INTRODUCTIONBasal Meningoencephalocele is a rare pathological entity that occurs in 1:35000 births (1, 2). It is characterized for the herniation of the neural tissue through a osseous structures of the base of the cranium deform (3, 4, 5).
The transsphenoidal Meningoencephalocele joint with anomalies of the facial development, the optic and the encephalic system (1, 5, 6, 7). The facial deformities are almost always present, and they found characteristics include hypertelorism, median nasal fissure, widened nasal base, cleft lip or palatal, syndrome of the cleft facial medial or bifid cranium occult frontal (8,9).
The transsphenoidal encephalocele generally is asymptomatic or an occasional finding, being the presentation most common for a mass located in the cranial line media (5). The clinical manifestations, when present, in part, depend on the age of the patient. In the absence of facial modifications, the diagnosis can be retarded for the adolescence or adult ages, when rhinorrhea, meningitis or inexplicable gradual visual deform encourage a diagnostic evaluation (8, 10, and 11).
Some children can present some signals and symptoms, including meningitis, nasal blockage, cranium facial deformities or liquoric fistulae, however, in some cases, the lesion cannot be discovered, occasionally up to be detected in an image examination.
The TC and the RNM are necessary to confirm the transsesfenoidal meningoencephalocele diagnosis, to define the presence of neural and vascular elements in the herniation and to disclose to the deforms in the osseous structures (5, 13). The RNM is the examination of choice for the diagnosis of this type of abnormality (12, 14). The three-dimensional TC can be useful for the planning of the complex cranium facial repairs (12, 14).
The aim of this report is present the case of a two-year-old patient of the male sex that although the scarcity of physical and clinical signals was diagnosed meningocele treated through endoscopic transnasal surgery using bilateral septal nasal mucosa shred, pedicellate in the sphenopalatine artery.
CASE REPORTRS, a two-year-old patient of the male sex, looked for our service in May, 2008 with a complaint of frequent episodes of sinusitis and acute otitis media, constant antibiotic use of ample specter. In the horoscope it was evidenced the presence of superior labial frenum and superior incisive diastases, though did not have discontinuity of mucosa in the palato and nor abnormality of the uvula.
The nasal endoscopy carried out with flexible nasopharingolaryngoscopy Pentax 3,2mm, evidenced rhynopathy allergic, posterior laryngitis and hypertrophy of adenoids, which they occupied, according to the finding of the examination, 50% of the choanae. The tomography study of cranium and face breast and the three-dimensional reconstruction evidenced media fissure cranial in funnel form (Figure 2). The magnetic resonance imaging of cranium and face breast evidenced a transsphenoidal meningocele invading the posterior portion of the nasal cavity (Figure 3). After a multicriteria evaluation before surgery, the chosen treatment was the transnasal endoscopic surgery, using bilateral septal nasal mucosa shred, pedicellate in the sphenopalatine artery.
The surgery was carried out under general anesthesia. A topic nasal vase-constriction was carried out. After that a nasal endoscopy was carried out using an endoscope of 4-mm, with an optic of 0-degrees. The lesion was in the posterior region of nasal septum. An infiltration of the previous portion of nasal septum with a solution of xylocaine and adrenalin (1:100.000), followed of the previous incision of the septal mucosa to the right, mucoperichondrium and periosteal release the right and the left after transfixing septal incision.
Two incisions parallel in the anteroposterior direction, from the initial incision, were carried out with the aim of create a shred pedicellate in the sphenopalatineartery the right (Figure 4). The left, three incisions were carried out with the aim to create the same shred pedicellate in the ipsilateral sphenopalatine artery. The septal cartilage was removed and private for use, if necessary, in the reconstruction of the osseous deform of the base of the cranium. The complete dissection of meningocele was carried out. The osseous disrafism of the base of the cranium (sphenoid) had the format of a "V" that hinders the use of cartilage or screens for sustentation of meningocele reduced, for this reason the use of shred of nasal mucosa became an effective solution (Figure 5).
Thus, after rotation of the shreds in the posterior direction, was applied fibrin glue, followed for the setting of Gelfoam and finally a sounding lead of Folley was inserted and that is inflated with intention to occupy the rhinopharynge keeping the located shreds, this remained per two days, with the child sedated in pediatric UTI. After two days the sounding lead of Folley was removed and the waked up child. No liquoric signal of fistulae was observed. After five days of hospital internment the child received high without signals from liquoric fistulae and infection.
The accompaniment of the patient occurs through ambulatories consultations where cautious nasal endoscopic is carried out. The patient is with 120 days of postoperative and complications were not observed until now.
DISCUSSIONThe lack of facial modifications in the physical examination and clinical manifestations that can to warning the doctor for a tomography evaluation detailed of the cranium and face breast makes it difficult diagnoses of meningoencephalocele. An apparently normal face, omits cranial deformities that can result in serious and fatal complications if badly lead by specialists. The manifestation of common pathologies of superior airways in this age group, united to the finding of a nasal endoscopic examination, without radiological complementation, can result in inadequate a surgical procedure in this case.
Thus, this in case that als demonstrates to the importance of the tomography study of the cranium and face breast in directed patients the specialties of craniomaxillofacial surgery and otorhinolaryngology. The radiological examinations united the three-dimensional reconstructions, are fundamental in such as way for diagnose, as for surgical planning, when possible.
Finally, the reconstruction of the cranial fissure and approach of meningoencephalocele through transnasal endoscopic surgery, showed a viable and effective option when carried out in a specialized center. The use of the shred of nasal septum, pedicellate in the sphenopalatine artery, allowed the separation of meningocele of the nasal cavity, even without correction of the cranial disrafism, minimizing the probability of meningitis along the life of this patient. This directly occurs due to nutrition sanguine of the shred, proceeding from the sphenopalatine artery, returning it in one tissue more robust, being useful in the closing of the cranial deform.
On the other hand, the surgery cause a septal perforation posterior important, that can result in crusts, bleeds, amongst other complications. In the adults its use is well described. However, in pediatric patients still is restricted and less described in literature. Some studies regarding complications with these shreds exist, as mucoceles, sinequans, necrosis and infection in adults. Studies for long periods of accompaniment not yet exist. However, the studies in validity demonstrate that these shreds had become a treatment secure and trustworthy for the defects of the base of the cranium.
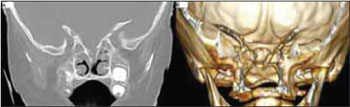
Figure 1. (a) The Coronal Cuts of TC, (b) Reconstruction with Osirix, demonstrating bifid of the perpendicular blade of the ethmoid and cranial media fissure.
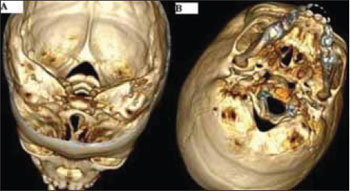
Figure 2. View (a) superior and (b) inferior of three-dimensional reconstruction, with Osirix, from TC, demonstrating disrafie (fissure) media cranial.
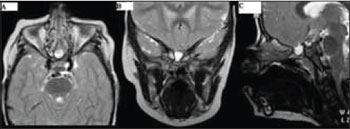
Figure 3. (a) Cuts Sagittal, (b) Cuts Coronal, (c) Cuts Axial of RNM in T2 demonstrating meningocele transsphenoidal.
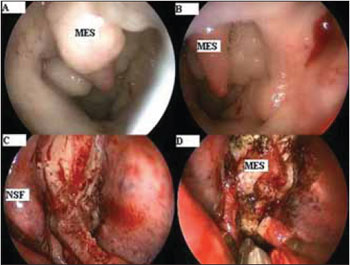
Figure 4. (A, B) Nasal Endoscopic showing meningocele involved for nasal mucosa. (c) Shred of nasal mucosa of septum the right, pedicellate in the sphenopalatine artery. (d) Dissection of meningocele.
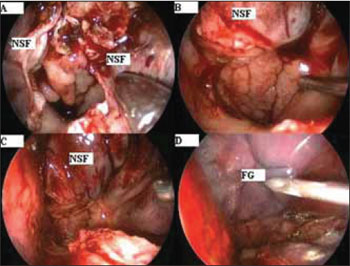
Figure 5. (a) Resection of meningocele. (B, C, D) Final aspect of the pedicellates septals shreds, occupying rhinopharynge.
We present a successful reconstruction of one congenital meningoencephalocele, omitted for a face without modifications, diagnosed after proceed of computerized tomography and RNM of cranium and face breast. Present Meningoencephalocele in the rhinopharynge, subjects the complications for presence of constant infections of superior airways and therefore corrected by transnasal endoscopic surgery, with the use of the shred of nasal septum pedicellate in the sphenopalatine artery. No complication occurred with the nasal shred and the deform of the base of the cranium was corrected successfully.
BIBLIOGRAPHICAL REFERENCES1. Larsen CE, Hudgins PA, Hunter SB. Skull-base meningoencephalocele presenting as a unilateral neck mass in a neonate. AJNR. 1995, 16:1161-1163.
2. Jabre A, Tabaddor R, Samaraweera R. Transsphenoidal meningoencephaloce-le in adults. Surg Neurol. 2000, 54(2):183-187.
3. Blustajn J, Netchine I, Fredy D, et al. Dysgenesis of the internal carotid artery associated with transsphenoidal encephalocele: a neural crest syndrome? AJNR. 1999, 20:1154-1157.
4. Machado MAC Jr, Barbosa VAO, Pires MCM, et al. Meningoencefaloventri- culocele transesfenoidal assintomática em adulto. Arq Neuropsiquiatr. 2001, 59(2-a):280-282.
5. Mylanus EAM, Marres HAM, Vlietman J, et al. Transalar sphenoidal ence-phalocele and respiratory distress in a neonate: a case report. Pediatrics. 1999, 103(1):1-12.
6. Diebler C, Dulac O. Cephaloceles: clinical and neuroradiological appearance. Neuroradiology. 1983, 25(4):199-216.
7. Elster AD, Branch CL Jr. Transalar sphenoidal encephaloceles: clinical and radiologic findings. Radiology. 1989, 170:245-247.
8. Yokota A, Matsukado Y, Fuwa I, et al. Anterior basal encephalocele of the neonatal and infantile period. Neurosurgery. 1986, 19(3):468-478.
9. DeMyer W. The median cleft face syndrome: differential diagnosis of cranium bifidum occultum, hypertelorism and median cleft nose, lip and palate. Neurology. 1967, 17(10):961-971.
10. Smith DE, Murphy MJ, Hitchom PW, et al. Transsphenoidal encephaloceles. Surg Neurol. 1983, 20(6):471-480.
11. Soyer P, Dobbelaere P, Benoit S. Transalar sphenoidal encephalocele: uncommon clinical and radiological findings. Case report. Clin Radiol. 1991, 43(1):65-67.
12. McComb JG. Neurological surgery: a comprehensive reference guide to the diagnostic and management neurosurgical problems, Youmans JR, ed 4. Philadelphia: WB Saunders, 1996: 829-841.
13. Tsutsumi K, Asano T, Shigeno T, et al. Transcranial approach for transsphenoidal encephalocele: report two cases. Surg Neurol. 1999, 51(3):252-257.
14. Cohen AR. Encephaloceles of the anterior cranial base. In Rengachary S, Wilkins R (eds): Neurosurgical operative atlas. American Association of Neurological Surgeons. Baltimore: Williams and Wilkins, 1992: 367-375.
1. Resident of the 2º Year of General Surgery of the Hospital Professor Edmundo Vasconcelos.
2. Specialist in Otorhinolaringology- SBORL. Otorhinolaringologist of the Institute Felippu de Rhinology.
3. Resident of the 3º year of Othorinolaringology of the Hospital Professor Edmundo Vasconcelos.
4. Plastic Surgeon (Specialist for the SBCP). Doctor of the Hospital Professor Edmundo Vasconcelos.
5. Associate Federal Professor University of São Paulo. Associate Federal Professor University of Director São Paulo of São Paulo ENT Center - Hospital Professor Edmundo Vasconcelos.
6. Teaching Free Professor of the FMUSP. Director of the Service of Craniomaxillofacial Surgery - Hospital Edmundo Vasconcelos Teaching Free Professor of the FMUSP.
Institution: Service of Plastic Surgery, Craniomaxillofacial and Otorhinolaryngology of the Hospital Professor Edmundo Vasconcelos. São Paulo/SP - Brazil. Mail Address: Jimmy Ayoub - 611, Martiniano de Carvalho St- Apt. 82 - Bela Vista - São Paulo/SP - Brazil - ZIP CODE: 01321-001 - Telephone: (+55 11) 5080-4000 - E-mail: jimmymed@bol.com.br. Article received on January 13, 2009. Article approved on March 15, 2009.