INTRODUCTIONCongenital choanal atresia is the failure in the development of the communication between posterior nasal cavity and nasopharynx (1), initially described by Johann Roderer, in 1755 (2-8), and surgically approached by Emmert in 1851 (3,8).
The incidence is 1:5,000 to 1:8,000 per live-born children, being more frequently unilateral and in female patients (1-6,9,10). In unilateral cases, it is more frequent on the right side (5,8,11). It is related to other congenital malformations in 20% to 50% of the cases (1,4,5). The association with other changes is more common in bilateral atresia cases (1).
Choanal atresia is present in 10%1 to 30%8 of CHARGE syndrome cases. In such syndrome, the newborn child presents iris coloboma (C), heart changes (H), choanal atresia (A), retarded development and growth (R), and ear changes and/or hypoacusis (E) (1,11,12). Children carrying bilateral choanal atresia statistically have higher risks of heart changes, CHARGE syndrome, apnea and sleep obstructive hypopnea syndrome, hematological alterations and prematurity (12).
Classically, in newborn children there is respiratory discomfort which is relieved by cry and cyanosis. We should suspect newborn children who present breathing difficulty, nasal secretion and mouth breathing (8). There is hyaline or purulent rhinorrhea associated to nasal obstruction in adults (2).
Currently, CT scan of paranasal sinus is the choice exam for its diagnosis (1-3,6,11).
The transnasal technique through endoscopy has been more used for the surgical correction of choanal atresia once it offers good visualization, is less traumatic, presents lower complication rates and provides a faster post-operative recovery (5).
CASE REPORT35-year-old female patient presenting bilateral nasal obstruction, hyaline rhinorrhea, anosmia and nasal voice since childhood. She denies need for special care at birth. She reports breathing difficulty while being breastfed in childhood. There is no association with other malformations at the physical examination. She presented nasal fossa full of hyaline secretion at rhinoscopy, ogival palate at oroscopy and absence of changes at otoscopy.
The paranasal sinus CT scan revealed bilateral bone choanal atresia in axial cut (Pictute 1) and sagital cut (Picture 2). The diagnosis was confirmed through nasal endoscopy (Picture 3).

Picture 1. The paranasal sinus CT scan revealed bilateral bone choanal atresia in axial cut.

Picture 2. The paranasal sinus CT scan revealed bilateral bone choanal atresia in sagital cut.
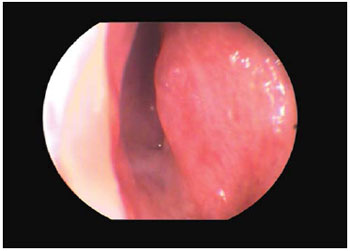
Picture 3. Nasal endoscopy of left nasal fossa proving complete closing of fossa. On the left the septal posterior part can be visualized and the inferior turbinate bottom can be seen on the right.
The surgical repair was done through crossseptal access associated to crossnasal access by endoscopic via, with the use of 30o 4.0 mm rigid telescope. The surgery was done under general anesthesia, with orotracheal intubation. Topical vasoconstriction was done in the nasal fossa with 1:2,000 adrenaline solution with the use of cottonoid, associated to infiltration of 1:100,000 adrenaline and Xylocaine solution. Rhinofarynx was protected with gauze.
The atresic plaque mucosa was incised in inverted "C" up to the lateral wall of the nasal fossa, with mucosa elevation, creating a mucoperiosteal flap. The plaque was perforated in the postero-inferior region of the medial wall (in the junction between palate, vomer and atresic plaque - thinnest region of atresia) with cutting clamp, extended with Sitelli clamp. The bone plaque and the pterigoid lateral layer were removed.
The crossseptal access was done with incision and elevation of the septal mucosa, with removal of the perpendicular layer of etmoid and posterior region of the vomer. A mucoperiosteal flap of lateral wall of the nasal fossa was placed covering the lateral wall of the new choana.
0.5 mg/ml mitomycin was applied for 5 minutes in the bloody borders. Plastic gutter was placed in both nasal fossae for 10 days. Stent was not used. Fibrin glue was not used.
Oral therapy with antibiotics was done with cephalexin for 10 days and oral corticoid was used for 5 days after the surgery. Serial nasal endoscopies were done twice a month as follow-up.
DISCUSSIONCurrently, there are 4 theories which try to explain the embryological origin of congenital choanal atresia (1,2,3-5,8,11,12):
1. Persistence of buccalpharyngeal membrane of anterior intestine;
2. Failure in the rupture of Hochstetter buconasal membrane, which generally occurs in the seventh gestational week;
3. Abnormal adherence of the mesodermal tissue in the choanal region;
4. Wrong guidance of mesodermal flow secondary to local factors.
There is a classification based on the clinical presentation of the newborn child with bilateral choanal atresia: 1. Newborn children who did not present oral respiration, having evolution with respiratory difficulty and cyclic cyanosis right after birth; 2. Eupneic newborn children, presenting dyspnea only during breastfeeding phase; 3. Assyntomatic newborn children, presenting symptoms only at adult phase (10). Such clinical degrees depend on how fast a newborn child develops the oropharyngeal respiration and learns how to coordinate oral respiration and breastfeeding, which explains who some newborn children may present no diagnosis during childhood, as it occurred in the presented case. Such classification contradicts the initial idea that all newborn children have exclusive nasal breathing until the third or fourth week of life.
Such maneuvers performed may lead to the suspicion of such pathology (2,11):
1. Non-progression of probe or catheter used in the nasal fossa of the newborn child;
2. Non-moving of cotton ball or non-condensation of mirror placed in front of the nostril;
3. Non visualization of blue methylene in the oropharynx placed in the nasal fossa.
The age in which children should undergo surgical correction remains controversial. The treatment of bilateral choanal atresia is not a surgical emergency (7). In newborn children with respiratory failure, it is essential to establish the patency of the superior air way through oropharynx way (placement of McGovern or Guedel probes) or endotracheal via (intubation, tracheotomy) (8,10,11).
Currently, CT scan of paranasal sinus is the choice exam for its diagnosis. This exams proves the kind of atresic plaque, other associated anomalies, besides helping in the surgical planning. It should always be associated to nasal endoscopy (9). The use of radiography of paranasal sinus is reported in the frontonasal, profile and Hitz incidences, with contrast in nasal fossae, producing retention of the contrast in the fossa in the cases of choanal imperforation (8).
CT scan usually proves normal aeration of paranasal sinus, confirming that the development of the sinus occurs regardless of its posterior nasal ventilation and its drainage (13), as it was confirmed in the presented case.
Studies prove that the choanal plaques may be purely osseous (30%) or membrane-osseous (70%), and that there are no exclusively membranous plaques (9).
Osseous atresia usually happens 1 to 2 mm anteriorly to the posterior border of hard palate (1). The anatomical references of the atresic plaque are: superiorly, inferior surface of sphenoid bone; laterally, the medial layer of the pterigoid process of the sphenoid; medially, the vomer; and inferiorly, the horizontal portion of the palatine bone (11).
Regardless of the surgical technique, the abnormal superior part of the vomer and part of the lateral pterigoid bone should be resected in order to create a common posterior nasal cavity (6,9). The choanal opening should be done from the region of confluence between the hard palate, the vomer and the atresic plaque once the latter in the thinnest area of the imperforation (1,6).
There are 4 main surgical accesses for the correction of choanal atresia: transnasal, transpalatal, transseptal and transantral (2,5,11,23). Currently, the most used ones are the transnasal and the transpalatal. Transnasal via must be assisted by microscope or endoscope, and several techniques may be used: serial dilatation, resection with clamp or CO
2 laser.
According to the research made in March 1999 on ASPO (
American Society of Pediatric Otolaryngology), the most used techniques, in descending order, are: transnasla with endoscope use, transpalatal, perforation with Fearon dilator, transnasal with microscope use and transnasal with laser use (10). The transasal technique is slightly better than the transpalatal technique (6,8).
The transpalatal acess described by Owens (15) and contemplated by Richardson (1) offers less re-stenosis risk (1,4), less time of stent use during the post-operative phase (1,4), higher success rates (1,3,4,6), better exposition of the surgical field (1,3,4,6), and better results in thick osseous atresic plaques (4). The success rate of this technique varies from 80% up to 90% (8). It presents some disadvantages such as further palate deformities, higher surgical time, higher bleeding risk, higher risk of palatal fistula (2,4-6,8,12), in addition to higher pain and discomfort after the surgery (11).
The transanasal surgery presents less trauma, less bleeding risk (1,6,11), less surgical time, less orthodontic complications, faster post-operative recovery and less hospitalization time (5). It presents disadvantages such as worse visualization of the surgical field when compared to the transpalatal access (1), in addition to higher re-stenosis rates (1,3).
The nasal endoscopic visualization revolutionized the surgical treatment of choanal atresia (7,11). Endoscopy enables the association of transnasal via with an excellent visualization of surgical field.
The transseptal via described by Carpenter-Neel enables the removal of the posterior portion of the vomer, the removal of the lateral pterogoid process and the simultaneous correction of potential septal defects, in addition to the correction of the atresic plaque. Gererally done only in children who are older than 8 years old to avoid precocious aggression to septal structures (5,8). This technique is specially effective in patients with choanal atresia who present thick posterior portion of vomer, associated to medial projection of the pterigoid process, determining the delta aspect (8).
The use of associated transeptal and transnasal techniques to provide excellent visualization of atresia in patients of all ages. The endoscopic view allows precision in septal, pterigoid and atresic plaque resections, besides enabling the development of the mucous flap (8). Such association is alleged in our clinic.
The use of stents in the post-operative phase, the period of its permanence and the material used are still controversional. Some authors affirm that the stent may bring trauma, stimulation to re-stenosis (10), generate lesions (septal, columella, intranasal sinequia), enable infection of paranasal sinus and bring discomfort (5,7,8). Its use in indicated in the post-operative phase, with permanence varying from 2 to 16 weeks (1,3,4,6,9,11,15). Smoother materials are preferred, once they are more sucessful when compared to the more rigid ones (3,15). The 30% re-stenosis rate is described with stent use.
New studies do not recommend the use of stents, but only the use of rotation of mucous flap to cover the bleeding area, using fibrin glue to fixate the flap (5,7,8). Stent is reported to cause necrosis of the mucous flap and higher risk of re-stenosis.
Choanal re-stenosis is one of the great problmes of choanal atresia surgery. Literature widely varies in terms of surgical failure. The re-stenosis rate varies from 0% to 85% of the cases (15). Choanes whose re-stenosis are smaller than 50% of its diameter are considered patent (7).
New studies describe the use of topical mitomycin in the choanal atresia aiming at the reduction of re-stenosis rates (12,14,15). Mitomycin is an anti-biotic and alkylant antineoplasic medication which inhibits the proliferation of fibroblasts. The recomemded concentrations of topical mitomycin cary from 0.4 up to mg/ml, for 3 to 5 minutes (14,15), applied in the bleeding borders of the new choana. The maximum non-toxic topical concentration described is 1 mg/ml.
It is described, with statistical significance, that the group which used topical mitomycin needs less dilatation in the post-operative follow-up, in addition to presenting less granulation tissue (15).
Regardless of the surgical technique used, the mucosa should be wounded as little as possible in order to avoid the formation of granulous tissue (4).
CONCLUSIONIn our experience, the transcanal access through endoscopy is the preferred via for the surgical correction of congenital choanal atresia.
In cases in which there is important thickening of the posterior portion of the vomer, the transeptal access may be associated to transnasal acess.
There is no need to use stents after the surgery, in case a mucous flap is used to cover the bleeding part of the new choana.
BIBLIOGRAPHIC REFERENCE1. Richardson MA, Osguthorpe JD. Surgical management of choanal atresia. Laryngoscope. 1988, 98(9):915-18.
2. Park AH, Brockenbrough J, Stankiewicz J. Endoscopic versus traditional approaches to choanal atresia. Otolaryngol Clin North Am. 2000, 33(1):77-90.
3. Josephson GD, Vickery CL, Giles WC, Gross CW. Transnasal endoscopic repair of congenital choanal atresia. Arch. Otolaryngol. Head Neck Surg. 1998, 124(5):537-40.
4. Hegerer AS, Strome M. Choanal atresia: a new embryologic theory and its influence on surgical management. Laryngoscope. 1982, 92(8):913-21.
5. Cedin AC, Rocha JrFP, Deppermann MB, Manzano PAM, Murao M, Shimuta AS. Transnasal endoscopic surgery of choanal atresia without the use of stents. Laryngoscope. 2002, 112(4):750-52.
6. Khafagy Y. Endoscopic repair of bilateral congenital choanal atresia. Laryngoscope. 2002, 112(2):316-9.
7. Schom S. Transnasal endoscopic repair of choanal atresia: why stent? Arch Otolaryngol Head Neck Surg. 2004, 131:362-6.
8. Cedin A, Fujita R, Cruz OLM. Endoscopic transeptal surgery for choanal atresia with a stentless folded-over-flsp technique. Otolaryngol Head Neck Surg. 2006, 135:693-98.
9. Brown OE, Pownell P, Manning SC. Choanal atresia: a new anatomc classification and clinical management applications. Laryngoscope. 1996, 106(1):97-101.
10. Chung D, Lessa MM, Lorenzetti FT, Goto EY, Voegels RL, Butugan O. Atresia congenital bilateral de coanas em paciente de 13 anos: relato de caso. Rev Bras Otorrinolaringol. 2001, 67(4):586-90.
11. Antunes A, Macedo GRM, Oliveira Jr GA, Leão RS, Caldas N. Atresia de coanas-tratamento por via endoscópica transnasal. Int Arch Otorhinolaryngol. 2002, 6(4):205-10.
12. Samedi D, Shah U, Handler S. Choanal atresia: a twenty-year review of medical comorbidities and surgical outcomes. Laryngoscope. 2003, 113(2):254-58.
13. Behar PM, Todd W. Paranasal sinus development and choanal atresia. Arch Otolaryngol Head Neck Surg. 2000, 126(2):155-57.
14. Prasad M, Ward RF, April M, Bent J, Froehlich P. Topical mitomycin as an adjunct to choanal atresia repair. Arch Otolaryngol Head Neck Surg. 2002, 128(4):398-400.
15. Holland BW, McGuirt WF. Surgical management of choanal atresia - Improved outcome using mitomycin. Arch Otolaryngol Head Neck Surg. 2001, 127(11):1375-80.
1. Resident Medical Doctor of the Otorrhinolaryngology Clinic of Hospital dos Servidores do Estado do Rio de Janeiro.
2. Medical Doctor of the Clinical Board of the Otorrhinolaryngology Clinic of Hospital dos Servidores do Estado do Rio de Janeiro.
3. Master's Degree on Otorrhinolaryngology by Universidade Federal do Rio de Janeiro. Assistant Professor of the Otorrhinolaryngology Clinic of the Medicine School of Universidade Federal do Rio de Janeiro.
4. Master's Degree Student by Universidade Federal do Rio de Janeiro. Medical Doctor of the Clinical Board of the Otorrhinolaryngology Clinic of Hospital dos Servidores do Estado do Rio de Janeiro.
Institution: Hospital dos Servidores do Estado do Rio de Janeiro.Rio de Janeiro / RJ - Brazil.
Mail address:
Andreia Ellery Frota
Rua Sacadura Cabral 178 - Saúde
Rio de Janeiro / RJ - Brazil - Zip-code: 20221-903
Telephone: (+55 21) 22913131 ramal 3771
E-mail: andreiaelleryfrota@gmail.com / andreiaelleryfrota@yahoo.com.br
Article received on September 5, 2007.
Article approved on December 27, 2007