INTRODUCTIONThe otitis media with effusion (OME) is one of the most common diseases of the childhood that demand visits at the otorhinolaryngologist. It is characterized by the presence of a liquid in the middle ear that may present as from clean and fluid up to thick and brownish, with a high protein content, original in the secretory epithelium.
The major incidence occurs in children aged from 6 to 13 months, with a second peak of incidence at the age of five years and strong association of immunological and social factors (1). The physiopathologic basis is intimate connected to the disorder of the Eustachian tube, anatomic disturbances or inflammatory and histological changes (2, 3).
The clinical manifestations are variable and may damage the speech development and the general learning. As the parents' report is not a reliable preview of audiologic changes (4), the diagnosis must be searched mainly upon physical exam and tympanometry.
The treatment of otitis media with effusion may be clinical or surgical. The standard surgical treatment is tympanostomy and positioning of the ventilation tube that allows the removal of liquid from the middle ear during the surgery by aspiration and at the follow-up, as well as allows the entry of air in the middle ear, by restoring the child's hearing and reversing the middle ear epithelium changes (5).
The surgical success is defined by the reversion of histological alterations and consequently the improvement of the child's hearing, that prevents learning deficits, speech disorders and psychosocial adjustment.
The objective of this study was to evaluate the follow-up of the children with diagnosis of otitis media with effusion submitted to surgical treatment, with focus on the preoperative and postoperative audiometric findings.
METHODThe retrospective study had its research protocol evaluated and approved by the Ethics Committee in Research of the Hospital under the number 009/2008. In the study we included patients aged less than twelve years old with diagnosis of otitis media with effusion resistant to clinical treatment and that were submitted to tympanostomy and insertion of the ventilation tube at the Hospital's Otorhinolaryngology Clinic in 2007. We excluded patients who did not present complete records.
We reviewed the records and analyzed the audiometry results of the children of the preoperative and postoperative. After the diagnosis, made by the clinical history, physical exam and audiometry, all patients were submitted to a set of clinical treatments that included oral antibiotics (amoxicillin 50mg/kg/dose during ten days), topical corticosteroids (for four weeks) and oral corticosteroids (1mg/kg/day for one week). After this period the clinical evaluation was repeated and a new tonal and vocal audiometry was carried out associated to imitanciometry to certify the failure of the clinical treatment. This second audiometry was used as a preoperative reference.
The postoperative audiometry was requested in the middle-term follow-up with an interval from six months to one year as of the operation after extrusion of the tube. We evaluated auditory the thresholds in the usual frequencies by airway and osseous way, and identified air-osseous gaps typical of conductive loss. The Speech Recognition Threshold (SRT) was also used in the evaluation.
The results express the comparison of the audiometric parameters before and after the surgical treatment. The four tone thresholds average for the speech area (LT) consists of the arithmetic average of the auditory thresholds for pure tones in the frequencies of 500, 1000, 2000 and 3000Hz.
RESULTSInitially we identified twenty children with diagnosis of chronic otitis media with effusion, resistant to clinical treatment, in 2007. Two of whom were not submitted to ventilation tube insertion because during the surgical procedure the state of the tympanic membrane and the middle ear did not justify such measure. These children were excluded from the study. Out of the eighteen children who were submitted to tympanostomy and positioning of the ventilation tube, sixteen maintained the middle term follow-up and carried out preoperative and postoperative audiometry, amounting to 32 (thirty-two) ears operated.
There were no complications as for the surgical procedure concerning tympanostomy and the insertion of the ventilation tube. The tympanostomy incision was radial, preferably in the antero-inferior quadrant, except for when an anterior convexity of the auditory meatus did not allow the complete viewing of the region. In this case, the incision was made at the lower region of the tympanic membrane, by preventing the tympanic ring, hammer and postero-superior region from the presence of the ossicular chain in this region. All sixteen children were submitted to adenoidectomy upon operatory procedure, for they presented hypertrophy. Ten patients were submitted to simultaneous tonsillectomy for sleep disorders justified by the palatine tonsils hypertrophy or recurrent tonsillitis. There was no difference between postoperative auditory thresholds of this group of ten patients compared to the previous group, which was not submitted upon tonsillectomy.
The demographic profile of the patients consisted of children with a mean age of 5.04 years (ranging from 4 to 7 years) upon surgical intervention. Seven were female and nine male. The SRT averages and that of the four tones thresholds for the speech area (LQ) are shown in Table 1.
All patients presented a conductive loss in the preoperative audiometry. The average preoperative audiogram shows the presence of a mean air-osseous gap of 25.1 dB in the right ear and of 27.3 dB in the left ear (Picture 1).
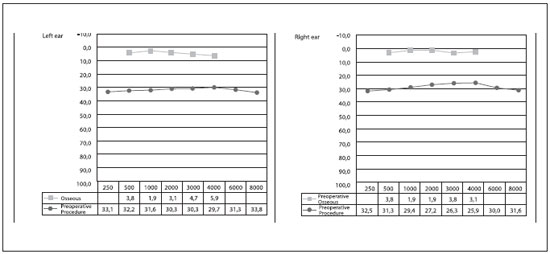
Picture 1. Pre-operative average audiogram (dB).
In the postoperative the patients present with a SRT significant improvement, ranging from an average of 28.75 dB to 13 dB, without difference between the ears (Picture 2).
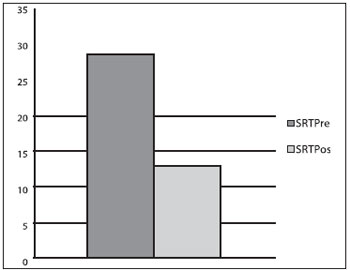
Picture 2. Comparison of preoperative and postoperative SRT (dB).
There was also an improvement to all tonal auditory thresholds with an average of 19 dB in gain at the evaluated frequencies (Picture 3).
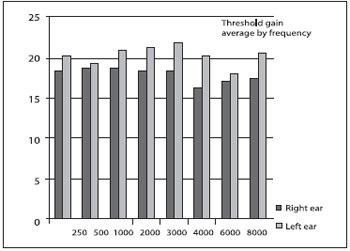
Picture 3. Average threshold gain per frequency (dB).
The air-osseous gap upon the postoperative was on average 6.8 dB in the right ear and 7 dB in the left ear, considered to be normal. The audiogram improvement was generally of 19.4 dB (Picture 4).
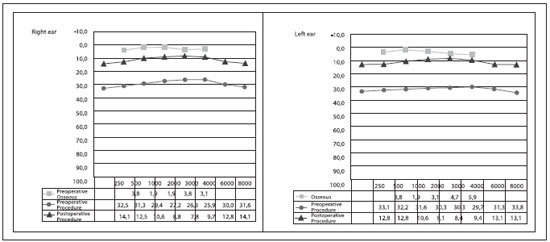
Picture 4. Comparison of preoperative and postoperative average audiograms (dB).
The SRT averages and that of the four tones thresholds for the speech area (LQ) in the postoperative are shown in Table 2.
DISCUSSIONThe OME is a disease with high prevalence in children and presents a large spectrum of clinical manifestations, which makes the diagnosis difficult.
The epidemiology is of difficult estimative for the transitory nature of the OMA episodes or the upper airways infections in this age range. In a prospective study, Tos (6) found a cumulative incidence of 91% in children younger than two years. In the older children, between two and six years, it was of 61%. The criteria used for characterization of the picture was the presence of a tympanometric curve of type B, otoscopy showing liquid at the OM and absence of acute infection signals.
Obesity may be associated to a higher risk of OME, as well as the already known factors, such as cold weather, frequency at baby nurseries and lower socio-economical level (7).
The physiopathology of OME is based on the deficiency to keep the microenvironment of the middle ear free from secretions and with a pressure similar to the external environment. It generally starts with an inflammatory event. Such alterations predispose to metaplasia of the middle ear mucosa, with an increase of caliciform cells and increase of the mucin gene expression, which promotes the presence of viscous fluid and leads to clinical manifestations.
Allergy is commonly associated to OME, but such association still needs evidence.
The clinical manifestations are not so evident because the children have a difficulty to express the symptoms. The hypacusis is one of the symptoms that may be reported by the parents, although there is no consistency between such complaints and what is clinically observed.
The diagnosis is made through clinical history, physical exam and tympanometry. The structural changes of the tympanic membrane offer important information about the middle ear and are more well evaluated through otomicroscopy. Tympanometric curves B and C portrays a lower complacence of the MT and negative pressure in the middle ear respectively and are associated to the tube dysfunction.
The OME clinical treatment is very discussed because the studies show controversial results. The classical treatment includes the use of antibiotics and oral and topical corticosteroids, which was adopted in our study. The use of antibiotics is reasonable because there is evidence of viable bacteria in the middle ear fluid. However, such treatment allows an improvement due to the diminishing of the edema and return of the ciliary function, but for a short time, with significant recurrence rates.
In patients with transitory OME, the clinical treatment allows a full improvement of the child, generally for a moderate period, at least until the next episode of UAI. The children with established histological changes will present some improvement in the tube function and the middle ear in the general aspect, but with recurrence of the short-time disease, which keeps the OME diagnosis in the short-term consultation. Therefore, the clinical treatment helps distinguish the patients who actually need surgical treatment from those who do not.
The surgical treatment, consisting of tympanostomy and placing of ventilation tube, is indicated when the effusion persists for more than three months, in spite of the clinical treatment. It is made under general anesthesia and the patients generally have adenoid hypertrophy that is also approached in the surgical procedure. All patients included in this study had at least moderate adenoid hypertrophy, which was excised. There is no evidence of change in the rate of OME recurrence in patients who were submitted to tonsillectomy or not simultaneously with tympanostomy and insertion of ventilation tube. There was no difference between the auditory thresholds of children who were submitted to tonsillectomy compared to those who were not. The type of ventilation tube commonly used in the children with OME is that of short duration, considering the high response rate in the short and middle term of the disease. In this study we inserted the tube of Donaldson type (1021), made of silicon, of short duration, with an average expectation of extrusion in six months.
The children with OME presented an increase of the speech recognition threshold (SRT), resulting from the conductive auditory loss installed by the increase of the tympano-ossicular system impedance. Such increase - preoperative average of 28.75% dB - implies mainly the damage of school learning, because the children get disperse and do not identify verbal orders easily. The SRT average improvement to 13 dB in the postoperative shows the efficiency of the surgical treatment in the most important aspect of the follow-up of these patients, the psychosocial development.
The tonal auditory thresholds presented little variation between the children and most of them showed moderate air-osseous gaps. The gap average was of 26 dB in the different frequencies. In the postoperative, with the major admittance of the middle ear by the draining of the fluid, the curve of the air thresholds approached the osseous thresholds curve, and allowed a hearing within normality. The postoperative air-osseous gap was of 6.9 dB, within the normality.
In this study the four tone preoperative average of the children was of 29.8 dB in both ears, characterizing a light conductive loss. The literature show a percentile 50 close to 25 dB(8), with about 20% of the children presenting thresholds higher than 35 dB. In this study 8 ears presented preoperative four-tone thresholds higher than 35 dB and 46.3 was the highest. This sample represents one quarter of the children. In many children this hearing loss is responsible for the fall of school efficiency, lack of attention and social disadjustment.
The surgical approach interrupts abruptly the main factor of the conductive dysacusis, the tympano-ossicular system impedance increase upon sound transmission, for the presence of liquid, generally thick and viscous in the middle ear. The secretion removal is made under aspiration, but the noise produced in this procedure is intense and may generate acoustic trauma and transient or permanent neurosensorial hearing loss. The aspiration must then be made, as well as all the surgical procedure, carefully so as to avoid iatrogenies. Because of a change in the conditions of the middle ear, the children tend to have a quick gain of auditory thresholds, but, such information is not transmitted for the age difficulty of expression.
In the middle-term postoperative, all children presented auditory thresholds gains and the four-tone average improved as a consequence. The four-tone average in the postoperative was of 10.4 dB, considered to be normal and according to the literature, although slightly higher (9). The difference between the preoperative and postoperative averages was of 19.4 dB, significant for the child's hearing. There was no neurosensorial hearing loss in the children evaluated identified in the preoperative or postoperative.
CONCLUSIONThe OME is very prevalent in children and its diagnosis is important for identification of risk factors for learning and language development. The clinical treatment is helpful by distinguishing the cases of transient and persistent OME.
The children submitted to tympanostomy and insertion of ventilation tube evaluated in this study presented a significant improvement of the auditory thresholds, allowing for hearing within a normal range in the postoperative.
The comparative evaluation between preoperative and postoperative audiometric data is not commonly approached in the literature. Because it includes data obtained through objective exam, we believe it is an excellent way to monitor the surgical results of tympanostomy for ventilation tube in children.
BIBLIOGRAPHICAL REFERENCES1. Kenna MA. Otitis media and the new guidelines. J Otolaryngol. 2005, 34 Suppl 1:S24-32.
2. Di Francesco R, Paulucci B, Nery C, Bento RF. Craniofacial morphology and otitis media with effusion in children. Int J Pediatr Otorhinolaryngol. 2008, 72(8):1151-8.
3. Tewfik TL, Mazer B. The links between allergy and otitis media with effusion. Curr Opin Otolaryngol Head Neck Surg. 2006, 14(3):187-90.
4. Stewart MG, Ohlms LA, Friedman EM, Sulek M, Duncan NO 3rd, Fernandez AD, Bautista MH. Is parental perception an accurate predictor of childhood hearing loss? A prospective study. Otolaryngol Head Neck Surg. 1999, 120(3):340-4.
5. Rosenfeld RM, Culpepper L, Doyle KJ, Grundfast KM, Hoberman A, Kenna MA ET al. Clinical practice guideline: Otitis media with effusion. Otolaryngol Head Neck Surg. 2004, 130(5 Suppl):S95-118.
6. Cayé-Thomasen P, Stangerup SE, Jørgensen G, Drozdziewic D, Bonding P, Tos M. Myringotomy versus ventilation tubes in secretory otitis media: eardrum pathology, hearing, and eustachian tube function 25 years after treatment. Otol Neurotol. 2008, 29(5):649-57.
7. Kim JB, Park DC, Cha CI, Yeo SG. Relationship Between Pediatric Obesity and Otitis Media With Effusion. Arch Otolaryngol Head Neck Surg. 2007, 133(4):379-82.
8. Olusesi AD. Otitis media as a cause of significant hearing loss among Nigerians. Int J Pediatr Otorhinolaryngol. 2008, 72(6):787-92.
9. Valtonen H, Tuomilehto H, Qvarnberg Y, Nuutinen J. A 14-year prospective follow-up study of children treated early in life with tympanostomy tubes: Part 1: Clinical outcomes. Arch Otolaryngol Head Neck Surg. 2005, 131(4):293-8.
1. Graduation in Medicine/UFMG. Resident Doctor in Otorhinolaryngology.
2. Otorhinolaryngologist Doctor. Assistant Doctor of the Otorhinolaryngological Clinic of the Armed Forces Hospital.
3. Graduation in Medicine/UFMS. Resident Doctor in Otorhinolaryngology.
4. Phonoaudiologist for the Armed Forces Hospital.
5. Master's Degree in Health Sciences - University of Brasília. Coordinator of the Medical Residence Program of Otorhinolaryngology of the Armed Forces Hospital.
Institution: Hospital das Forças Armadas - Brasília. Brasília / DF - Brazil.
Mail address:
Henrique Fernandes de Oliveira
Hospital das Forças Armadas
Avenida Contorno do Bosque s/n
Clínica de Otorrino Cruzeiro Novo
Brasília / DF - Brazil - CEP: 70658-900
Phone: (+55 61) 3966-2350 / 8185-6177
E-mail: hfdoliveira@yahoo.com.br
Article received on May 24 2009.
Accepted on June 09 2009.