INTRODUCTION The loss did not properly conducted may cause language impairments, cognitive, emotional, social and educational.
The cochlear implant (CI) provides acquisition and development of listening skills and language, and its use can reduce the impact of deafness in all its aspects (1).
The selection of patients for IC is a cause of numerous studies that have expanded the situations in which observed benefits to the patient and the best indication occurs in bilateral hearing loss without adequate functional improvement with a hearing aids (HA) (1, 2 3).
The activities related to IC gained significant momentum in our country in the 90s and some groups chose to meet all the causes of deafness, with no restrictions regarding the age and place of origin of patients, extending this benefit to the entire national territory (4). Still, a large number of people with hearing loss remains without any information on opportunities available therapeutic options, nor does it seek to develop intervention are essential for proper rehabilitation.
The correct selection of patients is a major challenge for the realization of ICs. This process involves high-cost technology, need for skilled professionals and observation of all stages of evaluation (2, 3). Being a relatively new procedure in our country there are a large number of inappropriate referrals to specialized services in cochlear implant, delaying the assessment and rehabilitation of patients who would have real benefits with the use of the implant (1, 2, 3).
Based on this scenario was put into operation the site of cochlear implant (www.implantecoclear.org.br) in 2006 with the aim of universal access to those in need of a reference service in cochlear implant, select patients who possess the minimum criteria indication for evaluation as a candidate for a cochlear implant, avoiding the generation of queries and offsets and reduce unnecessary costs to the hospital to the patient and the Unified Health System (SUS). The steps for selection or rejection of patients are shown in Figure 1 flowchart.
Our objectives are:
1) Describe the profile of the group of patients with pre-and peri-lingual deafness who were not invited for evaluation by the Cochlear Implant Group and analyze the main reasons that contributed to the failure to call.
2) Assess the use of the questionnaire, its scope and application as a tool for selecting patients who seek a service specializing in cochlear implants.
METHOD The questionnaire prepared in accordance with the Protocol for Cochlear Implant Latin American (5), HC-FMUSP Protocol (6) and the experience gained through the Central Brazilian cochlear implant (CBIC) is divided into five parts: identification, three pieces of related questions the historic hearing, education and communication (Annex 1) and an area intended to describe and attach reports of examinations and additional considerations.
To complete the questionnaire is recommended to aid the responsible physician preference and / or speech therapy, monitoring the case. After analyzing the questionnaires by doctors members of CBIC is opted for calling or not calling the patient.
Between March 2006 and November 2007, eleven hundred and Fifty-eight patients have accessed the site and filled out a questionnaire. Of this total, 401 patients with pre-and peri-lingual deafness were not summoned for evaluation as candidates for cochlear implants.
Criteria used for calling or refusal of patients pre-and peri-lingual for the first consultation were established using criteria established in national and international literature and also the experience of the CBIC. Thus, for not convening of patients pre-and peri-lingual below the age of three years was adopted the following criteria: inadequate completion of the questionnaire, hearing loss is not compatible, unilateral hearing loss and anatomical impossibility. Compared to patients aged 3-9 years, exclusive, in addition to the aforementioned criteria was added to the rehabilitation inadequate and inappropriate language as criteria for not calling. For patients aged 9 years or more to the fact of not being rehabilitated by the auri-oral method was an independent criterion of failure to call besides those already mentioned above (1,2,3,5,6,7,8).
Data obtained from the questionnaires were stored in a database created in Microsoft Office Excel 2003 software.
The variables included in the database and used for the analysis of all patients were: number of automatically generated in the patient record, access date, name, sex, age at registration, education, state or country of origin, use of equipment hearing, speech therapy, type of communication used by the patient, age at onset of deafness, duration of deafness, etiology, characteristic of the progression of hearing loss, individual background and language category of the patient.
Statistical analysis of the group of patients pre-and peri-lingual not invited was performed by an ENT doctor who did not attend the initial screening, when it was decided on the invitation or not the patients.
Data analysis
The inclusion of patients in the language category of pre-and peri-lingual was based on age at onset of deafness. Thus patients were considered those with pre-lingual onset of deafness ranging from 0-2 years and those with peri-lingual onset of deafness ranging from 2 to 4 years. The answers for questions 4, 5, 6 and 12 were used to establish the differentiation mode of communication between the patients: no communication, pounds, oral communication and global communication (8). As the language reported by patients aged over three years was classified as suitable cases of patients with established communication method or predominantly aural / oral and inadequate in other types of communication (Annex 1).
The criterion anatomical impossibility, considering the cases of malformations and / or agenesis of the cochlea and auditory nerve with cochlear ossification and permeability missing according to data provided by patients in the area dedicated to the findings of examinations. The cases of mild and moderate hearing loss, conductive hearing loss and hearing loss unilateral hearing losses were characterized as not compatible.
Regarding the performance of voice rehabilitation was seen as inappropriate in cases where that was not being done to monitor speech, when this was being carried out unevenly and in situations where the patient reported having already made some kind of rehabilitation, but found to without treatment for several years. At this point, to obtain more detailed analysis of rehabilitation of the patient were also evaluated using a hearing aid, the type of communication used by the patient, duration of deafness and age at registration.
RESULTS Of 1158 patients who accessed the site during the period studied 34% represents the group of patients with pre-and peri-lingual deafness who were not summoned for evaluation.
The average age of patients pre-and peri-lingual at registration on the site was 23.6 years.
Only 1% of accesses were from patients with hearing loss are not compatible.
Epidemiological data regarding gender, place of origin, education level, aetiology, type of language and progression of hearing loss are shown in Table 1.
The distribution by age found that 54% of patients were over 17 years, 30% between 9 and 17 years, 15% between 3 and 9 years and 1% between 0 and 3 years. The duration of deafness was higher than 20 years in 50% of patients, between 10 and 20 years by 32% between 5 and 10 years in 9% and between 0 and 5 years in 9% (Graphics 1 and 2).
Over 80% of patients reported to be making or have made use of a hearing individual and 19% reported never having used. As for the performance of voice rehabilitation 58% of patients had already completed and 42% of patients never experienced any type of rehabilitation (Graphics 3 and 4).
The type of communication used by patients, according to the responses obtained in questions 4, 5, 6 and 12 of the questionnaire showed 49% with global communication, with 18% using POUNDS, 6% with oral communication, 26% with no media type and 1% no response (Graphic 5).
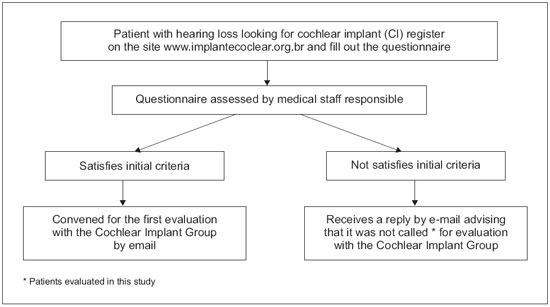
Figure 1. Flowchart .
Also significant in this study was the importance, in terms of coverage, the use of an online medical questionnaire. Within the sample studied were site access, by completing the questionnaire, for patients from all Brazilian states, except Alagoas. There was also access to a patient living abroad. This shows that in any region of the country can access the site of the cochlear implant. Few cases of patients with hearing loss are not compatible that replied and this is, at least in part to the information available on the site in terms of types of hearing loss and the indications for cochlear implantation.
A considerable portion of patients completed the questionnaire (34%) constituted the group of patients with pre-and peri-lingual deafness without minimum criteria for the call.
The average age of patients with pre-and peri-lingual deafness of 23.6 years demonstrates the predominance of an adult population of this group that sought an IC service. What reflects the difficulty encountered by the country's population, for early access to specialized centers for treatment and rehabilitation of patients with hearing loss and also the unknown of this method of rehabilitation for much of the Brazilian population and health professionals (4). Only 1% of patients in this group were aged between 0 and 3 years and it is within this age group who are the patients pre-and peri-lingual with greater potential benefit with CI (2,7).
DETTMANN et al. (2004) found that the main factors that lead to better results with the cochlear implant would be: the lowest age at implantation, shorter duration of hearing loss, greater pre-implant residual hearing, use of current technology in speech processing and communication mode approach emphasizing the aural / oral (9).
KIRK (2000) considers that the group of adolescents with hearing loss pre-and peri-lingual is the most difficult group to determine if the cochlear implant is not indicated or from the standpoint of audiological and adults with pre-lingual hearing loss are not good candidates for IC, especially if they were not properly rehabilitated for an oral communication (10). And it was precisely the group of patients pre-and peri-lingual over 17 years in the most representative number of patients in this study.
Criteria for selection of patients and refusal to perform a cochlear implant are constantly changing as the research proceeds (11,12). Any patient with severe hearing loss and / or deep it will not benefit from the use of hearing aids and not have medical or psychological contraindications for using the device may be a potential candidate for the IC (3,7,11). However the group of cochlear implant depends upon a team of doctors, audiologists, psychologists and social workers trained, specialized equipment and physical space for consultations, examinations and pre and post surgery and has a limited number of operating rooms suitable for the installation of the device at the institution where implants are performed. Thus we sought to establish the criteria for selection or rejection of patients for the first consultation, an efficient way to determine which patients are candidates with potential to be benefited by IC and prevent the convening of the cases in which the content analysis of the questionnaire clearly shows little or no chance of benefit from CI.
Criteria for selection of candidates for the IC varies according to each service may be limited to a pre-established age or be more extensive as this group of cochlear implant that has the minimum age for the procedure and 6 months as the largest maximum possible age where there are potential benefits with the use of the device (2,3,4,11).
In 2001 the Group of Latin American Research on Cochlear Implant summarized the following selection criteria for adolescents and adults pre and peri-lingual (5):
- Profound bilateral sensorineural hearing loss with limited use of hearing aids: hearing aids with thresholds equal to or greater than 65 dB HL;
- Limited test scores in speech perception in closed sets;
- Rehabilitation prior to recovery of waste with auditory development and mastery of oral communication skills and consistent use of hearing aids;
- No contraindication psychological, medical or duration.
Of the patients studied pre-and peri-lingual, there is a prevalence of 54% of patients aged above 17 years followed by 30% in the range between 9 and 17 years together has been shown that 42% of patients in this group did not perform any kind of effective speech rehabilitation, 49% of these patients had a pattern of global communication and 50% of patients had a duration of deafness over 20 years. This scenario contributed to the choice of the failure to call these patients and occurs due to the lack of centers rehabilitation in places of origin of patients and the difficulties of early access to a specialized rehabilitation and treatment of patients with hearing loss.
Among the patients' responses to question 2 of the questionnaire, an item b on the reasons for which they were not rehabilitated properly or did not perform any kind of rehabilitation were cited: the lack of resources, lack of information and lack of rehabilitation services speech near the places of origin. In contrast to the data that reflects the inadequate rehabilitation indicating that 81% of patients were doing or have already made use of HA shows that access to this type of device is already happening in most of the country, while those responsible for deploying improvements of the National Policy for Health Care Hearing the spread of diagnostic centers and hearing rehabilitation throughout the country.
Among the causes of deafness reported, the fact that 42% of patients knowing the reason for the hearing loss again reflect the difficulty to receive adequate treatment and guidance ENT. This finding is in agreement with the literature on unknown causes and raises questions about the genetic causes that are responsible for a proportion of cases of deafness which no clear etiology can be better conducted through the appropriate genetic counseling family.
Among the known causes, the finding that rubella followed by meningitis were the most frequently reported etiologies, points to the high incidence that these two diseases still present in the population with some type of hearing loss. Which raises the question about the policies adopted in the country for the prevention of infectious diseases. Important to note that one of the goals of the Pan American Health Organization (PAHO) and World Health Organization (WHO) established in 2003 proposed the elimination of rubella and congenital rubella syndrome in the Americas by 2010. In 2008, Brazil held a campaign of vaccination against rubella, this time including women and susceptible groups remaining, according to the 27th Pan American Sanitary Conference held in October 2007 in Washington, DC, USA.
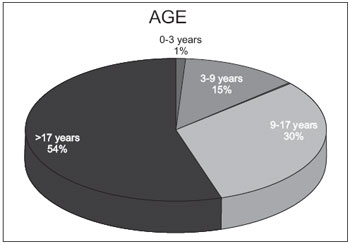
Graphic 1. Age.
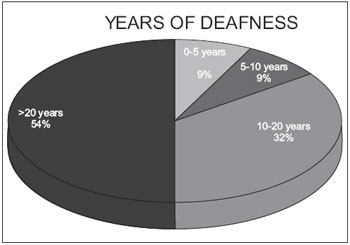
Graphic 2. Years of deafness.
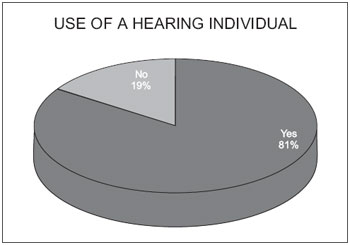
Graphic 3. Use of a hearing individual.
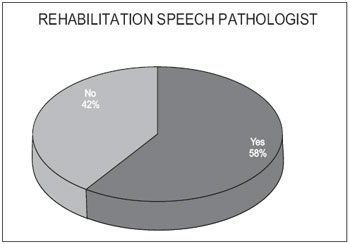
Graphic 4. Rehabilitation speech pathologist.
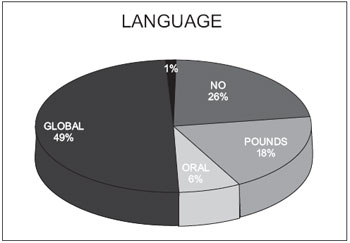
Graphic 5. Language.
The analysis of the questionnaire responses of the cochlear implant site allowed the following conclusions:
- The site proved to be a comprehensive help by providing access to a cochlear implant service for the Brazilian population;
- Most patients who sought the service specializing in cochlear implant patients is formed by pre-and peri tongue that do not have minimum criteria for appointment;
- In patients pre-and peri-lingual older age associated with deafness time high, so mostly no oral communication and lack of appropriate speech rehabilitation were instrumental in not convening.
- The questionnaire proved to be an applicable screening method for patients seeking a cochlear implant service.
BIBLIOGRAPHICAL REFERENCES1. Goffi Gomez MVS, et al. Critérios de Seleção e avaliação médica e audiológica dos candidatos ao Implante Coclear: Protocolo HC-FMUSP. Arq. Otorrinolaringol. 2004, 8(4):303-323.
2. Costa Fº AO, Bevilacqua MC, Moret ALM. Critérios de seleção de crianças candidatas ao implante coclear do hospital de pesquisa e reabilitação de lesões lábios-palatais - USP. Rev Bras Otorrinol. 1996, 62(4):306-313.
3. Bento RF, Sanchez TG, Brito RV. Critérios de indicação de implante coclear. Arq. Otorrinolaringol. 1997, 1(2):66-7.
4. Bento RF, Miniti A, Lerner A, Sanchez TG, Oshiro MS, Campos MI et al. O implante coclear FMUSP-1: apresentação de um programa brasileiro e seus resultados preliminares. Rev Bras Otorrinol. 1994, 60:Suplemento 1.
5. Protocolo Latino Americano para Implantes Cocleares. Elaborado pelo Grupo de Pesquisas Latino-americano. Cochlear Américas, 2003.
6. Goffi Gomez MVS. Programa de reabilitação fonoaudiológica no projeto implante coclear FMUSP -1. Arq. Otorrinolaringol. 1997, 1(4): 134-7.
7. Berrruecos P. Towards a better cochlear implant candidates selection in Latin American Countries. XXV International Congress of Audiology (Abstract Book). The Hague. 27-31 August, 2000.
8. Nascimento LT. Uma proposta de avaliação da linguagem oral [monografia]. Bauru: Hospital de Pesquisa e Reabilitação de Lesões lábio-Palatais, 1997. Adaptado de: Robbins AM, Osberger MJ. Meaningful use of speech scales. Indianápolis: University of Indiana School of Medicine, 1990. Arq. Otorrinolaringol., São Paulo, v.8, n.4, p. 303-323, 2004.
9. Dettman SJ, D´Costa WA, Dowell RC, Winton EJ, Hill KL, Williams S. Cochlear Implants for children with significant residual hearing. Arch Otolaryngol Head Neck Surg. 2004, 130 (May):612-618.
10. Kirk KI. Cochlear implants. new developments and results. Curr Opin Otolaryngol Head Neck Surg. 2000, 8:415-420.
11. Geers A, Brenner C, Davidson L. Factors associated with development of Speech perception skills in children implanted by age five. Ear Hear. 2003, 24(1):24S-35S.
12. Geers AE. Speech, Language and Reading Skills after early cochlear. Ear Hear. 2003, 24(1): 24S-35S.
1 ENT specialist by MEC and by ABORL / Otological Fellowship in Surgery and Skull Base. Fellow in Otological Surgery and Skull Base.
Institution: Clinical Otolaryngology John F. Leal. Guarapuava / PR - Brazil. Correspondence to: Achilles Leal Figueiredo - Rua Quintino Bocaiuva, 1248 - Guarapuava / PR - Brazil - Zip code: 85010-300 - Telephone: (+55 42) 3623-3861 - E-mail: jflorl@uol.com.br
Article received in February 1, 2010. Article accepted in March 26, 2010.