INTRODUCTIONAccording to WHO's data, in Brazil, around 2,250,000 inhabitants have a hearing deficit, corresponding to 1.5% of population (1). To serve this population, the Unified Health System (SUS) launched the Auditory Health Service comprising a screening and monitoring newborn's hearing and that of children in kindergarten and at school; a diagnosis of hearing loss in 3-year-old children or older, teenagers and adults (workers and elderly), meeting the requirements for each of these conditions (2).
Hearing loss can be considered one of the most devastating losses regarding the individual's social living. In adults, the impact of this type of auditory alteration can be associated with the cognitive decline, depression and a reduction of the functional state, mainly for those having loss but who were not evaluated or treated (3).
Accordingly, surveying the individuals with a hearing difficulty in a community, their location and the study of their social conditions are extremely important to fine-tune the measurements of public health in the several levels of prevention (4). For this purpose, it is fundamental to have methods of auditory screening with a sensibility to detect a hearing loss in individuals who do not suspect about having any hearing difficulty and, thus, do not pursue a treatment.
By definition, the screening is applied in a large population, its swiftness and simplicity in its application, and it must identify the individuals having a high likelihood of showing a disorder that is being tested (5). The auditory screening, in turn, must have a high sensitivity and specificity to identify the presence of an auditory alteration when there is really any, as well as have a low cost (6).
The golden test for hearing loss, pure-tone threshold audiometry, requires qualified personnel, acoustic cabin and specific equipment, making it difficult to be performed on a large scale basis. On the other hand, the use of questionnaires with a high sensitivity to indicate hearing loss and that are quickly and cheaply managed, can be a feasible option to screen hearing in large populations (7).
The self-evaluation questionnaires are useful to measure the emotional and social/situational consequences seen as a result of hearing loss, and they can be used in a wide range of situations in the clinical routine, such as auditory screening, first interview, advice, qualification, evaluation, individual's use and satisfaction with the sound amplification equipment and evaluation of the effectiveness of auditory rehabilitation programs (8). The Abbreviated Profile of Hearing Aid Benefit - APHAB, The Nursing Home Hearing Handicap - NHHI, The Hearing Handicap Inventory for the Elderly Screening Version - HHIE-S, The Hearing Handicap Inventory for Adults - HHIA, among others, are questionnaires used for this purpose (9).
Specifically among these questionnaires, the Hearing Handicap Inventory for the Adults Screening Version - HHIA-S and the Hearing Handicap Inventory for the Elderly Screening Version - HHIE-S, which are smaller versions, respectively, of the do Hearing Handicap Inventory for the Adult - HHIA and the Screening Hearing Handicap Inventory for the Elderly - HHIE, are rapidly applied and easily understood, what enables elderly individuals to use them. That is the very reason why the HHIE-S questionnaire is recommended by the American Speech-Language-Hearing Association (ASHA) as an auditory screening tool (8, 10).
Studies performed abroad by STEWART and cooperators in 2002 (10), and by CHANG, HO and CHOU in 2009 (11), researched the validity of the HHIE-S and HHIA-S questionnaires with respect to the perception of hearing loss in the elderly and adults. This study demonstrated that the questionnaires are highly sensitive and specific in the detection of hearing loss in this population.
In Brazil, there are currently some studies (8, 12, 13, 14, 15, 16, 17, 18) showing the usefulness of participation-restricting questionnaires to identify individuals with hearing loss and, in Rio Grande do Sul, the HHIE-S questionnaire was used to evaluate the subjective impact of an auditory rehabilitation program in the elderly (19). On the other hand, there are studies verifying the association between the complaint and the presence of hearing loss in the elderly (20) and showing the prognostic value, sensitivity and specificity of the simple inquiry about the presence of hearing loss (21) in the State of Rio Grande do Sul.
In the first study, individuals answered a demographic questionnaire, in which there was a list of health problems including hearing loss. Out of the 50 participants, both sexes, it was noticed that only 12 (24%) had a specific complaint of hearing loss, although 33 (66%) showed light, moderate, severe and deep hearing loss, and no association between the complaint and the hearing loss was evident. In the second one, with a sample of 795 individuals, both sexes and all age groups, 525 (66%) patients complained about hearing loss, 68 (8.6%) had other auditory complaints, and 202 (25.4%) had no auditory complaint. The results clearly showed that the complaint about hearing loss had a sensitivity of 80.9%, specificity of 69.6%, positive prognostic value of 86.5%, and negative prognostic value of 60.4%.
Nonetheless, the use of more comprehensive participation-restricting questionnaires allows the individual's auditory conditions to be better understood than the mere inquiry about their auditory condition in both adults and elderly.
The present work, thus, had the objective to verify the sensitivity and specificity of the HHIA-S and HHIE-S questionnaires to detect a hearing loss and their applicability in elderly and adult patients' auditory screening based on a sample of individuals served by SUS at the Audiology Department of Hospital Santa Clara's Otorhinolaryngology Ambulatory - Santa Casa de Porto Alegre Hospital Complex. Furthermore, as a secondary objective, the present work attempted to analyze the capacity of the aforementioned questionnaires to detect different degrees of the studied population's hearing impairment.
METHODThis work was approved by Irmandade da Santa Casa de Misericórdia de Porto Alegre (ISCMPA)'s Ethical Committee in Research under a record number 3292/10, dated of May 10, 2010.
Data collection was performed in a period between May and September 2010, three times a week, in the afternoon, and it was a transverse section study. The convenience sample was composed by individuals waiting to perform audiological exams at Hospital Santa Clara's SUS's Otorhinolaryngology Ambulatory - Complexo Hospitalar Santa Casa de Porto Alegre.
To be a part of the sample, participants complied with the following inclusion criteria: be able to read and write, declare to be able and interested in participating in the research and be 18 years old or older. Firstly, patients signed a Free and Clarified Agreement Term, authorizing the data collected in this study to be used, in accordance with the rules established by ISCMPA's Ethical Committee. After signing the term, the individuals above 60 years of age, i.e., considered elderly by the Ministry of Health (20), answered the HHIE-S questionnaire, and the subjects under 60 years of age answered the HHIA-S questionnaire.
The questionnaire Hearing Handicap Inventory for the Elderly Screening Version - HHIE-S was developed by VENTRY and WEINSTEIN (1982) and customized into Portuguese by Wieselberg (1997), and the Hearing Handicap Inventory for Adults Screening Version - HHIA-S questionnaire was translated and customized into Portuguese by Almeida (1998). These tools are comprised of ten questions divided into five items related to social/situation scale and other five corresponding to the emotional scale. These tools are reduced customizations of Hearing Handicap Inventory for the Elderly - HHIE and Hearing Handicap Inventory for the Adult - HHIA, hence they are the only equivalent records to be applied to different populations according to their age group (16). Accordingly, the questionnaires were grouped for data analysis.
The technique chosen to apply the questionnaire was "paper-pencil", i.e., the individual was taught how to read and answer the questionnaire by him/herself. However, it was not possible to use this type of technique with some participants in the sample, thus the "face-to-face" technique was used, i.e., the oral application of the questionnaire by the interview only by reading the items, without further explanations or preparations about them. This was requested or chosen by the individual him/herself in conformity with what was more convenient to him/her at the time of application, usually due to visual or reading difficulties. The participants who answered the "paper-pencil" and "face-to-face" questionnaires were initially analyzed in a separate way.
The likelihood of answers and their score in HHIA-S are identical to those in HHIE-S. Users were asked to answer "yes" (4 points), "sometimes" (2 points) or "no" (no point) for each question according to what they deemed to be more appropriate to their case or situation. The possibility of scores in both questionnaires ranges between 0 (no participation-restricting perception) and 40 (maximum participation restriction). Just like what was proposed by ROSIS, SOUZA and IÓRIO (12), individuals were grouped into three categories: 0-8 points (no participation restriction); 10-23 points (light to moderate restriction) and 24-40 points (significant participation restriction).
Audiometry collection was performed by filling out a questionnaire with the thresholds of frequencies of 250, 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz for airways, and 500, 1000, 2000 and 4000 Hz for bone pathways, in both ears. The audiometric exam was collected in each patient's record, after it has been performed in accordance with the usual procedure of the internship of the Phonoaudiology Degree at UFCSPA at the aforementioned Ambulatory. The equipment used to perform audiometry was Interacoustics AD 227 or Sibelmed AC 50-D.
As to the type of hearing loss, SILMAN e SILVERMAN (22)'s classification about the types of hearing losses as conductive, sensorineural and mixed was used. According to the degree of loss, individuals were classified by taking into consideration the ear with a better hearing, as proposed by LIMA, AIELLO and FERRARI (23), and COSTA, SAMPAIO and OLIVEIRA (24). The best ear was used, because the worst ear tends to be compensated by the function of best size in the subjective perception (7). This classification met BIAP (Bureau Internacional d´Audio Phonologie, 1997) (22)'s requirements, which uses the arithmetic average of answers in audiometric frequencies of 500, 1000, 2000 and 4000Hz and classifies the degrees of hearing loss as: light (21-40dBNA); moderate with a degree I (41-55dBNA); moderate with a degree II (56-70dBNA); severe with a degree I (71-80dBNA); severe with a degree II (81-90dBNA); very I (91-100dBNA); very severe with a degree II (101-110dBNA); very severe with a degree III (111-119dBNA) and total hearing loss/cophosis (above de 120dBNA).
The comparison of the results achieved between the two forms to apply the questionnaires (paper-pencil and face-to-face) was performed by Student's T Test. To verify the association between the variants, the statistical Chi-Square and Fisher's Exact tests were used, the latter of which was used as an alternative to Chi-Square, in case the sample is small in some cells of the crossed table.
For all the aforementioned tests, the maximum assumed significance level was 5% (p<0,05) and the software used for statistical analysis was SPSS version 10.0.
RESULTSSample was comprised of 51 individuals out of whom 49% (n=25) were female and 51% (n=26) were male. Out of the total of study participants, 31,3% (n=16) were aged between 18-39, 29,4% (n=15) were aged between 40-59, and 39.3% (n=20) were 60 years old or older. The observed average age was 52 with a 16.6-year range (standard deviation).
As to questionnaires, 60,7% (n=31) of individuals answered HHIA-S and 39,3% (n=20) answered HHIE-S. When comparing both questionnaires, no statistically significant difference was found between their results (t = 0,22), showing that these records, even in distinct age groups, can be applied for the same purpose.
In relation to the method of questionnaire application, 55% (n=28) of individuals answered in paper-pencil method and 45% (n=23) answered in the face-to-face method. There was no statistically significant difference when comparing the methods of questionnaire application
(t =0,16), so the application methods were grouped for analysis.
When it relates to the type of hearing loss, as SILMAN and SILVERMAN (21)'s classification, 45% (n=23) of the sample showed a sensorineural hearing loss, 11.7% (n=6) conductive hearing loss; 11.7% (n=6), mixed hearing loss, and 31.3% (n=16) showed normal hearing thresholds.
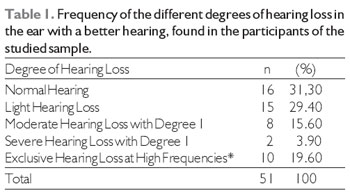
In Table 1, the frequency of the different degrees of hearing loss is introduced, taking into consideration the degree of the best ear, i.e., the one showing the best audiometric score in accordance with the standards suggested by BIAP (21). Accordingly, it was observed that most individuals had a normal hearing (31.3%) and a light hearing loss (29.4%).
When it relates to the answers achieved in the questionnaires, the sample individuals were classified as proposed by ROSIS, SOUZA and IÓRIO (11), and the following results were obtained: 29.4% (n=15) no participation restriction perceived, 29.4% (n=15) light to moderate participation restriction and 41.1% (n=21) significant participation restriction perceived.
The daily audiological evaluation determined the degree and type of hearing loss; applied questionnaires evaluated the degree of participation restriction, i.e., the social and emotional disadvantages as a result of hearing loss in the studied sample. Based on this, the results of the applicability of HHIA-S e HHIE-S tools were surveyed with regard to detecting adults and elderly's hearing loss, as well as their ability to detect different types and degrees of hearing impairment.
In Table 2, an association between the type of hearing loss and the degree of participation restriction is shown. We observed, in this Table, that there was no significant association (p= 0.701) between any kind of hearing loss and the presence of any degree of participation restriction, proving that these questionnaires do not seem to be valid tools to detect different types of hearing loss.
In Table 3, an association between the degree of hearing loss and the degree of participation restriction in the studied sample is shown, as per BIAP's classification (22). Based on the result of Fisher's Exact Test, it is once again observed in this table that there is no significant association between the degree of hearing loss and the degree of participation restriction.
In Graphic 1, the percentage in individuals with and without hearing loss and with and without a participation restriction is indicated. In this graphic, it is possible to observe that 53.3% of the individuals with a hearing disorder and 46.7% of the individuals having no hearing disorder showed no participation restriction; on the other hand, 75% of the individuals with hearing loss and 25% of the individuals without a hearing loss showed a participation restriction. By using Chi Square test, it was possible to observe that there was no significant association between the presence or absence of hearing loss at any degree and the presence or absence of participation restriction
(p= 0.118).
To analyze the validity of HHIE-S and HHIA-S questionnaires regarding their sensitivity and specificity to detect hearing losses and their applicability to screen hearing, it was investigated how many individuals were properly detected with a hearing disorder, considering that the accuracy of a test to properly detect positive patients, i.e., with a disorder, it is called sensitivity and its accuracy to properly detect the negative patients is called specificity (12).
In the studied sample, it was possible to observe that out of the individuals with a normal hearing, 9 had and 7 did not have a participation restriction as a result of hearing disorders that out of the 35 hearing loss participants, 27 showed a participation restriction and 8 showed none. Accordingly, the tools revealed a low sensitivity (47%), i.e., individuals with a hearing loss were not identified; however, they showed a high specificity (75%) by properly identifying the individuals having no hearing disorder.
* No classification found in BIAP (1997)'s suggestion: indicates a presence of average hearing within normal degrees, but the presence of exclusive hearing loss at high frequencies.
The results achieved in the present study demonstrated the presence of a virtually equivalent number of men and women and a higher percentage of adult individuals (60.7%) than elderly (39.3%) in the analyzed sample. It is necessary to emphasize that this sample was conveniently composed by individuals showing previous hearing complaints; hence they had been submitted to an audiological evaluation. Therefore, it is assumed that elderly individuals are served in audiological reference centers other than the ambulatory where the research was performed, since a higher prevalence of hearing loss in the senior years is expected (25).
When comparing the questionnaires, there was no significant difference between their results (t = 0.22). This data was expected, because FREITAS and COSTA (16) claim that these are the only records that are equivalent for application in different populations, in accordance with age groups. When it relates to the application of the aforesaid tools, no difference was evident in both types of application, and such a result was expected because, in another recent research, the application method did not impact the score achieved in a self-evaluation hearing-related questionnaire (26).
As it was verified, sensorineural hearing loss was very prevalent in the studied sample. This result was foreseen because of the number of elderly individuals composing the sample, given that in this population the occurrence of presbycusis is prevalent (25). This finding is also compatible with JARDIM et al's study (27), who equally verified a prevalence of this type of hearing loss in adult and elderly individuals served in the private department of a Brazilian audiological diagnostic center.
The frequency of the different degrees of hearing loss shown in Table 1 revealed a higher number of normal hearing individuals, although some of them have a unilateral hearing loss. It is noticeable that the higher the hearing loss the lower the number of people; such a fact can be explained by progressive losses characterized by presbycusis (25) shown by the elderly individuals in the studied sample.
With regard to the questionnaire answers, most individuals showed a significant participation restriction. This was expected because the population involved in the sample showed previous auditory complaints; hence they mentioned difficulties in accomplishing daily tasks. Another study performed in São Paulo, also in an audiology ambulatory, found similar results in percentages (12).
In Table 2, no statistically significant correlation between any kind of hearing loss and the degree of participation restriction was observed. Still in this Table, it is possible to observe that 23.1% and 26.4% of the individuals with normal auditory thresholds respectively showed a light to moderate perception and a significant participation- restricting perception degree. This finding could be explained by alterations in the auditory processing, because some patients showing audiometry within the normality standards report auditory complaints about speech clearness as a result of the auditory processing disorder (APD), what can place a significant effect over the self-evaluation of the participation-restricting perception (26, 28, 29). Hence, there was a hypothesis that these individuals had no peripheral hearing loss but complaining about social and emotional changes due to hearing disorders would possibly have APD.
Table 3 shows there was no significant association between the degree of hearing loss and the degree of participation restriction (p= 0,705). This finding corroborates with the literature in the works developed by ARAÚJO et al. (30) and ROSIS, SOUZA and IÓRIO (12) who also observed no association, implying that the perception of the hearing disorder was not associated with the degree of the hearing loss.
Besides, the tables shown in Table 2 indicate that individuals with light hearing loss show a higher degree of participation-restricting perception, hence revealing that the degree of hearing loss is not sufficient to prove a restriction in daily tasks because individuals with light, moderate degree I, severe degree I hearing loss and at high frequencies can have different degrees of participation-restricting perception. This result also confirms CORREA and RUSSO (8)'s findings, since, in their research, they verified individuals with light or moderated hearing loss with a higher degree of participation-restricting perception than individuals with higher hearing losses.
In Graphic 1, it is possible to observe that 75% of individuals with a participation-restricting perception showed a hearing loss, and 53.3% of the individuals who did not recognize this restriction also had hearing losses. This may have happened because many individuals answered the questionnaire with the adaptations already in practice in their daily tasks, as mentioned by themselves to researchers during interview. For example, with reference to question 8 of HHIA-S ("Do you have any difficulty in listening to TV or radio because of a hearing disorder?"), some people interviewed answered they had none provided that they would turn up the sound of the equipment.
This study showed that there was no significant association between the presence or absence of any degree of hearing loss and the presence or absence of a participation-restricting perception (p= 0.118). This finding matches that of another study (12), in which there was no statistically significant association between the result found in the audiometry and the perception of participation restriction in the individuals served in the Federal University of São Paulo's Audiology Ambulatory (UNIFESP).
With respect to the sensitivity and specificity to use HHIA-S and HHIE-S questionnaires to detect hearing loss and their applicability on a screening with adults and elderly showing hearing disorders, the study implied that these tools do not seem to be good to detect hearing alterations or screen individuals in audiology services, at which the patients have hearing-related complaints at arrival, resulting in a low sensitivity (47%) and a high specificity (75%). This finding confirms another research(12), in which HHIE-S questionnaire was also applied, found low values for sensitivity (23%) and high values for specificity (73.7%), in the group served in an audiology care center. In this same study (12), for a group served in a non-specific audiology disorder-related center, a high sensitivity (94,7%) and a high specificity (75%) were found, showing that HHIE-S questionnaire can be valid in this type of population as a screening tool. The findings hereof are equally supported by the work performed abroad by GATES et al. (31), who observed such results as 35% and 94 % for sensitivity and specificity, respectively, by using HHIE-S in an elderly population.
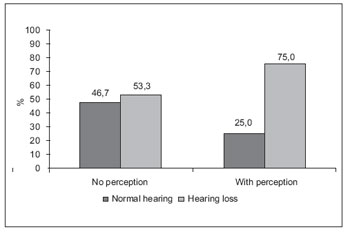
Graphic 1. Percentage of individuals with and without a participation restriction, in accordance with the presence or absence of hearing loss in the studied sample (Chi Square; p=0.118).
In the studied population, the HHIA-S and HHIE-S questionnaires showed a low sensitivity and a high specificity, proving they are not effective tools to screen individuals with previous hearing complaints.
Additionally, in this research, these questionnaires did not show they are efficient to detect different types and degrees of hearing impairment, indicating that the hearing impairment is not necessarily associated with the type or degree of hearing loss.
REFERENCES1. Silva LPA, Queiros F, Lima I. Fatores etiológicos da deficiência auditiva em crianças e adolescentes de um centro de referência APADA em Salvador - BA. Rev Bras Otorrinolaringol. 2006, 72: 33-6.
2. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Portaria SAS/MS 587 de 7 de outubro de 2004 - Determina a organização e a implantação de Redes Estaduais de Atenção à Saúde Auditiva. Brasília (DF): Ministério da Saúde; 2004.
3. Mulrow CD, Aguilar C, Endicott JE, Velez R, Tuley MR, Charlip WS, et al. Association between hearing impairment and the quality of life of elderly individuals. J. Am. Geriatr. Soc. 1990, 38:45-50.
4. Cruz SM, Oliveira LR, Carandina L, Lima MCP, César CLG, Barros MBA et al. Prevalência de deficiência auditiva referida e causas atribuídas: um estudo de base populacional. Cad Saúde Pública. 2009, 25:1123-31.
5. Freitas KC, Calviti K, Pereira LD. Sensibilidade, Especificidade e Valores Preditivos Positivos da Queixa Auditiva Comparados com Diferentes Médias Audiométricas. Rev Bras Otorrinolaringol. 2001, 75:794-800.
6. Freitas CG. A Importância da Imitanciometria na Triagem Auditiva Pré-Escolar. Rio de Janeiro, 1999, p.22 (Monografia de Especialização em Audiologia Clínica .Centro de Especialização em Fonoaudiologia Clínica - CEFAC).
7. Rosalino CV, Rozenfeld S. Triagem auditiva em idosos: comparação entre auto-relato e audiometria. Rev Bras Otorrinolaringol. 2005, 71:193-200.
8. Correa GF, Russo IC. Autopercepção do Handicap em Deficientes Auditivos Adultos e Idosos. Rev CEFAC. 1999, 1:54-63.
9. Macedo LS, Pupo C, Balieiro, CR. Aplicabilidade dos Questionários de Auto-avaliação em Adultos e Idosos com Deficiência Auditiva. Rev Dist Comum. 2006, 18:19-25.
10. Stewart M, Pankiw R, Lehman ME, Simpson TH Hearing Loss and Hearing Handicap in Users of Recreational Firearms. J Am Geriatr Soc. 2002, 13:160-8.
11. Chang HP, Ho CY, Chou P. The Factors Associated with a Self-Perceived Hearing Handicap im Elderly People with Hearing Impairment - Results from a Comunity - Based Study. Ear Hear. 2009, 30:576-583.
12. Rosis AC, Souza MR, Iório MC. Questionário Hearing Handicap Inventory for the Elderly - Screening Version (HHIE-S): estudo da sensibilidade e especificidade. Rev Soc Bras Fonoaudiol. 2009, 14:339-45.
13. Santiago LM, Novaes CD. Auto-Avaliação da Audição em Idosos. Rev CEFAC 2009, 11:98-105.
14. Calviti KCFK, Pereira LD. Sensibilidade, especificidade e valores preditivos da queixa auditiva comparados com diferentes médias audiométricas. Rev Bras Otorrinolaringol. 2009, 75:794-800.
15. Carvalho RD, Iório MC. Eficácia da Aplicação do Questionário de Handicap em Idosos Deficientes Auditivos. Rev Disturb Comum. 2007, 19:163-72.
16. Freitas CD, Costa MJ . Processo de Adaptação de Próteses Auditivas em Usuários Atendidos em uma Instituição Pública Federal - Parte II: resultados dos questionários de auto-avaliação. Rev Bras Otorrinolaringol. 2007, 73:660-70.
17. Lautenschlager L, Tochetto T, Gonçalves MS, Barreto DCM, Moro MP, Bolzan GP. Percepção de Idosos Socialmente Ativos quanto às Desvantagens Causadas pela Dificuldade Auditiva. Rev Einstein. 2008, 6:155-58.
18. Teixeira AR, Freitas CLRF, Millão LF, Gonçalves AK, Junior BB, Santos AMPV, et al. Relação entre a Queixa e a Presença de Perda Auditiva entre Idosos. Arq Int Otorrinolaringol. 2009, 13:78-82.
19. Angeli RD, Jotz GP, Barba MC, Demeneghi PGM, Mello CHP. Efetividade de um Programa de Protetização Auditiva em Idosos Através da Aplicação do Questionário HHIE-S. Arq Int Otorrinolaringol. 2009, 13:277-80.
20. Marini ALS, Halpern R, Aerts D. Sensibilidade, Especificidade e Valor Preditivo da Queixa Auditiva. Rev Saúde Pública. 2005, 39:982-84.
21. Lei N. 8.842, de 4 de Janeiro de 1994. Ministério da Saúde.
22. Conselhos Federal e Regional de Fonoaudiologia. Orientações dos Conselhos de Fonoaudiologia para o Laudo Audiológico. 2009, 8-11.
23. Lima II, Aiello CP, Ferrari DV. Correlações Audiométricas do Questionário de Handicap Auditivo para Adultos. Rev CEFAC. 2010, 12:1-1.
24. Costa MHO, Sampaio ALL, Oliveira CACP. Avaliação do Benefício da Prótese Auditiva Digital e da Percepção da Desvantagem Auditiva ou "Handicap" em Idosos não Institucionalizados. Arq Int Otorrinolaringol. 2007, 11:159-68.
25. Nóbrega JD, Câmara MFS, Borges ACC. Audição do Idoso: Análise da Percepção do Prejuízo Auditivo, Perfil Audiológico e suas Correlações. Rev Bras Prom Saúde. 2008, 21:39-46.
26. Marotta RMB, Quintero, SM, Marone SAM. Avaliação do processamento auditivo por meio do teste de reconhecimento de dissílabos em tarefa dicótica SSW em indivíduos com audição normal e ausência do reflexo acústico contralateral. Rev Bras Otorrinolaringol. 2002, 68:254-61.
27. Jardim IS, Iwahashi JH, Paula VC. Estudo do Perfil Audiológico de Indivíduos Atendidos em um Serviço de Diagnóstico Brasileiro. Arq Int Otorrinolaringol. 2010, 14: 32-37.
28. Quintero SM, Marotta RMB, Marone SAM. Avaliação do processamento auditivo em idosos com e sem presbiacusia por meio do teste de reconhecimento de dissílabos em tarefa dicótica - SSW. Rev Bras Otorrinolaringol. 2002, 68(1):28-33.
29. Fire KM, Lesner SA, Newman C. Hearing handicap as a function of central auditory abilities in the elderly. Am J Otol. 1991, 12:105-08.
30. Araújo P G V, Mondelli MFCG, Lauris JRP, Richiéri AC, Feniman MR. Avaliação do handicap auditivo do adulto com deficiência auditiva unilateral. Braz J Otorhinolaryngol. 2010, 6:370-83.
31. Gates G A, Murphy M, Rees TS, Fraher A. Screening for handicapping hearing loss in the elderly. J F Pract. 2003, 52:56-62.
1) Doctor in Human Communication Disorders from the Federal University of São Paulo. Professora at UFCSPA's Phonoaudiology Department.
2) Taking Doctorate Degree in Biomedical Gerontology (PUCRS). Professora at UFCSPA's Phonoaudiology Department.
3) Taking Specialization Degree in Orofacial Motricity at CEFAC-RS. Clinical Phonoaudiologist.
4) Taking Master Degree in Rehabilitation Sciecnce at UFCSPA's PPG. Taking Master Degree in Rehabilitation Sciecnce at UFCSPA's PPG.
Institution: Federal University of Health Sciences in Porto Alegre. Porto Alegre / RS - Brazil. Mailing address: Tanise Cristaldo Anhaia - Rua Duque de Caxias, 203/22 - Porto Alegre / RS - Brazil - ZIP Code: 90010-282 - Telephone: (+55 51) 9287-4589 - Email: tanise.anhaia@bol.com.br
Article received on March 25, 2011. Article approved on April 19, 2011.