressure in order to get men to be concerned about the appearance and the current literature does not reflect this trend.
Sedation and local anesthesia during a surgical procedure should achieve three fundamental objectives: to reduce pain (including that associated with the injection of anesthetic) (FOSKO, GIBNEY et al., 1998), reduce patient anxiety during the surgery and produce amnesia (DENG, XIAO et al. 2001; PRATT, 2001). Regardless of the sedative and local anesthetic used, most of the patients showed satisfactory levels of analgesia (Figure 1). Seventy-five percent of patients reported pain levels considered acceptable (score on the visual analog scale <3).
In all cases reviewed, the adrenaline was the vasoconstrictor used in combination with local anesthetic. The advantages of using a topical vasoconstrictor include less bleeding, improved visibility of the operative field and increasing the effectiveness of local anesthetic. The two concentrations of adrenaline used (1:40,000 and 1:50,000) are not seen frequently in literature, commonly used concentrations of 1:100,000 or 1:200,000 (AHLSTROM and FRODEL, 2002; DEMIRTAS, 2005; KOEPP, CONSTANTINESCU et al., 2005). Although they were above the recommended concentrations used were not reported significant hemodynamic side effects. Possibly, there were cases of transient tachycardia secondary to administration of epinephrine, however, if there was not important enough to require additional maneuvers or medications or be characterized as a complication for any of the surgeons. Further studies are needed to establish whether the adrenaline, these higher concentrations, has additional benefits in terms of reduction of trans-operative bleeding and amount of local anesthetic used, since, in patients in categories I and II of the ASA (SAKLAD, 1941; DRIPPS, LAMONT et al., 1961), such mergers appear to be safe.
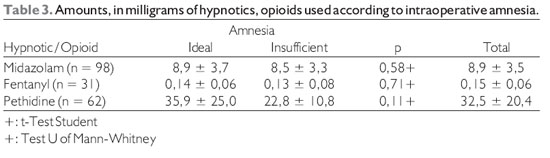
The techniques of local anesthesia associated with sedation with midazolam, pethidine and / or as described fentanyl were effective to promote comfort for the vast majority of patients undergoing rhinoplasty. There was no correlation between the degree of sedation and amnesia and the amount of sedatives used, suggesting different individual responses to medications.
BIBLIOGRAPHICAL REFERENCES1. Ahlstrom KK. e Frodel JL. Local anesthetics for facial plastic procedures. Otolaryngol Clin North Am. 2002, 35(1):29-53.
2. Bing JB, Mcauliffe MS, et al. Regional anesthesia with monitored anesthesia care for dermatologic laser surgery. Dermatol Clin. 2002, 20(1):123-134.
3. Bitar G, Mullis W, et al. Safety and Efficacy of Office-Based Surgery with Monitored Anesthesia Care/Sedation in 4778 Consecutive Plastic Surgery Procedures. Plastic & Reconstructive Surgery. 2003, 111(1):150-156.
4. CFM. Resolução CFM. C. F. D. Medicina. Diário Oficial da União. 1670/03 2003.
5. Demirtas Y, Ayhan S, Tulmac M, Findikcioglu F, Ozkose Z, Yalcin R, Atabay K. Hemodynamic effects of perioperative stressor events during rhinoplasty. Plastic & Reconstructive Surgery. 2005, 115(2):620-625.
6. Deng XM, Xiao WJ, et al. The Use of Midazolam and Small-Dose Ketamine for Sedation and Analgesia During Local Anesthesia. Anesthesia & Analgesia. 2001, 93(5):1174-1177.
7. Dripps RD, Lamont A, et al. The role of anesthesia in surgical mortality. JAMA, 1961, 178(3), 261-266.
8. Fosko SW, Gibney DM, et al. Repetitive pinching of the skin during lidocaine infiltration reduces patient discomfort. J Am Acad Dermatol. 1998, 39(1):74-78.
9. Hasen KV, Samartzis D., et al. An Outcome Study Comparing Intravenous Sedation with Midazolam/Fentanyl (Conscious Sedation) versus Propofol Infusion (Deep Sedation) for Aesthetic Surgery. Plastic & Reconstructive Surgery. 2003, 112(6):1683-1689.
10. Hausman LM. Advances in office-based anesthesia. Current Opinion in Anaesthesiology. 2003, 16(4):421-427.
11. Koeppe T, Constantinescu MA, et al. Current Trends in Local Anesthesia in Cosmetic Plastic Surgery of the Head and Neck: Results of a German National Survey and Observations on the Use of Ropivacaine. Plastic & Reconstructive Surgery. 2005, 115(6):1723-1730.
12. Pratt SD. Oral Premedication for Operations on the Face under Local Anesthesia: A Placebo-Controlled Double-Blind Trial. Plastic & Reconstructive Surgery. 2001, 108(3):644-646.
13. Reinisch JF, Bresnick SD, et al. Deep venous thrombosis and pulmonary embolism following facelifts: A study on incidence and prophylaxis. Plast Surg Forum. 1998, 21, p.159.
14. Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941, 2(3):281-284.
15. Ullmann Y, Levy Y, et al. Anesthesia for facial surgery. Aesthetic Plastic Surgery. 1999, 23(4):296-297.
1. Otolaryngologist at Hospital of the Medical School of USP and the Brazilian Institute Student Graduate - IBPG.
2. Dentist Specializing in Oral Implantology for the Paulista Association of Dental Surgeons Otorhinolaryngologist Skull and Maxillo-Facial Surgeon Member of the Brazilian Academy of Facial Plastic Surgery. Medical Advisor Group Face of Plastic Surgery, Department of Otorhinolaryngology, Hospital of the Medical School of USP Coordinator of the Brazilian Institute of Postgraduate - IBPG. Coordinator of the Brazilian Institute of Postgraduate - IBPG.
Instituition: Instituto Brasileiro de Pós Graduação - IBPG. São Paulo / SP - Brasil. Mail Address: Luiz Carlos de Melo Barboza Junior - Rua Sabará, 566 - conj. 102:104 - São Paulo / SP - Brazil - ZIP CODE: 01239-010 - Telefax: (+55 11) 3231-0051 - E-mail: carlosluiz@hotmail.com. Article received in February 2, 2010. Article approved in March 6, 2010.