INTRODUCTION The fibrous dysplasia (FD) is an uncommon pseudotumor, of benign and recurrent nature, with a still unknown etiology. It consists of the replacement of the normal bone for a disorganized fibrous tissue containing immature osteoid trabeculas, similar to Chinese characters. This tumor affects mostly white race individuals, during the childhood and adolescence, with a discreet predilection for the female sex (1,2).
It is specially important in otorhinolaryngology for being uncommon, with unspecific symptomatology, which often leads to a late diagnosis for the low suspicion. It has a predilection for facial and cranial bones and may also affect long bones. The FD generally has an asymptomatic course due to the low growth and tendency for stabilization after puberty (1,2). Only in a few cases has it an aggressive behavior, and causes anatomic disorders and deformities (3,4,5). The malignant transformation is observed in 1% of the cases (6,7).
This article describes two unusual manifestations of fibrous dysplasia characterized by the early recurrences with an extensive affection of the paranasal sinuses and aggressive behavior with orbitary and cranial base invasion.
CASE REPORT Case 1: Male patient aged 7 years, with complaint of moderate frontal headache, vertigo and recurrent epistaxis for 2 years. He evolves with self-mutilating psychiatric alterations, obstruction and enlarging of the nasal base; in addition to left exophthalmia, without visual deficit. The nasal obstruction, initially to the left, progressed contralaterally and damaged breathing and sleep. Computed Tomography (CT) was carried out in August 2002, which confirmed the expansive lesion with osseous density and ground glass appearance, with isocenter in nasal cavities, and suggested fibrous dysplasia. It expanded upwards to the ethmoidal sinuses and the anterior cranial cavity. Downwards, there was an enlargement and invasion of the left maxillary infundibulum and; in the middle it displaced the left orbit medial wall and caused compression on the medial rectus muscle and I degree bulbar proptosis. He was submitted to antrectomy and orbitary decompression to the left. The histopathological diagnosis confirmed normal osseous replacement for fibrous tissue containing immature and disorganized osteoid trabeculas. One year after the surgery, the symptoms returned. A new CT confirmed an expansive process with osseous density at ethmoidal level, part of the sphenoid bone and nasal cavities, that involved the left orbit and frontal sinus, as well as an infection of the left maxillary sinus (Picture 1). An antrectomy was carried out in 2004. After six months of follow up, there was no clinical nor radiologic abnormalities. However, there was a new recurrence after one year of follow up, with the facial CT showing a recurrent lesion in the left maxillary and sphenoid sinuses, ethmoidal and frontal sinuses (Picture 2). He was again submitted to surgery and there was a new recurrence in 2007. The paranasal sinuses CT showed hyperostosis on the facial bones with ground glass appearance, that suggested fibrous dysplasia. A fourth surgery was carried out in January 2008, that consisted of an ethmoid-maxilarectomy via degloving and bilateral frontal craniotomy for resection of the lesion affecting the sphenoid. The histopathological exam diagnosed fibrous dysplasia (Picture 3). The patient evolved well without signs of liquoric fistula and with improvement of the facial deformity.
Case 2: 25-year-old female patient with history of moderate pain and convexity in the maxillary and zygomatic region for 2 years. In June 2007, the facial sinuses CT revealed a solid lesion to the left that invaded the maxillary sinus with extension to the orbit, frontal and ethmoidal sinus, nasal cavity and ipsilateral pharynx, as well as osseous destruction and proptosis of the left ocular globe (Picture 4). She was submitted to upper left maxillary osteotomy. The histopathological diagnosis confirmed normal osseous replacement for fibrous tissue containing immature and disorganized osteoid trabeculas. Eight months after the surgery, the symptoms returned, and there was a new recurrence, with CT showing a lesion in the left maxillary sinus, ethmoidal and frontal sinuses and proptosis in the left ocular globe. In April 2008, a new osteotomy of the left upper maxilla was performed with resection of the expansive lesion. The histopathological exam diagnosed fibrous dysplasia. The patient evolved without complaints and improvement of the facial deformity.
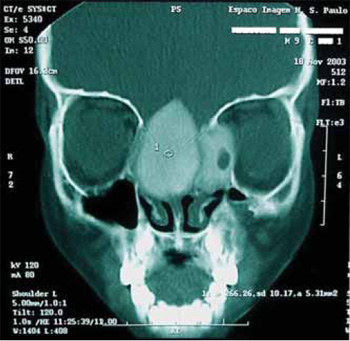
Picture 1. Computed Tomography coronal cut showing a tumor affecting the ethmoid, sphenoid, nasal cavities, left orbit and frontal sinus, as well as the left anthro maxillary.
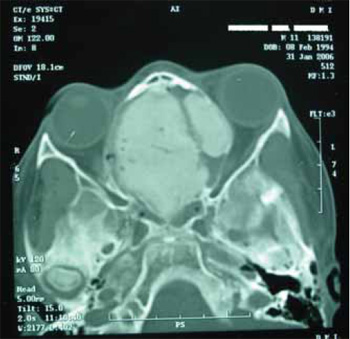
Picture 2. Computed tomography axial cut confirming an expansive lesion with osseous density and recurrent ground glass appearance affecting the ethmoidal sinuses and anterior cranial cavity, invasion of the left maxillary infundibulum and displacing the left orbit medial wall with bulbar proptosis.
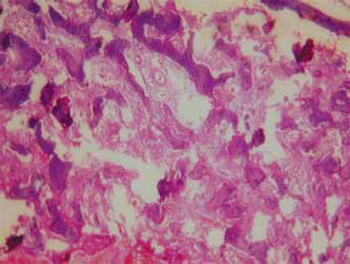
Picture 3. The histopathological diagnosis confirmed normal osseous replacement for fibrous tissue containing immature and disorganized osteoid trabeculas (40X).
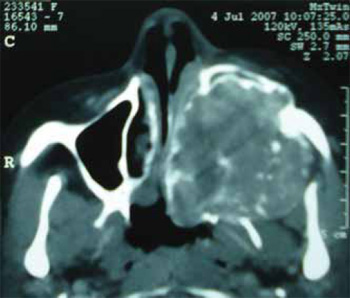
Picture 4. Computed tomography axial cut showing a tumor at the left, invading the maxillary sinus with extension orbit, frontal and ethmoidal sinus, nasal cavity and ipsilateral pharynx, as well as osseous destruction and proptosis of the left ocular globe.
The fibrous dysplasia is an uncommon benign tumor lesion of recurrent nature with a still unknown etiology. It consists of an alteration of the osseous maturation, and there is normal bone substitution by a disorganized fibrous tissue that contains immature curvilinear osteoid trabeculas, similar to Chinese letters (1). The craniofacial FD represents approximately 2.5% of the osseous tumors and 7.5% of the benign osseous tumors. It affects mostly white individuals, with a discreet predilection for the female sex (2).
The fibrous dysplasia presents two clinical standards. The monostotic standard is more frequent and corresponds to 70% of the cases; it occurs in a single bone or in contiguous bones. The polyostotic standard is found when several bones are affected. A specific form is called In both cases presented, there was a contiguous McCune-Albright's syndrome, consists of the polyostotic affection restricted to the craniofacial bones and type followed by cutaneous hyperpigmentation and early corresponding to the monostotic standard. In spite of being puberty, and is responsible for 3% of the cases with frequent, the affection of these bones in the monostotic prevalence of the female sex (1,2,3). form is less common, since the FD has a predilection for long bones (such as ribs, femur and tibia). The craniofacial involvement hits 25% in the monostotic and 50% in the polyostotic standard (1). In the face, the maxilla is the most affected bone, followed by the jaw. The frontal, temporal and clivus bones are less affected (10). The extension to the orbit is rare, and the cranial base invasion is an uncommon event (4,5,10,12).
Because they are uncommon tumors, with unspecific symptomatology and affect craniofacial bones, they have a special importance for otorhinolaryngology. The diagnosis is generally late for its low suspicion (1). When monostotic, the FD generally presents an asymptomatic or slight symptoms course, with insidious growth and tendency for stabilization after puberty. The discovery is usually incidental. Only in a few cases can it have a more aggressive growth, with quick growth, and provoke pain, nasal obstruction and exophthalmia. The polyostotic form is associated to a progressive affection, high probability of complications and recurrences at the adult age (3,4,5,12). In the cases reported, the symptoms started approximately 2 years before (nasal obstruction, headache, vertigo). These are unspecific and insidious pictures that evolved with aesthetic alterations, such as convexity of the nasal pyramid and ocular proptosis.
In advanced stages, the FD causes deformities and disorders, so that the symptoms relate to the affected area. The main symptoms are neurosensorial dysacusis, stenosis of the auditory meatus, unilateral and bilateral nasal obstruction, intense headache, exophthalmia (4,5,12). There may also be commitment of the trigeminal, facial nerves and other cranial pairs (2.9). The malignant transformation is observed in 1% of the cases, generally for osteosarcoma (6,7).
The imaging methods are critical for the characterization of the lesion and analysis of the tumoral expansion, and helps the surgical planning and the longitudinal follow up of the patients operated (8). The computed tomography has a higher accuracy than simple radiography (3). The radiologic forms are described: (1) the compact form is the most common (50% of the cases) and has a homogeneous standard, with "ground glass" appearance imaging; (2) the lytic lesion has an uneven nature surrounded by a high density margin; and (3) the mixed form, that presents radiolucent areas alternating with radiopaque areas (2,3,8).
The main differential diagnosis are: hyperostosis, osteoma, osteosarcoma, cordoma, hyperostotic menyngioma, brown tumor of the hyperthyroidism and ossifying fibroma (1.3). The latter is important for the clinical and radiologic similarity and must be diagnosed by histopathological exam (3.14).
Patients with small asymptomatic lesions require a follow up and there is no need for resection or surgical reconstruction. We must perform biopsy for diagnostic confirmation and a strict follow up with control CT. The surgical strategy is indicated for symptomatic lesions and it may be carried out at any age in case of stressed disorder or extensive affection. Many times it is not possible to perform the full excision of the lesions due to the degree of affection and the non-designing of tumoral margins (2.9). The fibrous dysplasia does not respond to radiotherapy and is considered to be a factor for malignization of the lesion (10).
In both cases described there was organic dysfunction and extensive tumoral invasion causing facial deformities, hence the choice of surgical intervention. In the first case, we carried out ethmoid-maxilarectomy via degloving followed by bilateral frontal craniotomy for tumoral excision that invaded the cranial base. In the second case, we opted for upper maxillary antrectomy for tumoral resection. Both patients evolved with remission of the symptoms, good aesthetic results and did not present with new recurrences during the postoperative follow up.
The osseous reconstructions are favorable in case of anatomic distortions, functional alterations and compression of cranial nerves, and more indicated after stabilization of the tumoral growth and must be immediately performed after a large resection of the osseous lesions (9). The autologous osseous grafts or synthetic methylmetacrilate. The results are promising when helped by new technologies in the surgical planning such as the virtual three dimensions (3D) computed tomography (15,16).
Currently, the modified intranasal endoscopic procedure of Lothrop has been used in the treatment of chronic sinusitis and tumors of the frontal sinus. It offers advantages on the open techniques for the minor surgical time and hospital permanence in the postoperative, as well as less intraoperative and postoperative complications (11).
FINAL COMMENTS The fibrous dysplasia is an uncommon osteopathy with unknown etiology. It is important for otorhinolaryngology because it affects craniofacial bones, and the maxilla is the most affected bone in the face. It has an unspecific symptomatology and the orbitary invasion is a rare event. The monostotic has an asymptomatic course, with a slow growth and stabilization after puberty, and only needs follow up. The polyostotic type has a progressive behavior and associates with complications and recurrences. The tomography is the choice in the characterization of the tumoral expansion, and helps in the surgical planning. The surgical strategy is indicated in symptomatic lesions, functional alterations and anatomic distortions. Endoscopic resections offer the advantages on the open techniques for being minimally invasive, with less intraoperative and postoperative complications. New techniques and osseous reconstructions from autologous or synthetic osseous grafts guided by 3D computed tomography for the surgical planning have been showing promising aesthetic and functional results.
BIBLIOGRAPHIC REFERENCES 1. Rosenberg A. Ossos, Articulações e Tumores de Partes Moles. Em: Cotran RS, Kumar V, Robbins ST. Patologia estrutural e funcional. 6ª ed. Rio de Janeiro: Guanabara Koogan; 2000. p. 1087-1134.
2. Jan M, Dweik A, Destrieux C, Djebbari Y. Fronto-orbital sphenoidal fibrous dysplasia. Neurosurgery. 1994, 34(3):544-547.
3. Alves AL, Canavarros F, Vilela DSA, Granato L, Próspero JD. Displasia fibrosa: relato de três casos. Rev Bras Otorrinolaringol. 2002, 68(2):288-292.
4. Júnior VS, Andrade EC, Didoni ALS, Jorge JC, Filho NS, Yoshimoto FR. Displasia fibrosa do osso temporal: relato de caso e revisão da literatura. Rev Bras Otorrinolaringol. 2004, 70(6):828-831.
5. Falavigna A, Borba LAB, Teles AR. Displasia fibrosa do clivus. Arq Neuropsiquiatr. 2006, 64(2):329-333.
6. Brownbill D, Snell JA. A case of malignant transformation in fibrous dysplasia. Aust N Z J Surg. 1967, 36(3):254-255.
7. Schwartz DT, Alpert M. The malignant transformation of fibrous dysplasia. Am J Med Sci. 1969, 247:1-20.
8. Botelho RA, Tornin OS, Yamashiro I, Menezes MC, Furlan S, Ridelenski M, et al. Características tomográficas da displasia fibrosa craniofacial: estudo retrospectivo de 14 casos. Radiol Bras. 2006, 39(4):269-272.
9. Sharma RR, Mahapatra AK, Pawar SJ, Lad SD, Athale SD, Musa MM. Symptomatic cranial fibrous dysplasias: clinicoradiological analysis in a series of eight operative cases with follow-up results. J Clin Neuroscienc. 2002, 9(4):381-390.
10. Sottano CA, Garcia CRM, Valdivia ODV, Paiva LJ. Displasia fibrosa craniofacial: estudo de 14 casos. Rev Bras Otorrinolaringol. 1979, 45(2):164-169.
11. Charlett SD, Mackay SG, Sacks R. Endoscopic treatment of fibrous dysplasia confined to the frontal sinus. Otolaryngol Head Neck Surg. 2007, 136(4):59-61.
12. Oliveira RCB, Granato L, Korn GP, Marcon MA, Cunha AP. Displasia fibrosa do osso temporal: relato de dois casos. Rev Bras Otorrinolaringol. 2004, 70(5):695-700.
13. Lupescu I, Hermier M, Georgescu SA, Froment JC. Helical CT and diagnostic evaluation of cranio-facial fibrous dysplasia. J Radiol. 2001, 82(2):145-149.
14. Voytek TM, Ro JY, Edeiken J, Ayala AG. Fibrous dysplasia and cemento-ossifying fibroma. A histologic spectrum. Am J Surg Pathol. 1995, 19(7):775-781.
15. Murray DJ, Edwads G, Mainprize JG, Antonyshyn O. Advanced technology in the management of fibrous dysplasia. J Plast Reconstr Aesthet Surg. 2008, 61(8):906-916.
16. Chowdhury K, Schramm VL. Fibrous Dysplasia of the sinuses and orbit: surgical techniques. Otolaryngol Head Neck Surg. 1999, 10(2):113-120.
2. Graduation. Resident Doctor of General Surgery of the Federal University of Piauí.
3. Doctoral Degree. Assistant Professor Doctor of the Head and Neck Surgery Service of the Federal University of Piauí, Teresina, Piauí, Brazil.
Institution: Serviço de Cirurgia de Cabeça e Pescoço da Universidade Federal do Piauí. Teresina / PI - Brazil. Mail Address: Vítor Yamashiro Rocha Soares - Rua Deusa Rocha, 2076 - Bairro: Cristo Rei Teresina / PI - Brazil - Zip Code: 64014-180 - Telephone: (+55 86) 3217-8321 - E-mail: vyrsoares@yahoo.com.br