INTRODUCTION Sinonasal papilloma is a benign tumor originating from the epithelium schneiderian lateral nasal wall. Its incidence is rare and according to literature a4 accounts for 0.5% of all nasal tumors. Em1991, the World Health Organization published a classification of nasal papillomas that fall into three pathological types: inverted papilloma, exophytic papilloma (or waffle) and columnar cell papilloma or cylindrical (1). Inverted papilloma is the most common of these, about 70% of cases.
The pathogenesis remains unclear despite the suspicions of factors such as allergies, chronic infections, environmental factors and exposure to tobacco. The possibility viral caused by HPV (Human Papillomavirus) has been reported by some authors, but the results remain inconclusive (2).
Despite its benign histological factors, this tumor is known to be aggressive with local bone erosion and paranasal extension. Has a high risk of recurrence and malignant transformation of its index ranges from 0% a 9 (3, 4).
The conduct for sinonasal papilloma remains controversial. The external access via lateral rhinotomy, described by MOURE in 1902, is considered the gold standard for treatment. With the recent improvements in endoscopic techniques, endonasal resection has been cited by several authors as a surgical alternative, due to its equivalent success rate and less morbidity than external access (5, 6).
The aim of this study was to report our institution's experience in the treatment of sinonasal inverted papilloma using endoscopic approach and compare the results with the literature.
METHOD Was carried out a review of records of all patients diagnosed with sinonasal papilloma treated at the Otorhinolaryngology, Hospital das Clinicas, Federal University of Bahia (UFBA), from January 2004 to May 2010. The follow up ranged from 12 months to 5 years. To increase the reliability of this study, all data were collected by the same author.
Patients with endoscopic evidence of unilateral nasal tumor, histological diagnosis of sinonasal papilloma (surgical) resection of the tumor by endoscopic sinus surgery and outpatient minimum of 12 months postoperative.
Being excluded patients aged less than 18 years, history of prior sinus surgery, CT scan with signs suggestive of associated malignancy (bone destruction with invasion of adjacent structures such as the CNS and the orbit).
Was evaluated in this study, the patient's sex, origin of the lesion, side of tumor, presence of recurrence, an association of malignancy and treatment.
All patients were classified according to the criteria proposed by KROUSE (7) for sinonasal papilloma (Table 1).
The treatment was always surgical, aiming at complete removal of the mass and the periosteum in the region of insertion of the tumor. All patients were advised of the possibility of using an external access Deputy depending on the severity and location of injury.
This study was approved by the Ethics Committee of the Federal University of Bahia (UFBA).
RESULTS This study included 12 patients with histological diagnosis of inverted papilloma. The prevalence of male ratio of 2:1 (Figure 1) and the mean age of patients was 51.25 years (range A73 de29 years). The incidence on the left side was 66.6% of cases (8 patients) and right side, 33.3% (4 cases). The postoperative follow-up ranged shape12 A60-month average of 23 months.The most common site of origin of the injury was the maxillary sinus in 6 cases representing 50% of the total (Table 2).
Considering the preoperative computed tomography, and based on the classification proposed by Krouse, the T1 group contained four patients (33.4%), group T2, five patients (41.6%) and T3 group, 3 patients (25%) . There was no patient be in group T4 (Figure 2).
Only one case of recurrence (8.3%), which is 12 months after surgery. There was no malignant transformation in multiple sclerosis patients.
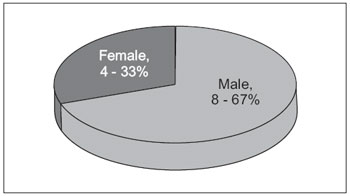
Figure 1. Patient gender.
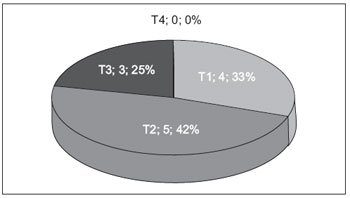
Figure 2. Staging of the tumor.
The incidence of sinonasal papilloma is higher in males and usually occurs between the 5th and 6th decades of life (8), a fact confirmed in our study. The literature states that the tumor is usually unilateral, as in this study, and no preponderance for left or right side.
The staging system proposed by KROUSE (7) is commonly used because it correlates the prognosis of sinonasal papilloma with its difficulty of treatment. This rating in turn is limited to the fact that overrides the presence of malignant transformation of tumor extension. The preoperative evaluation of the extent and location of tumor is extremely important for proper planning of surgical access to be chosen. This evaluation usually consists of endoscopic examinations and imaging. The endoscopy allows the examiner to show the location of the lesion and the presence of other pathologies such as polyps and sinusitis. A CT scan should always be investigated, because it assesses well the anatomy and adjacent bone erosion (10). However, it may overestimate the extent of disease due to lack of differentiation between tumor and inflammatory areas or retained secretions. MRI can make this differentiation, but has high cost and does not differentiate papilloma malignant tumor. In this series of 12 patients were combined endoscopy and computed tomography.
The main goal of treatment is complete surgical removal of the lesion on direct visual control with minimal morbidity. The endoscopic surgery through was initially used for treatment of minor injuries, however, with advancing technology, the criteria for its use are expanding. Several authors have advocated treatment by endoscopic approach in recent literature and have reached recurrence rates comparable to treatment via external access. BUSQUETS and HWANG (11) performed a meta-analysis to compare recurrence rates in patients treated via endoscopic or external access. The cohort group consisted of 1060 patients, of whom 714 were treated endoscopically and 346 via non-endoscopy. The authors found a lower recurrence rate (12%) in the first group compared to the second group (19%).
LAWSON et al in an analysis of 40 cases, found a recurrence of 5.8% in 17 patients treated with pure endoscopic access and 17% in 23 patients treated with combined access (14).
MORTUAIRE et al found a recurrence of 15.8% in patients who underwent external access, 17.6% for the purely endoscopic and 8.3% with combined access.
In our study, the recurrence rate in patients treated via a purely endoscopic access was equivalent to current publications. In our experience this success rate is due to the care team to achieve visualization and complete resection of the tumor and insertion of the periosteum. In our series only one patient had a relapse, which occurred after twelve months, and in this location than the original. The same was submitted to a new endoscopic surgical procedure and is more than two years without any warning signs of relapse. In literature we can find cases of recurrence with up to 56 months (12) which demonstrates the importance of a prolonged endoscopic follow up after surgery for a diagnosis and early intervention of relapses.
A great debate is still on the choice of adequate access to treatment for each type of sinonasal papilloma. There is no consensus among the authors who set exact values for choice of surgical approach. What is observed in the studies is a tendency for endoscopic early stages of KROUSE and access combined in more advanced stages or in recurrences. Should be taken into account the clinical and radiographic pre-operative and surgeon experience. As an example, lesions confined to the nasal cavity are predominantly treated by endoscopic approach, however, stretches the sinus sometimes need combined procedures such as Caldwell Luc, rhinotomy lateral mid-facial degloving, osteoplastic flap and others.
Several advantages have been reported when comparing the technique with purely endoscopic techniques for external access. Among these advantages we can mention: less surgical time, less bleeding, shorter hospital stay, no scarring, preservation of anatomical structures, etc. (13).
The rate of malignant transformation in the literature varies from 0% a9 and is consistent with our results.
CONCLUSION The treatment of inverted papilloma has been largely benefited from the advances in endoscopic techniques, with recurrence rates equivalent to those reported for external access.Imaging exams are essential in preoperative planning and decision-making technique. The key to the success of this treatment is the meticulous identification and removal of the lesion on his site from external access inserção.Um combined, however, is necessary depending on the extent of lesion, its insertion site and in cases of malignant transformation. A regular follow-up and long term is essential for a good monitoring developments.
BIBLIOGRAPHICAL REFERENCES1. Mackle T, Chambon G, Garrel R, Meieff M, Crampette L. Endoscopic treatment of sinonasal papilloma: a 12 year review. Acta Oto-Laryngologica. 2008, 128:670-674.
2. Buchwald C, Larsen AS. Endoscopic surgery of inverted papillomas under image guidance, a prospective study of 42 consecutive cases at a Danish university clinic. Otolaryngol Head and Neck Surg. 2005, 132(4):602-607.
3. Lawson W, Ho BT, Shaari CM, Biller HF. Inverted papilloma: a report of 112 cases. Laryngoscope 1995, 105:282-8.
4. Katori H, Tsukuda M. Staging of surgical approach of sinonasal inverted papilloma. Auris Nasus Larynx. 2005, 32:257-63.
5. Yiotakis J, Hantzakos A, Kandiloros D, et al. A rare location of bilateral inverted papilloma of the nose and paranasal sinuses. Rhinology. 2002; 40:220-222.
6. Krouse JH. Endoscopic treatment of inverted papilloma: safety and efficacy. Am J Otolaryngol. 2001, 22:87-99.
7. Krouse JH. Development of staging system for inverted papilloma. Laryngoscope. 2000, 110:965-968.
8. Mendenhall WM, Hinerman RW, Malyapa RS. Inverted Papilloma of the Nasal Cavity and Paranasal Sinuses. Am J Clin Oncol. 2007, 30:560-563.
9. Kraft M, Simmen D, Kaufmann T, Holzmann D. Long-term results of endonasal sinus surgery in sinonasal papillomas. Laryngoscope. 2003, 113:1541-7.
10. Sachs ME, Conley J, Rabuzzi DD, Blaugrund S, Price J. Degloving approach for total excision of inverted papillomas. Laryngoscope. 1984, 94:1595-8.
11. Busquets JM, Hwang PH. Endoscopic resection of sinonasal inverted papiloma: a meta-analysis. Otolaryngol Head Neck Surg. 2006, 134:476-482.
12. Schlosser RJ, Mason JC, Gross CW. Aggressive endoscopic resection of inverted papilloma: an update. Otolaryngol Head Neck Surg. 2001, 125-49-53.
13. SautterNB, Cannady SB, Citardi MJ. Comparison of open versus endoscopic resection of inverted papilloma. Am J Rhinol. 2007, 21:320-323.
14. Lawson W, Patel ZM. The evolution of management for inverted papilloma: An analysis of 200 cases. Otolaryngol Head Neck Surg. 2009, 140, 330-335.
15. Durucu C, Baglam T, Karatas E, Mumbuc S, Kanlikama M. Surgical treatment of inverted papilloma. J Craniofac Surg. 2009, 20:1985-1988.
1 Resident Physician in the second year of Otorhinolaryngology.
2 Resident of Otolaryngology at University Hospital Professor Edgard Santos UFBA - 3rd Year.
3 Doctor, Doctor ENT. Research Associate in the Department of Otolaryngology and Immunology at the University Hospital Professor Edgard Santos UFBA.
4 Doctor, Doctor ENT. Professor and Head, Department of Otorhinolaryngology, University Hospital Prof. Edgard Santos.
5 Otorhinolaryngologist. Fellow in the Department of Otorhinolaryngology, University Hospital Professor Edgard Santos UFBA.
Institution: Department of Otolaryngology, Hospital das Clinicas, Federal University of Bahia. Salvador / BA - Brazil. Mail Address: Luana Alves de Souza - Rua Dr. Clemente Ferreira, 139, Apt. 101 - Canela - Salvador / BA - Brazil - Zip code: 40110-200 - Telephone: (+55 71) 9606-2333 - E-mail: lua_goias@hotmail.com
Article received on February 14, 2010. Article accepted on July 11, 2010.