 |
802 |
|
Year: 2011 Vol. 15 Num. 4 - Out/Dez - (4º)
DOI: S1809-48722011000400004
|
|
 |
| Section:
Original Article
|
|
|
|
|
| Comparison between turbinoplasty and endoscopic turbinectomy: Efficacy and clinical parameters |
|
| Author(s): |
| Marcos Marques Rodrigues1, Ralph Silveira Dibbern2, Luis Francisco de Oliveira3, Melania Dirce Oliveira Marques4, Marcelo Fernando Bella5, Fausto Antonio de Paula Junior3, Fernando Cesar França Araújo4.
|
|
|
| Key words: |
| airway obstruction, nasal obstruction, rhinitis. |
|
|
 |
| Abstract: |
Introduction: Nasal Obstruction is a common symptom and affects 25% of the population. The inferior turbinate hypertrophy is the main cause of nasal obstruction. In the failure of clinical control, a surgical procedure to reduce the size of the inferior turbinate is indicated. Objective: Compare the improvement of life quality in late postoperative of Turbinectomy and turbinoplasty. Method: Study of a retrospective case series. 24 patients were submitted to a nasal surgery of turbinectomy or turbinoplasty in 2007. The patients were invited to an interview in august of 2008. The patients were evaluated in the following items: Postoperative NOSE scale, morbidity in postoperative, bleeding and quantity of crusts in postoperative. Results: 24 patients attended for the evaluation. The main variable analyzed was the difference between NOSE scales in late pre and post operative. There was no statistically significant by the test in the variables studied. Discussion: In the evaluation of the various types of surgical treatment of the inferior turbinate, literature shows similar results to our study, finding similar results between many surgical techniques in the improvement of the nasal obstruction and in mucociliary activity. Conclusion: There are no evidence in the literature and in our sample of the superiority of a technique of surgical treatment in the inferior turbinate under other treatments.
|
|
 |
INTRODUCTION
Nasal Obstruction (NO) is a commom symptom that reaches 25% of the population. The main etiologies for NO are: septal deviation, hypertrophy of the inferior and middle turbinate, nasal polyposis and hypertrophy of pharyngeal tonsils (1). Among those etiologies the hypertrophy of the inferior turbinates (HCCI) figure as the main cause of the nasal obstruction (2). About 20% of european population has chronic nasal obstruction caused by the HCCI (3). Allergic rhinitis, vasomotor rhinitis and septal deviation (compensatory hypertrophy) figure as the main causes of HCCI (4).
There are several options to clinical treatment of HCCI. Antihistamines, topical nasal corticosteroid and saline solution are the main drugs used. Vasoconstrictors and injection of corticosteroids are used on a smaller scale because of the potential deleterious (4). In failure of the clinical control it is indicated usually a surgical procedure to reduce the size of the inferior turbinate. The main techniques described are: Total or partial turbinectomy, turbinoplasty, submucous resection, laser-assisted turbinoplasty, cryosurgery, treatment with infrared light, argon plasma surgery, topical application of AgNO3, monopolar and bipolar electrocautery and volumetric tissue reduction by radiofrequency (5).
The NO is a symptom that produces significant interference in life quality. The nasal obstruction difficult the sleep quality and physical exercises, causes tiredness and irritability. In children the patency is fundamental to the craniofacial development, mouth breathing children tend to develop the ogival palate, long face and retrognathia perpetuating the nasal obstruction in the future adults (6).
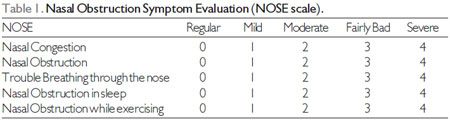
The evaluation of life quality and effectiveness of the treatment of NO is hard. As the American Academy of Otorhinolaryngology validated the questionnaire entitled Nasal Obstruction Syndrome Evaluation, known as NOSE scale, term used in this article. The scale is made up of 5 questions about life quality. Each receive a note that can go from 0 to 4. These notes are summed and multiplied by 20. In this way NOSE scale vary from 0 to 100 (7). The scale translated to Portuguese is found in Table 1.
The NOSE scale became a reference to studies that analyze the influence of NO in life quality, both basal and follow-up after clinical and surgical treatment (8).
The goal of this study is to compare the life quality in the late post operatory of turbinectomy and turbinoplasty.
METHOD
Study approved by the Ethics Committee and Research of Irmandade da Santa Casa de Limeiro under the protocol 145/09 and properly registered at the Clinical Trials Registry. Were evaluated 24 patients submitted to nasal surgery of turbinectomy or turbinoplasty without septoplasty in the period of January to December of 2007. The patients were submitted to nasofibroscopy with Machida Fiberoptic ENT-30 pIII of 3,2 mm were analyzed according to the level of obstruction of upper airway. The patients suffered from hypertrophy of the inferior turbinate. All the patients of the sample suffered from allergic rhinitis and were submitted to oral antihistamines treatment for 30 days and topical nasal corticosteroids for 3 months. The surgery was indicated after the verification of failure of clinical treatment. In this opportunity was applied the NOSE scale, in other words, in pre operatory after the clinical treatment. All the included patients signed the Free and Enlightened Consent Term.
The surgeries were made under general anesthesia and by a single surgeon. In each patient only one technique (Endoscopic Turbinectomy or Turbinoplasty) were bilaterally applied. There are no patients in the sample operated simultaneously by the two techniques. There were no pathological distinctions between the patients submitted to both techniques.
The patients called by the phone to a interview in August of 2008, with average time of 13,2 months of post operatory. The interviewers were the doctors that did not participate of the surgeries and were 'blinded' to the type of used technique. In some items was used the Visual Analogue Scale (VAS) graduating the symptoms from 0 to 10 according to the intensity of the symptoms. The patients were evaluated for the following items: NOSE scale post operatory (PO), associated surgery, and morbidity in PO (VAS), use of a cap, bleedings, amount of crusts in PO (VAS), need of reoperation and use of medications in late PO.
Then, the patients were submitted to a nasofibroscopy with Machida Fiberoptic ENT-30 PIII of 3,2 mm were analyzed according to the anatomical results of the late PO. Exam made with topical anesthetic and without topical vasoconstrictor.
Surgical Technique
Turbinectomy - The endoscopic evaluation of the inferior nasal turbinate. Preparation of the turbinate with topical vasoconstrictor solution with oxymetazoline hydrochloride at 0,05%. The portion of the turbinate to be retreat is designed and clamped with Rochester forceps. After about 3 minutes the drawn part was resected. The residual bloody surface was treated with oxymetazoline hydrochloride at 0,05% and cauterized with monopolar cautery to control the hemostasis.
Turbinoplasty - The endoscopic evaluation of the inferior nasal turbinate. Preparation of the turbinate with topical vasoconstrictor solution with oxymetazoline hydrochloride at 0,05%. Incision with scalpel blade nº 15. Dissection of submucosal tunnel (between the medial mucous and the bone of the inferior turbinate). Resection of a part of the turbinate bone and side mucosa. Next, the lateral flap was repositioned covering the bloody surface. The review of hemostasis was made with oxymetazoline hydrochloride at 0,05% and cauterized with monopolar cautery when necessary.
Exclusion Criteria
1) Younger than 21 years;
2) Craniofacial alterations and/or congenital malformation;
3) Patients with morbid obesity;
4) Patients carrying septal deviation with need of surgical correction;
5) Patients carriers of nasal polyposis and/or nasal tumors of any kind;
6) Patients carriers of chronic rhinosinusitis of any kind;
7) Patients that do not agree in participate of this research and/or refused to sign the Consent Term Free and Enlightened.
Statistical Analysis
The statistical analysis was performed with a statistical software SPSS for Windows and Student T test. The value of p<0,05 was considered statistically significant.
RESULTS
All the patients were contacted by telephone and called to a interview and otorhinolaryngological evaluation. Attended to evaluation 24 patients. The average time of surgery was 13,2 months, ranging from 8 to 20 months. These patients were split in 2 groups:
Group I - Patients submitted to inferior turbinectomy with 15 patients (62,5%);
Group II - Patients submitted to inferior turbinoplasty with 9 patients (37,5%).
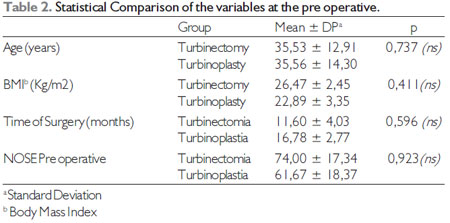
The two groups were compared according to the collected variables in pre operatory, to avoid biases of confusion. The group analysis is found in Table 2. The sample is valid, because the two groups are similar in the pre operatory.
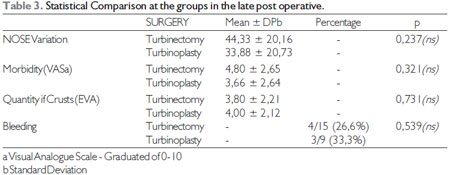
The two groups are compared according to the collected variables in interviews performed in the late post operatory. The main variable analyzed was the difference between NOSE scale in pre and late post operatory. There was no statistically significance by the student t test. The data is exposed in the Table 3.
DISCUSSION
Among the analyzed factors in choosing determined surgical technique, the mos important is without a doubt the security and experience of the surgeon. Other factors to be analyzed are: practicability, replicability, degree of morbidity and mortality and the results of the clinical studies well controlled and conducted. Many techniques are described in literature. The endoscopic approach is safer, because allow to a better evaluation of all the extension of the nasal turbinate, precise manipulation and more efficient hemostasis. The surgeries with use of lasers and radiofrequency have lower morbidity because of the degree of tissue injuries, however, they are expensive techniques and shortly available.
Turbinectomies and turbinoplasties are the most used endoscopic techniques to treat the inferior turbinate in Brazil. Turbinectomies are technically simpler, but, leaves the area bloody and exposed and have two main consequences: the formation of a crust and the need of a wider review of hemostasis. Theoretically this technique presents a bigger amount of crusts and a higher chance of bleeding. A important advantage is that the turbinectomy is of more rapid execution allowing a smaller surgical time and decreasing, consequently, the anesthetic morbidity.
The turbinoplasty is a technique more laborious and considered by a few more elegant, have the obvious advantage of not exposing the bloody area. There is less bleedings and lower formation of crusts. According to the surgeon training, it can be performed in a satisfactory time without increasing for too long the surgical time.
The groups showed itself as homogenous in the pre operative. There was no difference statistically significant as to IMC, NOSE, age and time of surgery. Through this selection we searched to eliminate some of biases of confusion. As the patients had similar points in NOSE scale we can conclude that the morbidity in pre operatory of nasal obstruction in the groups were equivalent.
At the evaluation of the late post operative was verified that the two techniques were equally effective in the improvement of the complaint of nasal obstruction. Both had important reduction at NOSE scale, however without the superiority of a technique over another technique (p=0,237). The two techniques studied were compared to the amount of crusts and morbidity, both from analog visual scale. In this regard the two techniques proved to be similar without a statistically significant difference.
In relation to the incidence of bleeding in post operatory the greater theoretical risk of turbinectomy wasn't confirmed in the sample. The incidence of bleeding was close in post operative of both techniques (p=0,539).
At the evaluation of many kind of surgical treatments of the inferior turbinate the literature show similar results to the study. SPACI and collaborators made a study comparing turbinectomies by laser, radiofrequency and conventional, finding similar results with the improvement of the nasal obstruction and the mucociliary activity (9). CAVALIERE compared the traditional turbinectomy and the radiofrequency finding similar results in the objective and subjective improvement of the nasal obstruction (10).
BHANDARKAR In its review about the procedures of the inferior turbinate, shows that the results of the surgery of the inferior turbinate are favorable and continue to be recommended as a treatment of the hypertrophy of the turbinate responsive not only by clinical treatment. The levels of evidence in literature are improving. Future studies well designed involving prospective data collection, the, measures resulting from the validation, statistical analysis of comparison, or control groups and long term monitoring would be fundamental to the level of evidence (11).
CONCLUSION
There are no evidence in the literature and in our sample of the superiority of turbinectomy over turbinoplasty and vice versa as the efficacy of the surgical treatment of the inferior turbinate on others treatments. The choosing of the surgical technique must be evaluated individually in each individual. All forms evaluated in this study to the surgical treatment of the inferior turbinate are effective. The surgeon must consider many factors like personal experience, applicability, replicability and results of the scientific studies for choosing the most appropriate surgical technique.
BIBLIOGRAPHIC REFERENCES
1. Passali D, Passali FM, Damiani V, Passali GC, Bellussi L. Treatment of inferior turbinate hypertrophy: a randomized clinical trial. Ann Otol Rhinol Laryngol. 2003, 112:683-688.
2. Lai VWS, Corey JP. The objective assessment of nasal patency. Ear Nose Throat J. 1993, 72:395-400.
3. Seeger J, Zenev E, Gundlach P, et al. Bipolar radiofrequency-induced thermotherapy of turbinate hypertrophy: pilot study and 20 months follow-up. Laryngoscope. 2001, 113:130-5.
4. Jackson LE, Koch RJ. Controversies in the management of inferior turbinate hypertrophy: a comprehensive review. Plast Reconstr Surg. 1999, 103:300-312.
5. Hol MKS, Huizing EH. Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniques. Rhinology. 2000, 38:157-66.
6. Camelo-Nunes IC, Solé D. Allergic rhinitis: indicators of quality of life. J Bras Pneumol. 2010, 36(1):124-33.
7. Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 2004, 130(2):157-63.
8. Stewart MG, Smith TL, Weaver EM, Witsell DL, Yueh B, Hannley MT, Johnson JT. Outcomes after nasal septoplasty: results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 2004, 130(3):283-90.
9. Sapçi T, Sahin B, Karavus A, Akbulut UG. Comparison of the effects of radiofrequency tissue ablation, CO2 laser ablation, and partial turbinectomy applications on nasal mucociliary functions. Laryngoscope. 2003, 113(3):514-9.
10. Cavaliere M, Mottola G, Iemma M. Comparison of the effectiveness and safety of radiofrequency turbinoplasty and traditional surgical technique in treatment of inferior turbinate hypertrophy. Otolaryngol Head Neck Surg. 2005, 133(6):972-8.
11. Bhandarkar ND, Smith TL. Outcomes of surgery for inferior turbinate hypertrophy. Curr Opin Otolaryngol Head Neck Surg. 2010, 18(1):49-53.
1) Professor.
2) Master in Otorhinolaryngology by the Medical School of USP Ribeirão Preto. Medic Otorhinolaryngologist responsible by the Sleep Apnea sector of Otorhinolaryngology Departament of Santa Casa de Limeira.
3) Medic. Otorhinolaryngologist of Santa Casa de Limeira.
4) Medic. Redident of Otorhinolaryngology Departament of Santa Casa de Limeira.
5) Coordenator of Otorhinolaryngology Departament of Santa Casa de Limeira.
Institution: Brotherhood of Santa Casa de Misericórdia de Limeira. Limeira / SP - Brazil. Mailling address: Marcos Marques Rodrigues - Avenue Geraldo Hilário da Silva, 146 - Jardim Flamboyant II - Araraquara / SP - Brazil - ZIP code: 14805-290 - Telephone: (+55 16) 8108-4840 - E-mail: marcosmmr@hotmail.com
Article received in March 10th of 2011. Article approved in July 10th of 2011.
|
|
 |
|
|
