INTRODUCTIONForeign bodies (FB) are frequent reasons of consultations in Otorhinolaryngology. The most commonly affected sites are the nasal cavity, ears and oropharynx. In these regions the foreign bodies have characteristic symptoms and their removal does not represent a great difficulty for the specialist. The inoculation form may be voluntary or accidental (1,2,3).
According to several authors (1,4,5,6), the FB correspond, on average, to 11% of the cases of Emergencies in Otorhinolaryngology and may evolve with complications in 22% of the cases. Such complications are mostly simple, but eventually more severe pictures such as tympanic perforations and bronchoaspiration may occur (6,7).
Several factors are critical for the occurrence of complications, like the attempt to remove by onlookers and unskilled health professionals; the inexperience of the clinician in the handling of foreign bodies; lack of suitable hospital infrastructure; poor structuring of the public network for Otorhinolaryngology Emergencies and long permanence of the foreign body (1,6,8).
The great potential for complications during the removal of such foreign bodies makes the operation of the otorhinolaryngologist crucial in this procedure. The FB removal success depends on the patient's cooperation, the doctor's ability, the type of FB, the previous manipulation, the visibility and depth of the FB and the available equipment (2).
Because the occurrence of FB involving the nasal cavities, ears and oropharynx is a reason for frequent consultations in otorhinolaryngology emergency services, its time of permanence is what will determine the symptomatology, since the cases of FB are seldom asymptomatic. In the nasal cavities, the symptoms start with sneezes, hyaline rhinorrhea and nasal obstruction, and evolves within some days into unilateral fetid and purulent rhinorrhea. In the ears the picture may start with hypacusis, otorrhagia, otorrhea or tinnitus. In the oropharynx, the main symptom is odinophagia (1,2).
As for the modes of insertion of the FB, we may divide them into voluntary or accidental. The voluntary insertion occurs mainly in children and the accidental, more common in adults, is represented by living animals, and the myiasis is commonly found and associated to the most severe complications (2,9). The first years of life are for children a phase of exploitation and interaction with the environment. When she begins to crawl and/or walk, the child begins to have access to a large variety of objects, which she ends up, by curiosity putting into more exposed holes such as ear, nose and oropharynx (10).
The shape and the size of the objects found to be FB may determine the difficulty for removal. In the ear FB there may occur complications due to the small dimensions of the external acoustic meatus and the vicinity of important structures (2,4). The removal becomes difficult when the FB is close to the tympanic membrane, due to the risk of its perforation. Among the most frequent complications, we may find: laceration of the external acoustic meatus, tympanic perforation, external otitis and hematoma. The cases of nasal cavity FB may evolve into epistaxis, septal perforation and rhinosinusitis according to their time of evolution and location (1,2).
The objective of this study is to describe a number of patients with foreign bodies in the Otorhinolaryngology Service of the Hospital Paulista de Otorrinolaringologia - São Paulo, as well as to evaluate the clinical picture and the treatment in such cases and their complications.
METHOD We carried out a prospective analysis of 128 patients with diagnosis of nose, ear and oropharynx foreign body, attended in the emergency room of the Hospital Paulista de Otorrinolaringologia, São Paulo, in the period from August 2005 through august 2007.
We took into consideration the age, sex, location of the foreign body, time of insertion and removal of the foreign body, type of foreign body, complications and most common symptoms.
The material used for removal of foreign bodies includes nasal and auricular specula, Bruenings tongue depressor, flexible and rigid optical fibers of 4mm of diameter (70o, 0o and 30o), Kelly and bayonet tweezers, optical fiber laryngoscope, Hartmann and alligator tweezers, leak and sharp hooks, ear washing syringes and electric ear washer. In only 12 patients (9.3%) there was the need for removal in the surgical center with general anesthesia.
RESULTSWe analyzed 128 cases of FB in otorhinolaryngology: 86 (67.18%) cases of ear; 24 (18.75%) of nasal cavity and 18 (14.07%) of oropharynx (Graphic 1). As for the sex of the patients we verified 71 (55.47%) cases of men and 57 (44.53%) of women. The age ranged from 2 -78 years and the mean age was of 17 years. Out of the age ranges, 41 patients (32.03%) were in the 0-10 years age range, 9 (7.03%) between 11-20 years, 74 (57.81%) between 21-59 years and only 4 (3.15%) older than 60 years (Table 1).
The evolution time average was of 12.2 days, and 73 (57.03%) cases were attended with less than 24 hours of evolution. From the total of patients, 83 (64.85%) received initial service in the Emergency Room of the Hospital Paulista and 45 (35.15%) had been sent from another service after some previous removal attempt. The cases of FB in the ear presented an evolution time average of 11.76 days. The cases of FB in the nose presented an evolution time average of 38.03 days. For the cases of FB in the oropharynx, the average was of only 1.83 days.
According to the location, out of the 86 auricular FB, 45 (52.32%) were inserted in the right ear, 39 (45.34%) in the left ear and 2 (2.34%) in both ears. In the nose FB 9 (37.5%) involved the right nostril and 14 (58.33%) the left nostril and only 1 (4.17%) involved both nostrils. Out of the cases of oropharynx FB, 5 (27.77%) occurred in the right tonsil, 7 (38.88%) in the left tonsil and 6 (33.33%) in the basioglossus region.
Among the auricular FB 44 (51.16%) were removed with alligator tweezers; 29 (33.73%) with ear irrigation with warm water by means of syringe or electric ear washer; 5 (5.82%) with otological curette for earwax and 8 (9.31%) cases required removal in the surgical center. Out of 24 patients with nasal FB, 18 (75%) were submitted to extraction with Itard probe; 5 (20.83%) with alligator or bayonet tweezers and only 1 (4.17%) required removal at the surgical center. As for the oropharynx cases, 15 (83.33%) were removed with Hartmann tweezers and in some cases it was necessary to use (flexible and/or rigid) optical fiber to improve visibility, and in 3 (16.67%) cases it was only possible in the surgical center by means of general anesthesia. The 12 (9.37%) cases that required forwarding to the surgical center with the help of general anesthesia, it was due specially to the lack of collaboration of the patients, mainly in the children and in the cases of oropharynx due to the intense nauseous reflex.
The most common symptoms of the ear FB cases were hypacusis with 34 (39.53%) cases and earache with 21 (24.41%) cases. In the nasal FB, the unilateral rhinorrhea was present in 9 (37.5%) cases and cacosmia in 6 (25%) cases. In the oropharynx FB, the main symptom was odinophagia with 16 (88.88%) cases (Table 2).
The most frequent ear FB was cotton, with 37 (43.02%) cases, followed by plastic artifact with 16 (18.60%) cases. In the most frequent FB in the nasal cavity, we found the same number of fragments of brush and paper with 8 (33.33%) cases each. In the oral cavity the most common was fish-bone, with 13 (72.22%) cases (Table 3).
Only 18 (14.06%) cases of complications were found, resulting from the presence of the FB or from their manipulation. Out of the ear FB cases, 9 (7.03%) cases presented with acute external otitis; 3 (2.34%) cases had laceration of the external auditory meatus and only one (0.78%) case of tympanic perforation. In the nasal FB, 4 (3.12%) cases evolved into rhinosinusitis and one (0.78%) case into epistaxis. The cases of FB of the oropharynx region no complications were found (Graphic 2).
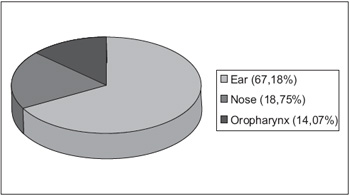
Graphic 1. Distribution of the foreign bodies in otorhinolaryngology
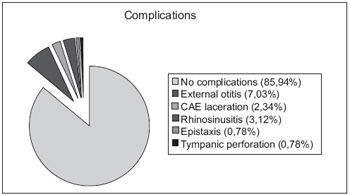
Graphic 2. Frequency and types of existing complications for removal of foreign body.
The otorhinolaryngologists deal with a major parcel of natural corporeal holes by which the foreign bodies may be introduced, such as: ear, nose and mouth. The esophagus and the lower airways are indirectly reached, since the foreign bodies must first pass through the pharynx or the nasal cavities. Some authors stand out that the oropharynx and nasal cavities FB are potential esophageal and bronchial FB (1,7,8). We thus know that such accidents may lead to severe complications and even to death, although in this study we did not observe any fatal outcome.
Our data agree with the literature (2,5,8,11,12,13) concerning the location of the foreign bodies, with predominance in ears, followed by the nasal region and oropharynx. As for sex, compared to other authors (2,5,8), we found no statistically significant differences.
The distribution by age range shows a clear predominance of FB in the nasal region in children, which was also confirmed in other studies (1,2,8,14). We observed the incidence diminishing according to the age increase. Such fact may be explained by the curiosity and discovery concerning the body. With growth and cognitive development, the introduction of FB in the nostrils diminishes significantly, which is found only in patients with psychiatric disorders (2,15). But the foreign bodies in oropharynx are mostly found in adults, while those in the ear show a more balanced distribution, which disagrees with the literature (2,8,11,16).
The time of evolution was lower than 24 hours in 57.03% of the cases, similar to that found in the studies by IKINO et al (1998) and TIAGO et al (2006). The oropharynx FB evolution time average was of only 1.82 days, which may be explained by the discomfort due to the presence of FB in this region. The cases of FB in the nose was the one that mostly presented a high average of evolution time with 39.03 days, as that of ear FB was of 11.76 days.
The high incidence of fish-bone as oropharynx foreign bodies reflects the lack of care and attention in the preparation of food and chewing, mainly with small fish. In the cases of ear FB, the cotton was the mostly found, mainly for the habit of the population to use cotton swabs for cleaning and relief of otological pruritus. In children we found more varied plastic fragments, since piece of toys, buttons, up to glass beads, etc. Sponge and paper fragments, generally removed from pillows, mattress, books and notebooks were the mostly found nasal foreign bodies. The case of animated foreign body in our study represented only 5 cases, all in patients older than 20 years old.
The most common symptoms of the ear FB cases were hypacusis with 39.53% of the cases and earache with 24.41% of the cases. In the nasal FB, the unilateral rhinorrhea was present in 37.5% of the cases and cacosmia in 25% of the cases. In the oropharynx FB, the main symptom was odinophagia with 88.88% of the cases, due to the extreme discomfort, aiming to seek early service.
The materials and methods used for removal of the FB from the ear, nose and oropharynx were similar to those presented in studies by MARQUES et al (1998) and TIAGO et al (2006). Only in 9.37% of the cases it was necessary to lead to the surgical center with the help of general anesthesia, it was due specially to the lack of collaboration of the patients, mainly in the children and in the cases of oropharynx due to the intense nauseous reflex. What was shown in the other studies was that the relationship between the need for general anesthesia for removal of FB ranged from 8.6 to 30% (17).
We found complications in 14.06% of the cases. Most authors verified a higher incidence of complication in cases previously manipulated by physicians of other specialty, other health professionals, the own patient and even other laypeople.
In our study, the most frequent complications were of acute external otitis (7.03%) evolving into earache, and the treatment was made with topical drops, and symptomatic: acute rhinosinusitis (3.12%) with purulent rhinorrhea and nasal obstruction, for which we prescribed systemic antibiotics for 14 days and nasal washing with physiologic solution, laceration of the external auditory meatus (EAM) with 2.34%, epistaxis (0.78%) of low quantity, that did not require any contention mechanism, and tympanic perforation (0.78%) that was treated and followed up in the service.
CONCLUSIONWith this study we observed that most cases with prior manipulation for removal of the foreign body by unskilled professional or by laypeople evolved into complications and showed that the management of such patients must be carried out by the otorhinolaryngologist and with the use of suitable material.
The large number of cases of foreign body in the ear, nose and throat are easily solved; but it is critical to remark that in cases where there is technical difficulty or lack of cooperation of the patient, we must choose the removal in a surgical center under sedation or general anesthesia, by thus avoiding iatrogenic complications.
BIBLIOGRAPHICAL REFERENCES1. Marques MPC, Sayuri MC, Nogueira MD, Nogueirol RB, Maestri VC. Tratamento dos corpos estranhos otorrinolaringológicos: um estudo prospectivo. Rev Bras Otorrinolaringol. 1998, 64:42-7.
2. Tiago MPC, Salgado DC, Correa JP, Pio MRB, Lambert EE. Corpo estranho de orelha, nariz e orofaringe: experiência de um hospital terciário. Rev Bras Otorrinolaringol. 2006, 72:177-81.
3. Lima MM, Moreira CA, Silva VC, De Freitas MR. 34 corpos estranhos auto-inoculados em seio maxilar. Rev Bras Otorrinolaringol. 2008, 74:948.
4. Bressler K, Shelton C. Ear foreign-body removal: a review of 98 consecutive cases. Laryngoscope. 1993, 103(4PT1):367-370.
5. Hanke Filho EH, CMR, Hanke EMR, Hanke MMR. Corpos Estranhos de Nariz, Ouvidos, Faringe e Seios Paranasais. Rev Soc Otorrinolaringol RJ. 2002, 2:73-7.
6. Figueiredo R. Corpos estranhos de orelha, nariz, faringe e laringe. In: Figueiredo R. Urgências e Emergências em Otorrinolaringologia. Primeira edição, Rio de Janeiro: Editora Revinter; 2006.
7. Figueiredo RM, Machado VS. Aspiração de corpo estranho através de traqueotomia: descrição de um caso. Rev Bras Otorrinolaringol. 2005, 71(2):234-6.
8. Figueredo RR, Azevedo AA, Kós AOA, Tomita S. Complicações de corpos estranhos em Otorrinolaringologia: um estudo retrospectivo. Rev Bras Otorrinolaringol. 2008, 74:7-15.
9. Hungria H. Patologia do ouvido externo. Hungria H. Otorrinolaringologia. 8º Ed. Rio de Janeiro: Guanabara Koogan; 2000. P 363-7.
10. Reilly J. Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope. 1997, 107:17-20.
11. Austin D. Diseases of the external ear. In: Ballenger JS, JB, editor. Otorrhinolaryngology Head and Neck Surgery. 15 th ed. Baltimore: Williams & Wilkins; 1996. pp. 974-88.
12. Hughson W. Examination of the ear and of the function of hearing. In: Jackson CJ, CL, editor. Diseases of the Nose, Throat and ear. Philadelphia: W.B. Sauders Co; 1945. pp. 221-32.
13. Balbani AK, Angélico JrFV, Sanches TG, Voegels RL, Butugan O, Camara J. Atendimento para retirada de corpos estranhos de ouvido, nariz e faringe em crianças. Rev de Pediatria do centro de Estudos Prof. Pedro Alcântara - Instituto da Criança do Hosp das Clínicas da FMUSP. 1998, 20(1):8-13.
14. Figueiredo RR, Azevedo AA, Kós AOA, Tomita S. Corpos estranhos de fossas nasais: descrição de tipos e complicações em 420 casos. Rev Bras Otorrinolaringol. 2006, 72:13-23.
15. Ikino CMY, D'Antonio WEPA, Balbani APS, Sanchez TG, Butugan O. Análise dos atendimentos para retirada de corpos estranhos de ouvido e nariz em crianças. Rev Bras Otorrinolaringol. 1998, 64:379-83.
16. Stool SE, McConnel CS Jr. Foreign bodies in pediatric otolaryngology. Some diagnostic and therapeutic pointers. Clin Pediatr (Phila). 1973, 12(2):113-6.
17. Thompson SK, Wein RO, Dutcher PO. External auditory canal foreign body removal: management practices and outcomes. Laryngoscope. 2003, 113:1912-5.
1. Former-Fellow at the University of Graz - Austria.
2. Otorhinolaryngologist. In course for post-graduation at the Fundação Santa Casa de Misericórdia de São Paulo.
3. First-Year Resident at the Hospital Paulista de Otorhinolaryngology.
Institution: Hospital Paulista de Otorrinolaringologia. São Paulo / SP - Brazil. Mail Address: Breno Simões Ribeiro da Silva - Rua Dr. Diogo de Farias, 780 - Bairro Vila Clementino - São Paulo / SP - Brazil - Zip code: 04037-002 - Telephone: (+55 11) 5087-8700 - E-mail: brenosimoes21@yahoo.com.br. Article received on August 6 2009. Approved on October 1 2009.