 |
765 |
|
Year: 2011 Vol. 15 Num. 2 - Abr/Jun - (13º)
DOI: 10.1590/S1809-48722011000200013
|
|
 |
| Section:
Original Article
|
|
|
|
|
| Audiologic Evaluation of Patients with Mucopolysaccharidosis at a Pediatric Hospital |
|
| Author(s): |
| Ariana Braga Gomes1, Rodrigo Guimarães Pereira2, Tríssia Maria Farah Vassoler3, Lauro João Lobo Alcantara4, Elise Zimmermann3, Mara Lúcia Schmitz Ferreira Santos5.
|
|
|
| Key words: |
| otorhinolaryngology, pediatrics, mucopolysaccharidosis, audiology. |
|
|
 |
| Abstract: |
Introduction: Mucopolysaccharidosis are characterized by the deficit of lysosomal enzymes corrupting the glycosaminoglycans. Accumulating these metabolites causes several alterations, such as otologic alterations. Objective: To evaluate a number of patients with mucopolysaccharidosis at Pequeno Principe Hospital, emphasizing their audiologic alterations and establish a permanent evaluation protocol for these patients. Method: A backward-looking study of audiologic evaluation by using records of 18 patients diagnosed with mucopolysaccharidosis and attended at Pequeno Principe Hospital between January 2005 and November 2010. Results: 7 records were selected, out of which only one did not have a hearing loss, and most of them presented conductive or mixed hearing loss, and only one had an exclusively sensorineural loss. Six of these patients had also been submitted to at least one otorhinolaryngological procedure. Conclusion: Mucopolysaccharidosis patients require a permanent care and a multidisciplinary follow-up. The pediatric otorhinolaryngologist plays an important role when performing the otologic and audiologic evaluation and managing the airways, since almost all the patients evaluated presented some kind of hearing loss and an indication of otorhinolaryngologic procedure. The pattern determined in our service was at least an initial consultation when there is a suspicion and/or diagnosis of MPS and sequential consultations that were at least twice a year or more frequent, if necessary.
|
|
 |
INTRODUCTION
Mucopolysaccharidoses (MPS) represent a group of diseases characterized by the deficit of lysosomal enzymes lowering the glycosaminoglycans (GAGS), which are carbohydrate polymers and proteins. They are a part of a group of hereditary metabolic diseases known as inborn errors of metabolism. MPS are rare diseases separately, but jointly they have an estimated incidence of 1:10000 to 1:25000 (1).
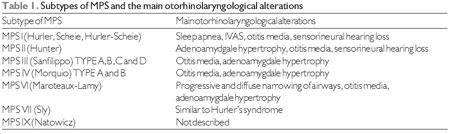
There are seven known types of mucopolysaccharidosis based on both clinical characteristics and the deficient enzyme (Table 1). All of them present an autosomal recessive inheritance, except for the type II (Hunter's syndrome) presenting an X- associated inheritance. Accumulating these metabolites causes several alterations, and these children are generally born without these alterations and develop them progressively (2).
The diagnosis is made by the GAG standard in urine and confirmed by the analysis of lysosomal enzymes in blood, leukocytes or, in addition to a genetic study. In suspected cases, amniocentesis and biopsy of chorionic vilosities allow for the prenatal diagnosis (3).
Clinical presentation can be wide-ranging, and the most common manifestations are: skeletal and cardiac alterations, mental retardation, organomegaly and characteristic facies (3).
The otorhinolaryngologic alterations of these patients can be divided into three groups: otologic alterations, adenotonsillar hypertrophy and airway alterations.
Adenotonsillar hypertrophy is sensibly universal by reason of the deposit of glycosaminoglycans, therefore, an indication of adenoamygdalectomy is frequently noticed on these patients. This type of deposit can as well be seen on the pharynx walls and, when in association with macroglossia and mandible abnormalities (occasionally they are seen on MPS cases), there is the risk of progressive obstruction of upper airways and sleep apnea. Additionally, infections recurring from the upper respiratory tract can also cause tonsillar diseases associated with this disease. With respect to managing the obstruction of the upper airways, firstly adenoamygdalectomy is performed and, in most of the cases, it is the only necessary treatment. Occasionally, in extreme cases, there is a need for tracheotomy (2).
In association with adenotonsillar hypertrophy, there can still be a deposit of glycosaminoglycans on both pharynx and larynx walls, especially in arytenoid cartilages and aryepiglottic membranes. In extreme cases, due to the accumulation of mucopolysaccharides, there is a prolapse of laryngeal wall, provoking stridor and a severe obstruction of the airways. Besides, there is a possibility of deposit on tracheal walls with a subsequent narrowing of lumen (2).
In the present study, we shall emphasize the otologic alterations. The most common alterations are: otitis media with effusion (OME), which can lead to both conductive hearing and sensorineural alterations (4).
The objective of this study is o evaluate a number of patients with mucopolysaccharidosis at Pequeno Principe Hospital, emphasizing their audiologic alterations and establish a permanent evaluation protocol for these patients.
METHOD
The present work is characterized as a backward-looking study of audiologic evaluation by using records of 18 patients diagnosed with mucopolysaccharidosis and attended at Pequeno Principe Hospital between January 2005 and November 2010.
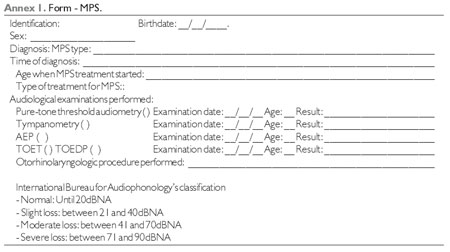
The evaluation of the hearing loss was performed by analyzing the data achieved by a pure-tone threshold audiometry, impedance audiometry, AEP (Brainstem Auditory Evoked Potential) and TOE (transient otoacoustic emissions), and the degree of hearing loss is analyzed in accordance with the International Bureau for Audiophonology's classification (5).
The collection of information was performed by filling out a form based on each patient's records (Annex 1).
The research project was evaluated and approved by the Ethical and Research Committee of Human Beings of Pequeno Principe Hospital (registration Nº 0822-10).
Patients - inclusion criteria
The criteria to include patients in this study are as follows:
- To present a diagnosis of mucopolysaccharidosis;
- To present an audiologic evaluation and description of an otorhinolaryngologic physical examination in the record;
- Absence of erasures and/or unintelligible writing;
Selecting patients
The selection of patients for this study complied with the following plan:
- To acquire at Pequeno Principe Hospital's SAME a list of the patients served and diagnosed with mucopolysaccharidosis in the period between January 2005 and November 2010;
- Patients' conformity with the inclusion criteria.
Outlining the study
After selecting the records, their data were analyzed by filling out a specific form (Annex 1).
The described audiologic alterations were divided into conductive, sensorineural and mixed. The degree of hearing loss was analyzed in accordance with International Bureau for Audiophonology's classification (5).
The therapeutics established for each specific situation was equally analyzed.
RESULTS
On the whole, the records of 18 patients diagnosed with mucopolysaccharidosis served in the period between January 2005 and November 2010 were evaluated.
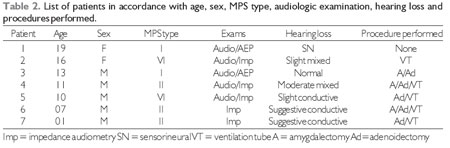
From this total, 7 records were selected in accordance with the inclusion criteria described in the method. Same were numbered from 1 to 7.
The group's average age was 11 years; 5 patients were male and 2 were female (Table 2).
Two patients had a type 1-MPS diagnosis, three patients had the type II and two patients had the type IV (Table 2).
From the seven patients, five performed either audiometry and impedance audiometry examinations or audiometry and AEP, whilst two performed only impedance audiometry (Table 2).
With respect to the type of hearing loss, 42.8% (three patients) had exclusively conductive type, 28.5% (two patients) had the mixed type, 14.3% (one patient) had exclusively sensorineural type, and in 14.3% (one patient) the examination was normal (Table 2).
The group, one patient was submitted to adenoamygdalectomy procedure, one patient was submitted only to ventilation tubes, two patients were submitted to adenoidectomy with ventilation tubes, two patients were submitted to adenoamygdalectomy and ventilation tubes, and one patient was not submitted to any otorhinolaryngological surgical procedure (Table 2).
DISCUSSION
MPS otorhinolaryngologic manifestations can be divided into three groups: otologic problems, adenotonsillar hypertrophy and airways disorders. Minor degrees attacks, such as otitis media with effusion, are nearly universal in this group of patients (2).
Owing to the deposit of mucopolysaccharides on rhinopharynx, hearing tubes and middle ear, these patients presented an elevated risk of developing otitis media with effusion and recurring episodes of acute otitis media. Whenever indicated, symptomatic treatments must be put into practice as a placement of ventilation tubes and hearing apparatus when indicated.
It is unclear whether the sensorineural element has a congenital basis or it is secondarily acquired to the deposit of glycosaminoglycans partially lowered in the cochlear duct, stria vascularis in the cochlear nerve or even in the central nervous system. This type of sensorineural loss is particularly noticed in patients with types I and II-MPS (4.7). Besides, the deposits in the middle ear can explain the inability that some patients have to recover the difference between the airways and the bone conductions in the audiometry after performing tympanotomy (4). Unluckily, the hearing loss is frequently noticed at the moment of diagnosis and, while the conductive hearing loss is unlikely to improve, amplification is usually required in cases of permanent sensorineural loss (4,7).
In a backward-looking study (n=9) with the intention of evaluating the otorhinolaryngologic alterations found in children with a confirmed diagnosis of mucopolysaccharidosis, it has been noticed the 100%-prevalence of recurring otitis media in the evaluated group. Additionally, all the patients in the series were submitted to tympanotomy at least once and 78% of them were submitted to multiple tympanotomy with the placement of ventilation tubes. Hearing loss was demonstrated by audiometry in 78% of patients. Of this group, 71% had mixed hearing loss, 14% had only sensorial hearing loss and 14% had only a conductive one (4).
Further to the management of the symptoms and individual manifestations, efforts have been made to control the pathologic processes as a whole, in an attempt to block or at least adjourn the evolution of the disease. The transplantation of osseous medulla has been investigated since the 1980's and has been frequently used in MPS children under 2 years of age or in those patients with slight forms of MPS II, VI or VII (8). Literary data shows a reduction in hepatosplenomegaly, an improvement in airway obstruction, a reduction in the intracranial hypertension and a reduction of the glycosaminoglycan deposits in the cephalorachidian liquid, liver and skin of children submitted to the transplantation of bone marrow, probably due to restoring the ability of the organism in lowering substrates accumulated on cellular level (9). Besides, comparative studies have suggested that the transplantation would result in improving both the hearing ability and the voice in comparison with groups without a treatment (10). More recently, therapies of enzymatic replacement have been developed and used in the treatment of the different types of mucopolysaccharidosis. Although studies demonstrate the promising effect of replacement, there is no random clinical essay demonstrating their actual efficiency yet (4).
CONCLUSION
Mucopolysaccharidosis patients require a permanent care and a follow-up with multidisciplinary professionals. In this context, the pediatric otorhinolaryngologist plays an important role when performing the otologic and audiologic evaluation and managing the airways, since almost all the patients evaluated presented some kind of hearing loss and an indication of otorhinolaryngologic procedure. The clinical suspicion, the early recognition of lesions, as well as the rehabilitation are essential to achieve better results, minimize the sequels and provide a better quality of life to the patients and their relatives. The pattern determined in our service was at least an initial consultation when there is a suspicion and/or diagnosis of MPS and sequential consultations that were at least twice a year or more frequent, if necessary.
BIBLIOGRAPHICAL REFERENCES
1. Yeung AH, Cowan MJ, Horn B, Rosbe KW. Airway Management in Children With Mucopolysaccharidoses. Arch Otolaryngol Head Neck Surg. 2009, 135(1):73-79.
2. Simmons MA, Bruce IA, Penney S, Wraith E, Rothera MP. Otorhinolaryngological manifestations of the Mucopolysaccharidoses. Int J Pediatr Otorhinolaryngol. 2005, 69:589-595.
3. Pinto LLC. Um estudo sobre a história natural da mucopolissacaridose tipo II (Síndrome de Hunter) em pacientes brasileiros. [dissertação] Porto Alegre (RS). UFRS, 2005.
4. Wold SM, Derkay CS, Darrow DH, Proud V. Role of the pediatric otolaryngologist in diagnosis and management of children with mucopolysaccharidoses. Intl J Pediatr Otorhinolaryngol. 2010, 74:27-31.
5. Meikle PJ, Hopwood JJ, Clague AE, Carey WF. Prevalence of lysosomal storage disorders. J Am Med Assoc. 1999, 281(3):249-254.
6. Shinhar SY, Zablocki H, Madgy DN. Airway management in mucopolysaccharide storage disorders. Arch Otolaryngol Head Neck Surg. 2004, 130:233-237.
7. Friedmann I, Spellacy E, Crow J, Watts RW. Histopathological studies of the temporal bones in Hurler's disease (mucopolysaccharidosis IH). J Laryngol Otol. 1985, 99:29-41.
8. Walker RWM, Colovic V, Robinson DN, Dearlove OR. Postobstructive pulmonary oedema during anaesthesia in children with mucopolysaccharidoses. Paediatr Anaesth. 2002, 12:1-7.
9. Belani KG, Krivit W, Carpenter BL, Braunlin E, Buckley JJ, Liao JC, et al. Children with mucopolysaccharidoses: perioperative care, morbidity, mortality, and new findings. J Pediatr Surg. 1993, 28(3):408-410.
10. Papsin BC, Vellodi A, Bailey CM, Ratcliffe PC, Leighton SE. Otologic and laryngologic manifestations of mucopolysaccharidoses after bone marrow transplantation. Otolaryngol Head Neck Surg. 1998, 118(1):30-36.
1 Otorhinolaryngologist Doctor. Fellow at Pequeno Príncipe Hospital's Pediatric Otorhinolaryngology Department.
2 Pediatric Otorhinolaryngologist. Fellowship Coordinator at Pequeno Príncipe Hospital's Pediatric Otorhinolaryngology Department.
3 Otorhinolaryngologist Doctor. Pediatric Otorhinolaryngologist at Pequeno Príncipe Hospital.
4 Assistant Professor of Otorhinolaryngology of UFPR's Medical School (Head of Pequeno Príncipe Hospital's Pediatric Otorhinolaryngology Department).
5 Neuropediatrician at Pequeno Príncipe Hospital. Coordinator at the Emergency Department of Inborn Error of Metabolism at Pequeno Príncipe Hospital.
Institution: Pequeno Príncipe Hospital. Curitiba / PR - Brazil. Mailing address: Ariana Braga Gomes - Avenida Silva Jardim, 2014 - Apto. 304 - Curitiba / PR - Brazil - ZIP Code: 80250-200 - Telephone: (+55 41) 3342-5581 - Email: arianabgomes@gmail.com
Article received on January 16, 2011. Article approved on March 9, 2011.
|
|
 |
|
|
