INTRODUCTION Despite of the tongue being in frequent contact with trauma, bites and foreign bodies, it is rare the occurrence of abscesses in the tongue (1). That arises due to the fact that it presents keratinized squamous epithelium; the muscles are very vascularized, rich lymphatic drainage and direct contact with the saliva that has immune functions of protection, lubrification and constant cleaning (2). BERNARDINI reported in a review of literature performed between 1816 e 1945 a total of 186 cases (3). SANDS found 28 cases reported in the English language from 1957 and 1993, and only 12 of them were out of India (4). Were found 33 cases reports from 1993 to 2008 in English language (1,2,4-13). Epidemiologically is more associated to the male gender, to smoking, to the use of dental prostheses and poor oral hygiene (4). The etiology must be considered depending on the local of the clinical manifestation. Abscess from the anterior two thirds of the tongue are results from bites, local traumas and foreign bodies. The posterior third can be related with lingual tonsils, to thyroglossal duct remnants and the pathologies from the first and second molars (4,10). Fracture of the jaw, insect bites and mucosal resection of the mucosa of the nasal septum must be researched (1). The recently literature shows association between piercings and tongue abscesses (9). This work has as objective report a case of tongue abscess occurred in our service, and do a literature review.
CASE REPORTPatient EF 76 years old was attended with complaints of pain when swallowing of progressive evolution for about a week, with increased deterioration 3 days ago, associated to the reduction of the food intake because of the pain. Report the history of surgery for dental implant in the beginning of the period. Present history of myocardial revascularization 19 years ago making a regular use of antiplatelet, associated to systemic arterial hypertension and chronic renal failure clinically controlled. Denied smoking and drinking. In the moment of admission the patient was prostate, dehydrated ++/4+, eupneic and no fever. The exam in the oral cavity showed bulging of approximately 2x2 cm in the posterior middle third of the tongue to the right side, painful to the touch, without limits in the mouth opening. Were not evident vegetating lesions or ulceratd. The nasofibroscopy showed moderate bulging in the base of the tongue to the right side, hyperemia of the epiglottis, vocal folds were mobile bilaterally, good air gap, absence of laryngeal lesions. Hemogram with 18.400 leukocytes at the expense of targeted (71%). Was chosen the patient hospitalization. Was asked a magnetic resonance imaging (MRI) that showed lesion of irregular configuration, multiloculated, measuring 4x3 cm in its biggest diameter at the base of the tongue to the right side, characterized for hyper intensity of signal in the weighted sequences in T2 and hypo intensity of signal in the weighted sequences in T1. The lesion presented peripheral enhancement after the injection of the paramagnetic contrast agent and was associated to the deviation to the left of the septum interlingual. On the clinical history, of the clinical picture and the MRI, initiated the clinical support to the patient and intravenous antibiotic therapy with clindamycin and ceftrioxona. The surgical exploration of the lesion was performed in the fifth day of hospitalization because the patient was using the AAS. Was showed the thick secretion in the surgical act, being harvested material for anatomopathological and culture. The patient progressed satisfactorily with improvement of the pain and the general state being discharged on the seventh day of hospitalization. The anatomopathological of the material picked showed a inflammatory chronic process nonspecific amid mild fibrosis and skeletal muscle tissue, no signs of malignancy. The culture of the material was negative.
DISCUSSIONThe clinical manifestation from the tongue abscess can be varied. Pain, fever, bulging, odynophagia, dysphagia and otalgia may be present (8).
The diagnosis must be done by the clinical history, correlating the risks factors associated with smoking, poor oral hygiene, use of dental prostheses and sex, physical exam of the oral cavity and frequently in confirming image exams. The ultrasonography defines and differentiates cystic structures, vascularized and abscesses but in the tongue there is a difficult for the use of the transducer. The computed tomography allows definition and anatomical relation of the lesion mostly in the posterior third of the tongue.
The MRI allows a better visualization of soft tissue and avoids artifacts of the jaw and dental amalgam, being this the chosen exam in the case (6,14). The time of evolution of the presented case, the previous history of the dental implant, clinical manifestation of the patient and findings in the MRI, directs us to the for the suspect of tongue abscess, however is of extremely importance we consider differential diagnosis depending on the location of the lesion (4).
The differential diagnosis from the anterior lesions of the tongue includes lingual artery false aneurysm, tuberculosis, syphilis, neoplasms and actinomycosis (2,7,15). The lesions from the posterior third must include thyroglossal cyst and lingual tonsil abscess (2). Infarctions, edema, macroglossia due to hypopituitarism, metabolical alterations as deficiency of B12 vitamin, hypothyroidism, amyloidosis, acromegaly, iron deficiency, also must be considered as differential diagnosis (8).
The approach must include the permeability of the airway, clinical support, systemic antibiotic therapy and abscess drainage (4,12).
The antibiotic therapy used in our case, clindamycin and ceftriaxone, presented and adequate coverage for the microorganisms more commonly responsible for the abscess of the tongue according to the literature. They compose a mixed flora and are frequently present in the superior airway and in the flora of the oral cavity. The most common are the Streptococus Viridans, Haemophilus influenzae, Staphylococus aureus, Bacterioides e Neisseria, and others (1,2,4,5,6)
The option for the surgical drainage, that should have been immediate, was performed after the fifth day of hospitalization because the patient was in use of antiplatelet agent and had satisfactorily answered in the beginning of the clinical treatment, which allowed us to avoid the risk of bleeding. Could have chosen for the drainage for guided puncture by ultrasonography, being this a less invasive procedure, with lower risks of bleedings also effective in the drainage of the abscess (1), but we did not have technical conditions for its realization.
The abscess when located in the posterior third of the tongue, requires a surgical drainage under general anesthesia, because can evolve with the local edema and obstruction of the airway, increasing even more the risk of the procedure (1).
The good prognosis and the none recurrence of the abscess in cases where are performed abscess drainage (surgical or by puncture) is due to the factors of protection presented by the tongue like the bactericidal action of saliva, its rich vascularization and the musculature that when contracting limits the inflammation and the cavity formed by the abscess (1). However the gravity of the abscess, there are no reports in the literature of fatal cases after the extensive use of antibiotics (4).
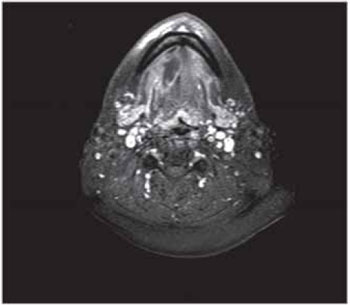
Figure 1. Axial contrast-enhanced T1 SPIR.
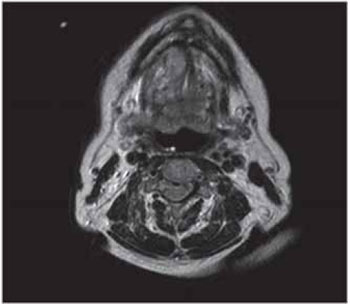
Figure 2. Axial T2 Court.
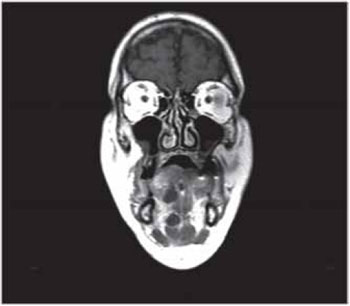
Figure 3. Court Coronal T1 with contrast.
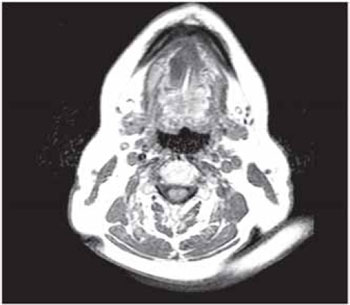
Figure 4. Cut Axial T1 without contrast.
The tongue abscess is a rare disease, however must be considered as a differential diagnosis from the bulging of the tongue. The image exams help in the diagnosis. The systemic antibiotic therapy associated to the drainage is the treatment of choice for the tongue abscesses and must be performed in a routine basis.
BIBLIOGRAPHIC REFERENCES1. Balatsouras DG, Elioupolous NP, Kaberos AC. Lingual Abscess: Diagnousis and Treatment. Head Neck. 2004, 26(6):550-554.
2. Hehar SS, Johnson IJM, Jones NS. Glossal abscess presenting as unilateral tongue swelling. The Journal of Laryngology and Otology. 1996, 110:389-390.
3. Bernardini CV. Abscess of the tongue. California and Western Medicine. 1945, 63:1316-1317.
4. Sands M, Pepe J, Brown RB. Tongue abscess: case report and review. Clin Infect Dis. 1993, 16:133-35.
5. Munõz A, Ballesteros AI, Castelo JAB. Primary Lingual Abscess Presenting as Acute Swelling of the Tongue Obstructing the Upper Airway: Diagnosis with MR. Am J Neuroradiol. 1998, 19:496-498.
6. Ozturk M, Mavili E, Erdogan N, Cagli S, Guney E. Tongue Abscesses: MR Imaging Findings. Am J Neuroradiol. 2006, 27:1300-03.
7. Kim HJ, Lee BJ, Kim SJ, Shim WY, Baik SK, Sunwoo M. Tongue Abscess Mimicking Neoplasia. Am J Neuroradiol. 2006, 27:2202-03.
8. Antoniades K, Hadjipetrou L, Antoniades V. Acute tongue abscess: report of three cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004, 97:570-73.
9. Olsen JC. Lingual abscess secondary to body piercing. J Emerg Med. 2001;20:409.
10. Eviatar E, Pitaro K, Segal S, Kessler A. Lingual abscess: Secondary to follicular tonsillitis. Otolaryngology - Head and Neck Surgery. 2004, 131(4) 558-559.
11. Boon M, Pribitkin E, Spiegel J, Nazarian L, Herbison GJ. Lingual abscess from a grill cleaning brush bristle. Laryngoscope. 2009, 119(1):79-8.
12. Vellin JF, Crestani S, Saroul N, Bivahagumye L, Gabrillargues J, Gilain L. Acute Abscess of the Base of the Tongue: A Rare but Important Emergency. J Emerg Med. 2008 Nov 18.
13. Moya Albiol S, Estors JL, De la Fuente Arjona, Urchueguía Navarro MT. Tongue abscess. Report of a case and bibliographic review. Acta Otorrinolaringol Esp. 2000, 51(6):535-8.
14. Ozturk M, Yorulmaz I, Guney E, Ozcan N. Masses of the tongue on mouth floor: findings on magnatic resonance imaging. Eur Radiol. 2000, 10:1669-1674.
15. Zamarro MTL, Pérez ML, Soriano JAM, Sanz GM. Actinomicosis de base de lengua. Acta Otorrinolaringol Esp. 2005, 56:222-225.
1) Medical Resident in Otorhinolaryngology.
2) Doctorate from the Faculty of Medicine of from USP Ribeirão Preto. Professor from the Departament of Otorhinolaryngology and Surgery from Head and Neck from Medical School of São José do Rio Preto -FAMERP.
3) Radiologist. Assistant Professor of Education from the Departament of Image from the Hospital de Base de São José do Rio Preto.
Institution: Departament of Otorhinolaryngology and Surgery from Head and Neck from Medical School of São José do Rio Preto -FAMERP. São José do Rio Preto / SP - Brazil. Mailling Adress: Thiago Bittencourt Ottoni de Carvalho - Rua José Picerni 449, Apto 21 - Jardim Panorama - São José do Rio Preto / SP - Brazil - Zip Code: 15091-200 - Tel.: (+55 61) 7814-7648; (+55 17) 8141-5584 - E-mail: drthiago.ottoni@yahoo.com.br
Article received in November 29 of 2009. Article approved in January 27 of 2010.