 |
556 |
|
| Year: 2008 Vol. 12 Num. 3 - Jul/Set - (21º)
|
|
 |
|
|
| Pleomorphic Adenoma of Maxillary Sinus - A Case Report |
|
| Author(s): |
| Camila Cristina Ishikawa1, Fabrizio Ricci Romano2, Richard L. Voegels3, Ossamu Butugan3
|
|
|
| Key words: |
| pleomorphic adenoma, maxillary sinus, salivary glands |
|
|
 |
| Abstract: |
Introduction: Pleomorphic adenoma is the most common head and neck benign glandular tumor. Pleomorphic adenoma of the maxillary sinus has rarely been described in the literature. Objective: To report a case of a patient with a unilateral nasal mass, originated from the maxillary sinus, with histopathological diagnosis of pleomorphic adenoma. Case Report: A.O.V., 55-year-old male Caucasian patient, who had been suffering from nasal obstruction for years and also presented a polypoid mass in the left nasal cavity. Patient was submitted to endoscopic tumor resection and diagnosed of pleomorphic adenoma. Conclusion: Although pleomorphic adenoma is a rare type of tumor, it is benign, and it must be distinguished from other nasal tumors associated with chronic nasal complaints.
|
|
 |
INTRODUCTION
The pleomorphic adenoma is the most common benign glandular tumor originated in the head and neck (1,2). It is the tumor that most commonly affects the major salivary glands, specially the parotid glands in 80% of the cases. The minor salivary glands are only affected in 8% of the cases, generally in soft and hard palates (3). It seldom affects other areas of the aerodigestive tract.
In the nasal cavity, its most frequent location is the quadrangular cartilage, followed by the nasal lateral wall, mainly the infundibula (1). Maxillary sinus pleomorphic adenoma cases are rarely described in the literature (4).
The purpose of this work is to report the case of a patient with a unilateral nasal mass, originated in the maxillary sinus, who had the histopathological diagnosis of pleomorphic adenoma.
CASE REPORT
A.O.V., 55 years old, white, male, went to the Otorhinolaryngology service complaining of nasal obstruction of many years, pruritus and eventual sneezes. He denied pain, facial convexity or blooding events. At the otorhinolaryngological examination a moderate increase of the inferior nasal turbinates was observed, with the presence of thick mucoid secretion in the left nasal cavity. In the nasofibrolaryngoscopy the presence of a polypoid aspect mass was observed, originated in the left medium meatus and protracting to the nasal cavity.
The computed tomography (Figures 1 and 2) of paranasal sinus revealed a mass of lobate contours, occupying the left maxillary sinus drainage ostium, expanding to the left maxillary sinus, inferior medium ipsilateral meatus and pharyngonasal cavity, compressing and diverting the osseous nasal septum to the right. There were no signs of osseous invasion. There was no significant enhancement evidenced by the contrast injection.
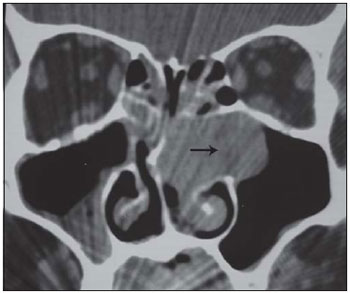 Figure 1. Computed tomography of paranasal sinuses in coronal cut, showing mass occupying the left maxillary sinus, expanding to the maxillary sinus and nasal cavity (arrow). 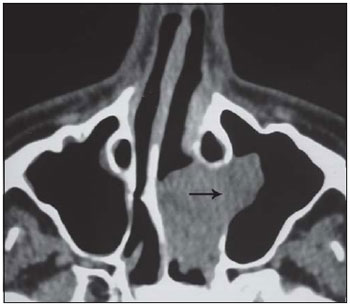 Figure 2. Computed tomography of paranasal sinuses in axial cut, showing mass occupying the left maxillary sinus ostium, expanding to the maxillary sinus and nasal cavity (arrow).
He was submitted to a full tumor resection via endoscopy, and a left maxillary sinus superior wall tumor insertion was observed. The histopathological exam presented the diagnosis of pleomorphic adenoma.
In the postoperative, the patient keeps on ambulatory service follow-up, without evidence of a clinical and tomography recurrence 4 years after the surgery (figures 3 and 4).
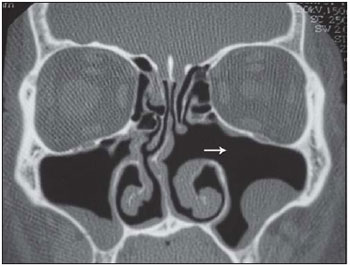 Figure 3. Computed tomography of paranasal sinuses in coronal cut, postoperative control, showing recurrence signals absence (arrow). 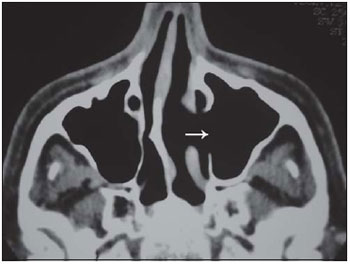 Figure 4. Computed tomography of paranasal sinuses in axial cut, postoperative control, showing recurrence signals absence (arrow).
DISCUSSION
The pleomorphic adenoma rarely affects the nasosinusal cavity. A number of nasal pleomorphic adenoma cases, described by Compagno and Wong (5), included 40 cases from more than 10.000 tumors of salivary glands, but no primary involvement of paranasal sinuses has been found. In a review of 2807 cases of salivary glands cancer, Spiro (6)did not describe any benign tumor of maxillary and ethmoidal sinuses.
The pleomorphic adenoma may be present at any age, but the majority occurs between the 3rd and 6th decades of life, and is more common in women, without racial distinction (2,4).
The main complaints are: unilateral nasal obstruction (71%) and epistaxis (56%). Other symptoms are nasal mass, epiphora and rhinorrhea (7). It appears as a painless, unilateral, grayish-white, submucosal, polypoid, firm and encapsulated mass (2).
The radiologic findings are not specific. TC shows a homogeneous, well delimited mass, without calcifications, with osseous remodeling, suggesting a slow growth benign process (7,8). The RNM image is variable; it generally shows a well delimited mass, with hyposignal in T1 and intermediate and heterogeneous signal in T2 (8).
The diagnosis is carried out by the suspected lesion biopsy. It histologically presents high myoepithelial cellularity with little or no stromal component (7). The nasal cavity pleomorphic adenoma generally shows a more cellular pattern with less stroma, in contrast with the histological findings of the major salivary glands tumors (4).
The differential diagnosis includes polyp, papilloma, angiofibroma, haemangioma and CEC (7).
The chosen treatment is the surgery excision with free margins (3,7). The access depends on the size of the tumor. When the tumor is small, it is recommended to use the approach via transnasal endoscopy; if there is large tumor commitment the lateral rhinotomy or mid-facial degloving is recommended complimented with nasal endoscopy (3). In more recent publications, some authors showed that the intranasal access through endoscopy is effective with low recurrence range (7). Radiotherapy has little usability in these patients and is only indicated in case of unresectable tumors or of surgery contraindication (3).
The routine postoperative follow-up is necessary due to the recurrence potential (2.4 to 7.5% of cases after primary excision) (7) and malignant transformation (2 to 3%) that occur mainly in the cases of tumor recurrence (3).
The presence of a tumor in this patient, with less exuberant and of long duration symptomatology, reinforces the orientation that every patient with chronic nasal complaint must be submitted to investigation via endoscopy or tomography, with the risk of failing to diagnose important and potentially severe affections.
FINAL COMMENTS
The unilateral nasosinusal mass differential diagnosis is not always easy, since the patients very often present slow evolution non-specific symptoms, and implies several benign and malign tumors. The definite diagnosis is made by means of histopathological exam.
BIBLIOGRAPHICAL REFERENCES
1. Felix JAP, Tonon S, Saddy JC et al. Adenoma pleomórfico de septo nasal: relato de caso e revisão da literatura. Rev Bras Otorrinolaringol. 2000, 66:409-412.
2. Rocha MP, Campagnolo AM, Macedo VS et al. Adenoma pleomórfico de septo: relato de caso. Rev Bras Otorrinolaringol. 2004, 70:416-418.
3. Patrocínio TG, Patrocínio JÁ, Patrocínio LG. Adenoma pleomórfico nasal: ressecção via degloving médio-facial. Arq Int Otorrinolaringol. 2006, 10:154-158.
4. Berenholz L, Kessler A, Segal S. Massive pleomorphic adenoma of the maxillary sinus. Int J Oral Maxillofac Surg. 1998, 27:372-373.
5. Compagno J, Wong RT. Intranasal mixed tumors (pleomorphic adenomas). A clinicopathologic study of 40 cases. Am J Clin Pathol. 1977, 68:213-218.
6. Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2807 patients. Head Neck Surg. 1986, 8:177-184.
7. Jackson LE, Rosenberg SI. Pleomorphic adenoma of the lateral nasal wall. Otolaryngol Head Neck Surg. 2002, 127:474-476.
8. Fushiki H, Morijiri M, Maruyama M et al. MRI of intranasal pleomorphic adenoma. Acta Otolaryngol. 2006, 126:889-891.
1. Medical Doctor. HCFMUSP Otorhinolaryngology Discipline Resident.
2. Doctor of Science by FMUSP. Assistant Doctor at HCFMUSP Otorhinolaryngology Clinical Division.
3. Ph.D., Professor of HCFMUSP Otorhinolaryngology Discipline.Professor Associated of the HCFMUSP Otorhinolaryngology Clinical Division.
Institution: Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo. São Paulo / SP - Brazil.
Mail adrress:
Camila Cristina Ishikawa
Rua França Pinto, 512 - Apto. 161
São Paulo / SP - Brazil - Zipcode: 04016-002
Fax: (+55 11) 5539-1957
E-mail: camilaishikawa@yahoo.com.br
Article received on September 8, 2007.
Article approved on March 30, 2008
|
|
 |
|
|
