INTRODUCTIONThe nasal septum correction surgery (septoplasty) septoplasty began in the 19th century, and it has been modified and enhanced ever since. The used techniques have tried to give as much as functional and respiratory improvements, preserving other physiological nose aspects (1). The hypertrophy in the inferior conchae can also cause a nasal obstruction (2).
Several surgical techniques are available to treat the concha hypertrophy, including the partial or total turbinectomy, submucosal or extramucosal electrocautery, and resection by radiofrequency, laser or cryosurgery (3). Nowadays, there is no agreement in literature indicating the most suitable technique to reduce nasal conchae (3).
The nasal pack has been used to control primary bleeding in patients submitted to nasal surgery (4-7). Besides, the pack is used to stabilize the cartilaginous-osseous structure of the nose and avoid complications in the post-surgical period, such as septal hematoma, infection, abscess development and drilling (4-8)
Several complications have been related to the nasal pack, as vasovagal reflex, (arrhythmia, hypotension and apnea), allergy, toxic shock syndrome, Eustachian tube, dysfunction, infection and respiratory disorders (4-6). The patients also complain about some pack-related discomfort and pain (4-7,9,10).
There are several types of materials to carry out the nasal pack, out of which the most used are: Gelfoam®, gauze with petrolatum or paraffin; Surgicel®; Merocel®; protective sheath (4-8). Some studies have investigated the efficiency of the nasal pack to control bleeding and complications after septoplasty (4-6,9). However, a few studies evaluate the efficiency of the nasal pack in patients submitted to septoplasty with bilateral inferior partial turbinectomy.
This work has the objective to compare the degree of nasal bleeding among patients submitted to septoplasty with partial bilateral inferior turbinectomy, whether using the nasal pack or not.
METHOD60 patients served at the otorhinolaryngology ambulatory of tertiary hospital in the city of São Paulo, diagnosed of nasal septum deviation and inferior conchae hypertrophy, were evaluated. The patients were submitted to a clinical treatment with antihistaminic and topic corticosteroids, without showing an improvement in the symptoms, hence a septoplasty with bilateral inferior partial turbinectomy was performed. Successive surgical procedures were performed in the period from May 2009 to June 2010. The project was assessed and approved by the Research Ethics Committee of the Institution (Resolution nº 19/2010).
This work included the patients presenting the nasal septum deviation with symptoms of chronic nasal obstruction (unilateral or bilateral) and with symptoms remaining until 02 months after the clinical treatment (topical corticosteroids with or without antihistamines) associated with inferior nasal conchae hypertrophy.
Patients presenting the following symptoms were excluded from this work: septoplasty associated to nasosinusal surgery; nasosinusal tumors; chronic rhinosinusitis; rhinoplasty, head and neck radiotherapy; nasal septum drilling; nasal valve insufficiency ; nasosinusal granulomatous disease; pharyngeal tonsil hyperplasia; snoring surgery; craniofacial malformation; and pregnancy.
A longitudinal study of prospect cohort type was performed, in which the patients submitted to septoplasty and bilateral inferior partial turbinectomy were evaluated with respect to the intensity of the post-surgical nasal bleeding. The inferior nasal conchae were classified as: normotrophy, slight hypertrophy (degree 1), moderate hypertrophy (degree 2) and severe hypertrophy (degree 3). A reduction of the nasal conchae was performed in patients with degree-2 hypertrophy (36 patients) and degree-3 hypertrophy (24 patients). The bleeding intensity was scaled from 1 to 4, as follows:
1- there was no bleeding;
2- minimum bleeding, and it stopped spontaneously
3- bleeding required a vasoconstriction; and
4- nasal packing needed.
The surgical procedures were performed with general anesthesia in association with a submucosal infiltration of septum with lidocaine 20% and norepinephrine 1:80.000 a few minutes before the incision. Modified Cottle technique was used to correct the nasal septum deviation (1). For the surgical treatment of the inferior nasal concha, the bilateral inferior turbinectomy technique was used with direct visualization (1,11). The surgeries were performed by resident doctors in the second year guided and supervised by assistant doctors of the Institution.
After surgery, the sample was divided into 02 groups: patients using and patients not using the nasal pack. About the use of nasal packs, it was decided during surgery, in accordance with the bleeding degree. Two kinds of nasal packs were used: Merocel® (15 patients) and protective sheath (5 patients). The nasal splint was used in 57(95%) patients for a period ranging from 07 to 10 days. In the post-surgical period and after the pack was removed, the patients were told to wash their nose with a cephalexin-associated physiologic solution for 07 days.
In order to compare the groups (with and without the nasal pack) in accordance with bleeding degree, Chi-square test was performed. p<0,05 was considered significant.
RESULTSThe sample of this study was comprises of 60 patients submitted to bilateral partial inferior turbinectomy being 26(43,3%) of female gender and 34(56,6%) male gender. The average age was 34.8 years, varying from 9 to 68 years. The nasal pack was used in 20 (33,3%) patients and not used in 40 (66,6%), as can be observed in table 1. The time length using the pack was 31.3 hours, ranging from 24 to 72 hours.
It was observed that the post-surgical bleeding degree of the group submitted to partial bilateral inferior turbinectomy, who used the nasal pack, was lower, with a statistically significant difference (p=0.014) than in the group not using the pack.
None of the patients using the nasal pack showed any complications. The complications observed after surgery occurred in patients who did not use the nasal pack (10%), among whom two developed acute rhinosinusitis (5%), one with vestibular retraction (2.5%), and one with nasal vestibulitis (2.5%).
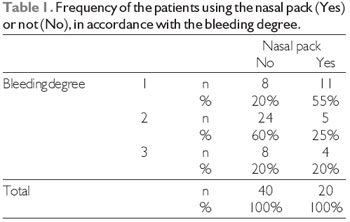
Legend: n = frequency; Chi-square test (p)=0,014.
The surgery to correct nasal septum deviation (septoplasty) and reduce nasal conchae has been modified and enhanced in the last few years (1). These changes are important to achieve better results in the post-surgical period, as well as make the surgery less painful and uncomfortable on the patient.
In the last years, it has been investigated the requirement to use the nasal pack after surgery in patients submitted to the nasal surgery (5,8). Discomfort and pain have been some of the factors contraindicating its use (5, 8, 9, 12). Recent studies indicate that the nasal pack significantly contributes to post-surgical pain (7,9). Pain can be caused by misplacing the blood coagulum, as well as the adherence of the traditional packs to the nasal mucosa, and removing the nasal pack is frequently the most uncomfortable part and annoys the patients submitted to septoplasty.
The nasal pack is used to prevent hemorrhage, septal hematoma and synechias (4, 6, 8). Some works have demonstrated that there is no difference in relation to complications among patients using and not using the pack (4-6,9). In this study, it was observed that the post-surgical complications occurred in patients who did not use the nasal pack (10%), in contrast with most studies that showed there is no difference between using the pack or not (4-6). AWAN et al demonstrated that the patients using the nasal pack had a higher rate of cephalea, epiphora, dysphagia and sleep disorders in relation to patients not using the pack, but there was no difference between the groups, when such complications as follows were evaluated: Septal hematoma, synechia and infection (9).
Most studies evaluate the efficiency of the bleeding control by using the nasal pack in patients submitted to septoplasty separately, and it is almost a common sense that there is no advantage to use the pack (4-6,9). However, we did not find works comparing the bleeding intensity in the patients submitted to septoplasty associated with turbinectomy and the nasal pack.
In this study, it was observed that the post-surgical bleeding intensity in the patients submitted to septoplasty with bilateral partial inferior turbinectomy was lower than in the patients using the pack (Table 1). However, in accordance with the classification used in this study, the bleeding served in most patients of the group without the nasal pack showed a spontaneous resolution (60%), and the rest did not bleed (20%) or stopped only with vasoconstrictors (20%), and it was not necessary to use the nasal pack. Therefore, although the highest bleeding rate in patients of the group without the pack, it was not necessary to make them uncomfortable and cause other complications related to the pack.
LUBIANCA-NETO et al suggest that there is difference in relation to the post-surgical bleeding between the patients using the pack for 24 hours and the ones using the pack for 48 hours (6). Therefore, it is not reasonable to use the pack for longer than 48 hours in all the patients but those with a high risk of bleeding (6).
CONCLUSION The patients submitted to septoplasty with partial bilateral inferior turbinectomy, not using a post-surgical nasal pack, appeared to bleed more than patients using a nasal pack.
BIBLIOGRAPHICAL REFERENCES1. Maniglia AJ, Maniglia JJ, Maniglia JV. Indicações e técnicas cirúrgicas de septoplastia. Em: Maniglia AJ, Maniglia JJ, Maniglia JV. Rinoplastia - Estética-Funcional-Reconstrutora. Rio de Janeiro: Revinter; 2002.
2. Stewart MG, Smith TL, Weaver EM, Witsell DL, Yueh B, Hannley MT, Johnson JT. Outcomes after nasal septoplasty: results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 2004, 130:283-90.
3. Bhandarkar ND, Smith TL. Outcomes of surgery for inferior turbinate hypertrophy. Curr Opin Otolaryngol Head Neck Surg. 2010, 18:49-53.
4. Ardehali MM, Bastaninejad S. Use of nasal packs and intranasal septal splints following septoplasty. Int J Oral Maxillofac Surg. 2009, 38:1022-4.
5. Basha SI, Gupta D, Kaluskar SK. Routine nasal packing following nasal surgery - is it necessary? Indian J Otolaryngol Head Neck Surg. 2005, 57:69-71.
6. Lubianca-Neto JF, Sant'Anna GD, Mauri M, Arrarte JLF, Brinckmann CA. Evaluation of time of nasal packing after nasal surgery: a randomized trial. Otolaryngol Head Neck Surg. 2000, 122:899-901.
7. Chheda N, Kartz AE, Gynizio L, Singer AJ. The pain of nasal tampon removal after nasal surgery: a randomized control trial. Otolaryngol Head Neck Surg. 2009, 140:215-7.
8. Berlucchi M, Castelnuovo P, Vincenzi A, Morra B, Pasquini E. Endoscopic outcomes of resorbable nasal packing after functional endoscopic sinus surgery: a multicenter prospective randomized controlled study. Eur Arch Otorhinolaryngol. 2009, 266:839-45.
9. Awan MS, Iqbal M. Nasal packing after septoplasty: a randomized comparison of packing versus no packing in 88 patients. Ear Nose Throat J. 2008, 88:624-7.
10. Bresnihan M, Mehigan B, Curran A. An evaluation of Merocel and series 5000 nasal packs in patients following nasal surgery: a prospective randomized trial. Clin Otolaryngol. 2007, 32:352-5.
11. Sampaio PL, Galindo C, Voegels RL. Tratamento Cirúrgico das Conchas Nasais. Em: Campos CAH, Costa HOO. Tratado de Otorrinolaringologia. 1º Ed. São Paulo: Editora Roca; 2003, vol 5, pp. 260-8.
12. Bajaj Y, Kanatas AN, Carr S, Sethi N, Kelly G. Is nasal packing really required after septoplasty? Int J Clin Pract. 2009, 63:757-9.
1 Resident Doctor (R3) at HSPM's Otorhinolaryngology Department.
2 Doctor in Sciences from University of São Paulo. Post-Doctorate from University of São Paulo. Assistant Doctor at HSPM's Otorhinolaryngology Department.
3 Resident Doctor (R2) at HSPM's Otorhinolaryngology Department.
Institution: São Paulo's Municipal Civil Servants Hopsital (HMSP). São Paulo / SP - Brazil. Mailing address: Leandro Castro Velasco - Rua Antônio Alves Martins, 150 - Bairro: Lucilene - Santa Helena de Goiás / GO - Brazil - ZIP Code: 75920-000 - Telephone: (+55 64) 3614-1639 - Email: lcvelasco@hotmail.com
Article received on November 5, 2010. Article approved on February 5, 2011.