INTRODUCTIONThe pre-surgical evaluation based on the patient's anatomy is extremely important for rhinoplasty to be successful (1,2). The type of skin, thickness of the subcutaneous tissue, support of the tip and the size, form and position of the biggest alar cartilages are extremely important when choosing the available techniques to reach a proper sharpness of the nasal tip (2,3,4,5).
The thickness of the nasal subcutaneous tissue is extremely changeable. A same noise is usually thicker in both the tip and the nasal root. It equally varies with race, and it is thicker in afro-descending patients than white patients.
The intra-domal space is regarded as the space between the highest protrusion of the biggest alar cartilages, and it is normally occupied by adipose tissue (7). The shape of the biggest alar cartilages, especially the dome (cupola) is wide and it can contribute for the width of the tip complex (6). The 30o angle of interdomal divergence and the domal arch equal to or smaller than 4 mm are considered normal.
Anatomic studies in corpses showed that barely defined box-like bulbous nasal tips show a thicker subcutaneous nasal tissue (8). However, measurement techniques of the thickness of the subcutaneous tissue in 'in vivo' patients is not standardized in literature.
The objective of this study is to evaluate the inter-observer changeability of the ultrasound method to measure the thickness of the subcutaneous tissue of the nasal tip by using a standardized technique.
METHOD47 volunteers were submitted to a nasal tip ultrasound. The inclusion criteria were: age between 18 and 70. The exclusion criteria were: previous nasal surgery, scar in the nasal tip, previous nasal trauma and presence of any disease changing the anatomy of skin, subcutaneous tissue and nasal tip cartilages.
The ultrasound exams were performed by two radiologist specialists, who used the same previously standardized exam technique. Each patient was evaluated on the same day; however, the observers could not access the results of the previously obtained measurements in order to prevent samples from being contaminated.
The equipment used to perform the ultrasound was a Medison® Sonoace 8000 SE with an electronic linear transducer at a frequency between 5 and 9 MHz. All the patients were evaluated in a dorsal decubitus position. The transducer was positioned on the nasal tip without putting any pressure on it not to underestimate affection. The thickness of the subcutaneous tissue was evaluated by measuring the point with the highest protrusion of the largest alar cartilage dome towards skin, in millimeters.
Statistical Analysis
The descriptive statistical analysis was used for a socio-demographic characterization and to calculate the averages and standard deviations of the measures achieved by the two observers. When performing Lilliefors test, the data normality was checked. Student's t test was used to compare the measures achieved by the two observers. The intraclass correlation coefficient and the respective confidence interval were used to determine the reproducibility of the measures achieved by the two observers. Bland-Altman graphic was equally used to evaluate the compliance between the measures. The level of statistical significance was defined as p < 0,05.
RESULTSThe study group was comprised of 47 patients - 16 were male and 31 were aged between 18 and 70 (average of 35 ± 14).
The ultrasound measurement of the subcutaneous tissue of the nasal tip was performed in an average of 1.2 minutes (0.9-2 minutes). The achieved measurement averages of the subcutaneous tissue of the nasal tip and their respective standard deviations were: 4.352 mm ± 0.6222 for the first examiner and 4.330 mm ±0.674 for the second examiner.
The measurement comparisons achieved by the examiners one and two did not show statistically significant differences (p = 0.5303), implying that the examiners do not disagree with each other regarding the measurements (Graphic 1). The good similarity can be confirmed by referring to the graphic of the averages. The average of differences was very low, i.e., 0.02234 mm and a standard deviation of 0.24 mm, proving the examiners excellently agree with each other.
When analyzing the reproducibility between examiners, an interclass 'r' correlation coefficient (Pearson) 0,9333 (confidence interval [IC] 95= 0.88-0.96 p < 0.0001), i.e., an excellent inter-observer reproducibility was found.

Figure 1. Ultrasound image of the nasal tip clearly showing the thickness measure of the subcutaneous tissue of the nasal tip (biggest protrusion of the largest alar cartilage dome towards skin).
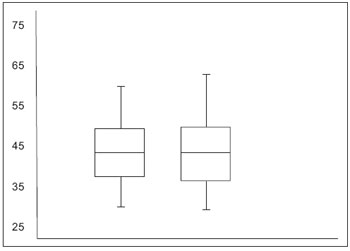
Graphic 1. Averages and standard deviation of the measures obtained by examiners 1 and 2. No significant different were observed among the averages of the three measures obtained by the examiners.
The nasal tip surgery is an extremely complex part of rhinoplasty (1). Likewise, it is influenced by factors such as type of skin, thickness of the subcutaneous tissue, tip support and size, shape and position of the biggest alar cartilages. Therefore, a detailed anatomic knowledge of this area helps surgeon plan the surgery and decide about the technique to be used, hence directly impacting the final aesthetic result (2, 3, 4).
Additionally, the thickness of the skin and subcutaneous tissue is an extremely important factor to choose the technique to be used, with a view to achieving a better sharpness of the nasal tip (5). Thus, the ultrasound analysis of the nasal tip simultaneously performed with the pre-surgical analysis can help surgeon decide abut the technique to be used for each patient.
Ultrasound exam to evaluate the nasal tip was firstly introduced by TASMAN and HELBIG in 2000, for purposes of evaluating the changes occurred on the nasal tip as a result of rhinoplasty (9). In 2004, COPCU et al. used the ultrasound to show the presence of interdomal adipose tissue as an independent structure taking the interdomal space on the nasal tip (8). COSKUN et al., in 2008, published the tridimensional ultrasound analysis of the interdomal adipose tissue by way of vertical, transverse and longitudinal measures of this structure, which was confirmed by dissection (10). However, no study was performed to accredit the method to evaluate the thickness of the subcutaneous tissue of the nasal tip.
The sharpness of the nasal tip can be achieved by several methods, including techniques of suture, resections and exertions (11,12). Choosing the technique to be used on each patient is totally dependent on the skin and the subcutaneous tissue. The suture techniques are applied to patients with thin and normal and intended to correct abnormalities of the nasal tip cartilages in those patients with box-like nasal tips (5, 13, 14, 15). Patients with bigger abnormalities of the nasal tip and thick skin are not satisfactorily approached by suture techniques. They need exertions to attain proper sharpness and enhancement of the nasal tip (16). Dome-dividing techniques can equally be necessary for patients with extremely thick skin (17,18).
Several authors agree that the best sharpness of the nasal tip must be founded on the most conservative techniques for more discreet alterations in individuals with thin skins and subcutaneous tissues, and more aggressive techniques for bigger abnormalities in patients with thick skins and subcutaneous tissues (5).
The ultrasound evaluation of the nasal tip is an objective method to identify the anatomy of this region and proved to be effective to evaluate the skin and the subcutaneous tissue of the nasal tip. The results achieved proved that there is a good reproducibility without a statistically significant difference in the measurements obtained by the examiners, making this method reliable as one more tool for the surgeon in the pre-surgical analysis and subsequently in the surgical plan.
CONCLUSIONUsing ultrasound exam to evaluate the thickness of the subcutaneous tissue proved to be reproducible and examiners satisfactorily agree. It is a non-invasive, low-cost and safe method that can help surgeon both evaluate the patient's skin and the subcutaneous tissue and choose the best surgical technique for each case.
REFERENCES1. Ghavami A, Janis JE, Acikel C, Rohrich RJ. Tip shaping in primary rhinoplasty: an algorithmic approach. Plast Reconstr Surg. 2008, 122(4):1229-1241.
2. Toriumi DM. New concepts in nasal tip contouring. Arch Facial Plast Surg. 2006, 8(3):156-185.
3. Tardy ME Jr. Graduated sculpture refinement of the nasal tip. Facial Plast Surg Clin North Am. 2004, 12(1):51-80.
4. Patrocínio LG, Carvalho PM, de Souza HM, Couto HG, Patrocínio JA. Surgical maneuvers performed on rhinoplasty procedures carried out at an otorhinolaryngology residency program. Braz J Otorhinolaryngol. 2006, 72(4):439-442.
5. Patrocínio LG, Patrocínio TG, Maniglia JV, Patrocínio JÁ. Graduated Approach to Refinement of the Nasal Lobule. Arch Facial Plast Surg. 2009, 11(4):221-229.
6. Daniel RK. The nasal tip: anatomy and aesthetics. Plast Reconstr Surg. 1992, 89(2):216-224.
7. Sun GK, Lee DS, Glasgold AI. Interdomal fat pad: An important anatomical structure in rhinoplasty. Arch Facial Plast Surg. 2000, 2:260-263.
8. Copcu E, Metin K, Ozsunar Y, Çulhaci N, Ozkök S. The interdomal fat pad of the nose: A new anatomical structure. Surg Radiol Anat. 2004, 26(1):14-18.
9. Tasman, AJ, Helbig M. Sonography of nasal tip anatomy and surgical tip refinement. Plast Reconstr Surg. 2000, 105:2573-2579.
10. Coskun N, Yavuz A, Dikici MB, Sindel T, Islamoglu K, Sindel M. Three-Dimensional Measurements of the Nasal Interdomal Fat Pad. Aesth Plast Surg. 2008, 32:262-265.
11. Crumley RL, Lanser M. Quantitative analysis of nasal tip projection. Laryngoscope. 1998, 202-208
12. Tardy M-E, Cheng E. Transdomal suture refinement of the nasal tip. Facial Plast Surg. 1997, 4:317-320
13. Guyuron B, Behmand RA. Nasal tip sutures part II: the interplays. Plast Reconstr Surg. 2003, 112:1130-45.
14. Behmand RA, Ghavami A, Guyuron B. Nasal tip sutures Part I: the evolution. Plast Reconstr Surg. 2003, 112:1125-9.
15. Pedroza F. A 20-year review of the "new domes" technique for refining the drooping nasal tip. Arch Facial Plast Surg. 2002, 4(3):157-163.
16. Pastorek NJ, Bustillo A, Murphy MR, Becker DG. The extended columellar struttip graft. Arch Facial Plast Surg. 2005, 7(3):176-184.
17. Simons RL. Vertical dome division in rhinoplasty. Otolaryngol Clin North Am. 1987, 20(4):785-796.
18. Patrocínio LG, Patrocínio JA. Open rhinoplasty in African American noses. Br J Oral Maxillofac Surg. 2007, 45(7):561-566.
1) Doctor. Otorhinolaryngology Department of the Federal University of Uberlândia's Medical School.
2) Doctor. Radiology Deparment of the Federal University of Uberlândia's Medical School.
3) Professor Doctor. Radiology Deparment of the Federal University of Uberlândia's Medical School.
4) Professor Doctor. Head of the Deparment of Junior Doctors in Otorhinolaryngology of the Federal University of Uberlândia's Medical School.
Institutition: Hospital Santa Genoveva. Uberlândia / MG - Brazil. Mailing address: Lucas Gomes Patrocinio - Rua Artur Bernardes 555, 1º Andar - Uberlândia / MG - Brazil - ZIP Code: 3840-368 - Telephone: (+55 34) 3215-1143 - Email: lucaspatrocinio@clinicaotoface.com.br
Article received on April 28,2011. Article approved on June 25, 2011.