INTRODUCTIONThe Otoacoustic Emissions (OAE) are subliminal sounds arising from the external acoustic meatus, when the tympanic membrane receives vibrations from the cochlea transmitted by the middle ear (1). These vibrations occur as a sub-product of a specific and vulnerable cochlear mechanism renowned as the cochlear amplifier, which significantly contributes to the auditory sensitivity and the discrimination of frequencies (2).
In the clinical practice, the OAE can be spontaneously registered or acoustically evoked by a transient stimulus or a product of distortion (3).
The evoked OAEs are registered for most individuals showing a normal cochlear function, apart from their age and sex. Its presence indicates the integrity of the external celiac cells of cochlea (4).
To capture the OAE, there needs to be the integrity of middle and external ears, because any change in the transmission of the acoustic stimulus can lead to a reduction or absence of response, jeopardizing the exam analysis (5).
In the clinical practice, it is possible to observe an association between the reduction in the levels of emission responses or even an absence of responses in patients who showed changes in the middle ear (6).
The most common causes of changes in the child's middle ear are related to tympanic drilling, infection or a liquid in the middle ear and more recently the gastroesophageal reflux disease has been included, which can significantly contribute to the inflammation of the middle ear and participate in the physiopathology of effusive otitis as a result of the action of the pepsinate acid and the pepsinogen (7, 8).
The gastroesophageal reflux disease (GERD) is more frequent in the first months of life. The post-alimentary regurgitations appear between birth and four months of age, showing a spontaneous resolution, in most of cases, until one or two years of age (9, 10).
GERD was classified as physiological in infants aged between one and twelve months, when they showed two or more regurgitation episodes daily within a period longer than three weeks, without a history of hematemesis, bronchoaspiration, apnea, pondero-statural deficit or abnormal postural (11).
The regurgitation tends to naturally disappear within 12 months; however, it does not mean that the reflux is no longer present, because in approximately 5% of the cases the continuance of a reflux without regurgitation can cause otorhinolaryngological symptoms, such as: laryngitis, otitis and sinusitis (12).
Due to the short quantity of works about the otoacoustic emissions evoked in GERD babies and the need to perform this evaluation in the neonatal auditory screening (NAS), the objective of this study was to analyze the occurrence of the response levels of the acoustic emissions evoked by transient stimuli in infants with a physiological GERD.
METHODCollection started after the Ethics Committee of the State University of Health Sciences of Alagoas UNCISAL approved under the Protocol Nº 583. Prospective study performed at the Santa Juliana Hospital's Department of Otorhinolaryngology, Maceió, Alagoas (Municipal Philanthropic Institution) and complies with the National Health Council's resolution Nº 196/96. The Free and Clarified Term of Agreement was read and explained to those responsible for the infants, who agreed and signed.
The sample was comprised of 118 6-month-old infants of both sexes, prematurely or timely born, divided into two groups: Study group (SG), consisting of 63 infants clinically diagnosed of reflux by gastroenterologists or pediatricians. This diagnosis was made by a form based on the ROMA II criterion reporting the GERD symptoms. When at least two symptoms were identified, the baby was included in the group with physiological gastroesophageal reflux. Infants with pathological reflux were not identified. The control group (CG) was comprised 55 infants without reflux, matched by age, sex and gestational age.
The study group with reflux was composed of 36 female children and 27 males, and the group without reflux of 30 female children and 25 males. And in relation to gestational age (born timely or prematurely), the group with reflux was formed by 18 prematurely born children and 45 timely born children; in the group without reflux, 16 children were prematurely born and 39 were timely born.
Infants with cleft lip and palate or bad formation of the external and/or middle ear, bad formation of head and neck, genetic syndromes associated with auditory changes, children with family history of hearing loss and neurological changes and bronchopulmonary dysplasia were excluded.
The size of the sample was calculated by the software named Statcalt Epi info, version 6.04. Where an alpha and beta error of 5% was assigned, a value of minimum sample of 82 infants was achieved.
To analyze the GERD in relation to the analysis of the width and the signal/noise ratio of TEOAE, the Mann-Whitney test was used; and to associate the drug in the TEOAE occurrence, the Chi-square test was used for independence.
An otorhinolaryngological evaluation was performed in all the individuals by means of otoscopy in order to verify the integrity of external and middle ear
Transient-Evoked Otoacoustic Emissions (TEOAE) was performed by the researcher responsible in an otorhinolaryngological center in an environment with a low level of noise and with the infant in a state of natural sleep in his/her mother's lap. The tests were performed by using the Interacoustic otoRead Interacoustic equipment, which allows otoacoustic emissions to be recorded by placing a probe (with attached microphone) in the external acoustic meatus.
As a criterion for analysis, the PASS/FAIL parameter described in the protocol of the equipment with stimulus was used: click; intensity: 83 dBpeSPL; number of frequency bands tested: 6 (of 1500Hz to 4000Hz). The values to be considered PASS test were: Emissions present in a signal/noise ratio of 4 dB in at least three frequency bands. The capturing time of the OAE in the equipment is as long as 64 seconds, and it can automatically stop before the time is ended when the result is considered present.
The two evaluations (otoscopy and TEOAE) were conducted separately, but on the same day, when the examiners were unaware of the results of this evaluation, before all tests had been completed.
RESULTSThe results will be presented by comparing the groups with and without GERD in the distribution of relative frequency (percentage) of the qualitative variables.
The occurrence of TEOAE in both groups are described in Graphics 1 and 2.
When comparing the results of the occurrence of TEOAEs between groups, we observed a higher prevalence of TEOAE in the group without reflux. However, it was also possible to observe that even in the group with reflux, there was a higher incidence of TEOAE present in comparison with the absent results.
When analyzing the occurrence of drugs in the group with reflux, it was observed that 81% of the GERD group had never used any drug.
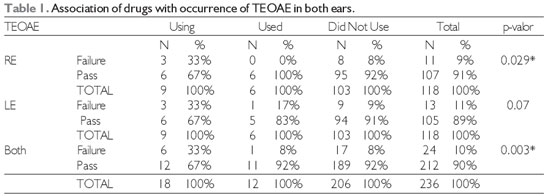
Regarding the association of medication with the occurrence of TEOAE, the results described in Table 1 were observed. The statistical test used for this analysis was the Chi-Square.
It was verified that there was a statistically significant association between drugs and the results of TEOAE in both ears, as well as in the right ear. There was a statistically significant difference in infants who have used drugs from those who did not. The infants using the medication showed a greater percentage occurrence of failure in TEOAE in comparison with the other failure percentage of infants who have already used of or have never used the drug.
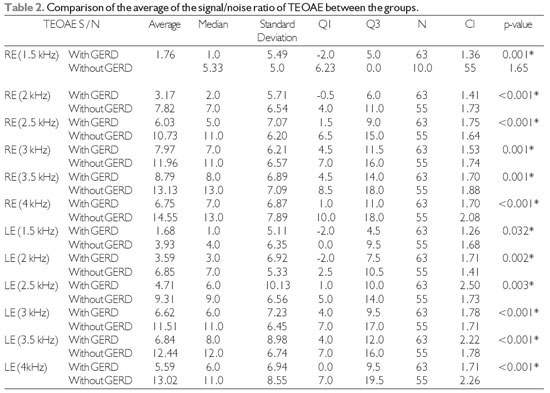
To evaluate the signal/noise ratio of the TEOAE in both groups, we used the Mann-Whitney test and the results are observed in Table 2.
There was a statistically significant difference between the groups for all frequency bands in both ears. That is, in the control group, group without reflux, the signal/noise ratios achieved in the TEOAE were statistically significant higher than those obtained in the group with reflux. The highest average signal/noise ratio was found in the frequency band of 4 kHz in both ears, with average values of 14.55 dB ± 2.08 dB in the RE and 13.02dB ± 2.26 in the LE.
The results of average levels of responses of TEOAE in the frequency bands studied in both ears are described in table 3. In this analysis, we used the Mann-Whitney test.
It was possible to observe that the average responses levels of TEOAE were higher in the group without reflux for the frequency bands of 2kHz, 2.5kHz, 3kHz, 3.5kHz, 4,kHz, and 4.5kHz bilaterally, with a statistically significant difference. Only in the frequency of 1.5 kHz in both ears, there was no statistically significant difference between the groups. The highest average TEOAE levels were 7.71 dB and 7dB found in the frequency band of 2 and 4 kHz, respectively, in the RE of the group without reflux.
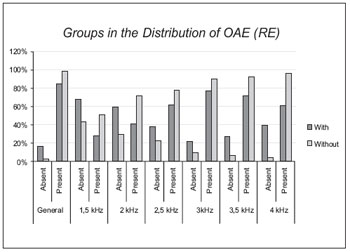
Graphic 1. Comparison of groups when distributing the occurrence of OAE in the RE.
Legend: RE: right ear; OAE: otoacoustic emissions; with: group with GERD; without: group without GERD.
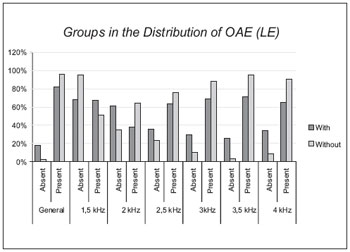
Graphic 2. Comparison of groups when distributing the occurrence of OAE in the LE.
Legend: LE: left ear; OAE: otoacoustic emissions; with: group with GERD; without: group without GERD.
In the analysis of the TEOAE in the groups studied (Graphics 1 and 2), a greater occurrence of responses was noticed in the group without reflux, however a high prevalence of responses were also noticed in the group with reflux in the frequency bands of 1.5; 3 and 3.5kHz. This finding disagrees with the study that observed OAEs in only 2 and 4 kHz frequencies in children with secretory otitis media (13).
In the analysis of TEOAE occurrence with the use of drugs by infants in the group with reflux (Table 1), it was noted that the majority of infants who were using drugs failed more in TEOAE in comparison with the infants who never used medication, with a statistically significant difference. Because GERD can cause a change in the middle ear (9.10) and this, in turn, interferes with TEOAE, it is possible that the absence of responses in the group who used drugs occurred because of the most critical period of GERD, i.e., exaggerated vomiting, which, in turn, can cause the Eustachian tube dysfunction and lead to changes in the middle ear (10, 12, 14, 15, 16).
Studies reported that treatment of GERD improves otorhinolaryngological symptoms (10, 17, 18). This may explain the high prevalence of TEOAE in infants who had already made use of drugs in comparison with those still using them. The OAEs are present in the functionally normal ears and they are no longer captured when presenting thresholds above 30dBNA or a modification of the middle ear. (1, 2, 4, 6)
When the levels of the signal ratio were analyzed by frequency band (Table 2) by comparing the groups, a statistically significant was observed in all frequency bands: The group with reflux had lower levels of signal to noise ratio.
It was possible to note that the highest levels of signal-to-noise ratio of TEOAE occurred in frequency bands of 3 and 4 kHz, in the group without reflux in both ears and in the bands of 3 and 3.5kHz in the group with reflux. A study with 100 newborns found spontaneous OAE with a greater concentration on the frequency bands of 3 and 4 kHz bilaterally, in the timely newborns and without risk indicators. This may justify greater a signal to noise ratio in these frequency bands. Another study reports that the newborn OAE is always higher in acute frequency bands due to the anatomy of the ear, and it is important to detect hearing loss (3, 4, 6, 19).
The signal/noise ratio is one of the evaluated analyses in the TEOAE pass/fail criteria and so that it can be considered as pass, the integrity of the middle ear is necessary to better capture this relationship, thus avoiding false positive results (20).
When comparing the response levels of the TEOAE (table 3), it was possible to observe that the group without reflux presented more answers in the frequency bands of 2 to 4 kHz, with a significant difference when compared to the group with reflux. These findings corroborate with studies that found a higher TEOAE width at high frequencies and lower width at low frequencies (21, 22), and it can be connected with the increase of the width of these frequencies, the spontaneous OAE that occurred between 3 and 4 kHz (23) .
Studies have reported that the average ear of neonates is dominated by mass and by low resonance frequency (24) and that the resonance frequency of effusive ears occurs in 858Hz with a standard deviation of 483Hz (25) and that the change in the middle ear impairs the magnitude of the OAE (26).
By analyzing the groups separately, it was possible to observe that in both there was in a higher prevalence of TEOAE. One fact that stands out is that even with TEOAEs present, a decrease in TEOAE width was observed in the group with GERD in comparison with those without reflux. Studies (7, 8, 25, 26) reported that the GERD may contribute to the inflammation of the middle ear and that this results in a significant reduction of the TEOAE response.
Legend: * P-value <0.05. Legend: TEOAE: transient-evoked otoacoustic emission; RE: right ear; LE: left ear.
Legend: *p-value: 0.05; TEOAE: transient-evoked otoacoustic emission; RE: right ear; LE: left ear.
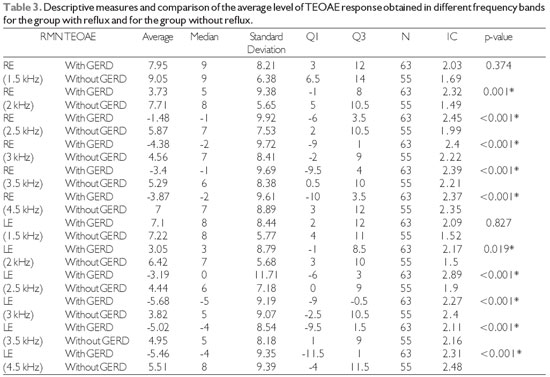
Legend: *p-value<0.05. Legend: TEOAE; RMN: Average level of the responses of transient-evoked otoacoustic emissions; With GERD: with gastroesophageal disorder; Without GERD: without gastroesophageal disorder
There was a significant decrease in the occurrence and levels of response of the transient-evoked otoacoustic emissions in infants with physiological gastroesophageal reflux when compared to children without reflux.
REFERENCES1. Kemp DT. Otoacoustic emissions, their origin in cochlear function, and use. British Medical Bulletin. 2002, 63:223-241.
2. Kemp DT, Bray P, Alexander L, Brown AM. Acoustic emission cochleography; pratical aspects. Scand. Audiol. Suppl. 1986, 25:71-85.
3. Gattaz G, Cerruti VQ. O uso do registro de emissões otoacústicas evocadas para triagem auditiva em neonatos de risco para deficiência auditiva. Revista Paulista de Pediatria. 1994, 12(3):291-4.
4. Pialarissi PR, Gattaz G. Emissões otoacústicas: conceitos básicos e aplicações clínicas. Rev Arquivos da Fundação Otorrinolaringologia. 1997, 1(2):13-6.
5. DellAringa Alfredo R, DellAringa Ana Helena Bannwart, Juares Antônio JC, Melo Cinthia de, Perches Filho Renato M.Emissões otoacústicas por produtos de distorção em crianças de 2 a 7 anos. Rev. Bras. Otorrinolaringol. [serialontheInternet]. 2004 June [cited 2010 Oct 18], 70(3):380384. Availablerom: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-72992004000300014&lng=en.doi:10.1590/S0034-72992004000300014.
6. Choi SS, Pafitis IA, Zaizal GH, Paterl KM. Clinical Applications of transienty evoked otoacustic emissions in the pediatric population. Ann Otol Rhinol Laryngol. 1999, 108:132-8.
7. Tasker A, Dettmar PW, Panetti M, Koufman JÁ, Birchall JP, Pearson JP. Is gastric reflux a cause of otitis media with effusion in children? Laryngoscope. 2002, 112(11):1930-1934
8. Crapko M, Kerschner JE, Syring M, Johnston N. Role of extra-esophageal reflux in chronic otitis media with effusion. Laringoscope. 2007, 117:1419-23.
9. Carré IJ.The natural history of partial thoracic stomach (hiatus hernia) in children. Arch Dis Child. 1959, 34:344-53.
10. Shepherd RW, Wren J, Evans S, Ong TH, Lander M. Gastroesophageal reflux in children; clinical profile course and outcome with active therapy in cases. Clin Pediatr. 1987, 26:55-60
11. Roma Foundation.org [home page the internet]. McLean, VA: Roma Foundation Introduces Diagnostic Algorithms for Common Gastrointestinal Symptoms, Inc.; c2009 [updated 2009 Fev 10; cited 2009 Mar 9]. Avaliable from: http://www.romecriteria.org > acesso em: 18 agosto de 2010 às 21:00 horas.
12. Pediatric Gastroesohpageal Reflux Clinical Practice Guidelines were published in the Journal of Pediatric Gastroenterology and Nutrition 2001; Volume 32: Supplement 2 pages 1-31. Complete or: www.cdhnf.org or www.naspghan.org > acesso em: 05 julho de 2010 às 23:34 horas .
13. Van Cauwenberge PB, Vinck BM, De Vel E, Dhooge I. Tympanometry and click evoked otoacoustic emissions in secretory otitis media: Are c-eoae really consistently absent in type b tympanograms. Sixth international symposium on recent Advance in otitis media. 1995 June; Ft. Lauderdale, FL.
14. Quintella T. Refluxo gastroesofágico e doença otorrinolaringológica na infância. In: Sih T e col. Otorrinolaringologia Pediátrica. Rio de janeiro: Revinter, 1998. p.17-21.
15. Velepic M, Rozmanic V, Velepic M, Bonifacie M. Gastroesophageal reflux, allergy and chronic tubotympanal disorders in children. Int J Pediatr Otorhinolaryngol. 2000, 55:187-90.
16. Crapko M, Kerschner JE, Syring M, Johnston N. Role of extra-esophageal reflux in chronic otitis media with Effusion. Laringoscope. 2007, 117:1419-23.
17. Halstead LA. Role of gastroesophageal reflux in pediatric upper airway disorders. Otolaringol Head Neck Surg. 1999, 120:208-14.
18. Megale SRMCL, Scanavini ABA, Andrade EC, Fernandes MIM, Anselmo-Lima WT. Gastroesophageal reflux disease: Its importance in ear, nose, and throat practice. Int J Pediatr Otorhinolaryngol. 2006, 70:81-8.
19. Speri MRB, Pratesi R. Emissões otoacústicas transients e espontâneas em recém nascidos a termo. Artigos distúrbio da comunicação. São Paulo. 2004, 16(1):9-16.
20. Finitzo T, Albright K, Oneal J. The newborn with hearing loss: detection in the nursey. Pediatrics. 1998, 102(6):1452-60.
21. Basseto M, Chiari BM, Azevedo MF. Emissões otoacústicas evocadas transientes (EOAT): amplitude da resposta em recém-nascidos a termo e pré-termo. Rev Bras Otorrinolaringol. 2003, 69(1):84-92.
22. Naeve SL, Margolis RH, Levine SC, Fournier EM. Effects of ear-canal air pressure on evoked otoacoustic emissions. J Acoustic Soc Am. 1992, 91:2091-5.
23. Holte L, Margolis RH, Cavanaugh RM. Developmental changes in multifrequency tympanograms. Audiology. 1991, 30:1- 24.
24. M Vlachou S, Ferekidis E, Douniadakis D, Apostolopoulos N, Adamopoulos G. Multiple-frequency tympanometry in children with acute otitis media. Otolaryngology - Head Neck Surgery. 1999, 121(6):797-801.
25. Koivunem P, Uhari M, Laitakari K, Alho OP, Luotonem J. Otoacustic emissions and tympanometry in children with otitis media. Ear Hear. 2000, 21:212-17.
26. Azevedo MF. Emissões otoacústicas. Figueredo MS. Emissões otoacústicas e BERA. São José dos Campos: Pulso; 2003. p.53-7
1) Attending Master's degree in human communication disorders at the Federal University of São Paulo (UNIFESP). Assistant Professor of the State University of Health Sciences in Alagoas (UNCISAL)'s Phonoaudiology School.
2) Doctor in Human Communication Disorders from the Federal University of São Paulo (UNIFESP). Cooperator Professor of Human Communication Disorders at the Federal University of São Paulo (UNIFESP).
3) Specialized in Audiology from the State University of Health Sciences in Alagoas (UNCISAL). Junior Doctor in audiology at the State University of Health Sciences of Alagoas (UNCISAL).
4) Specialization in Audiology Clinics by the Mother and Child Institute of Pernambuco. Junior Doctor in Audiology from the State University of Health Sciences in Alagoas (UNCISAL).
5) Otorhinolaryngologist. Labor and Traffic Doctor.
6) Doctor in Human Communication Disorders from the Federal University of São Paulo (UNIFESP). Associate Professor Doctor of the Federal University of São Paulo (UNIFESP).
Institution: State University of Health Sciences of Alagoas (UNCISAL). Arapiraca / AL - Brazil. Mailing address: Kelvânio Vitório de Farias - Travessa Manoel Afonso Maranhão, 83 - Jardim Esperança - Arapiraca / Al - Brazil - ZIP Code: 57307-300 - Telephone: (+55 82) 9932-0729 - Email: k_fono@hotmail.com
Article received on January 19, 2011. Article approved on April 19, 2011.